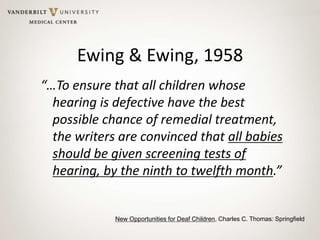
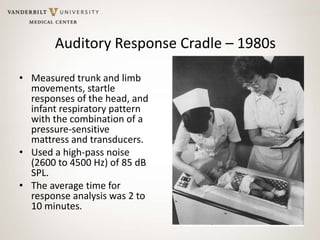
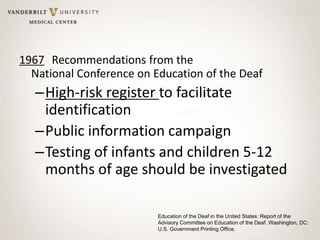
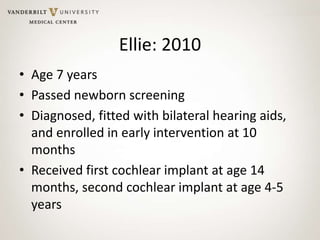
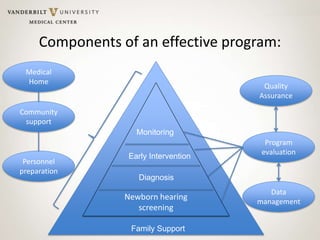
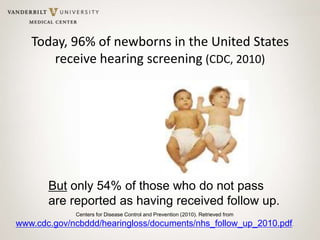
This document summarizes the history of newborn hearing screening and intervention from the mid-20th century to present day, and outlines a charge for further progress. Key points include: screening began in the 1960s/70s using crude methods; recommendations in the 1960s paved the way for universal screening; improvements in technology enabled widespread newborn screening by 2000s; while screening coverage is now 96%, only 54% of infants who don't pass receive follow-up; the document calls for expanding teleaudiology, screening for etiologies, preventing hearing loss, and personalized intervention to help all children access services.