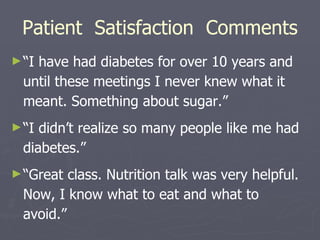
The study evaluated whether diabetic patients who regularly attend group medical visits for 6 months would show improvements in metabolic parameters and diabetes knowledge compared to traditional individual visits. The group visits included education, medical evaluation, and coordination of care. Results showed statistically significant improvements in HbA1c, diabetes knowledge, weight, blood pressure, and patient satisfaction for those in the group visit model. The study concluded that group visits can empower diabetics to better self-manage their condition through lifestyle changes.