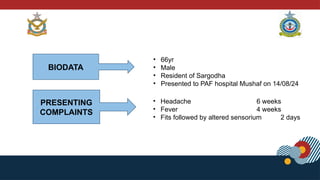
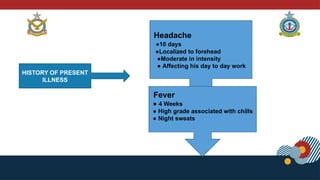
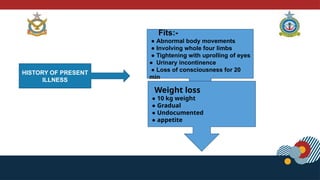
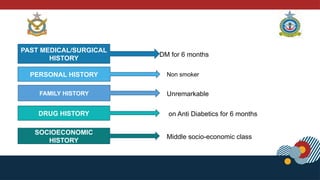
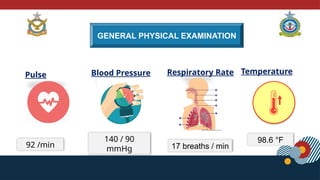
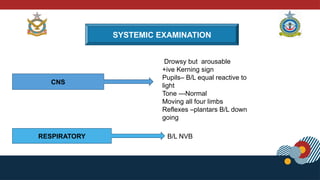
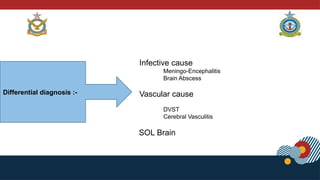
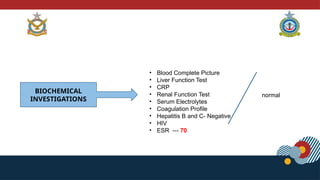
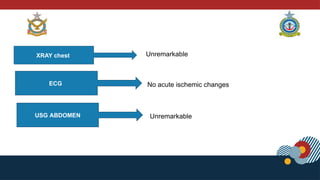
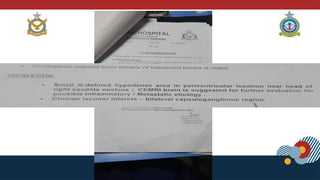
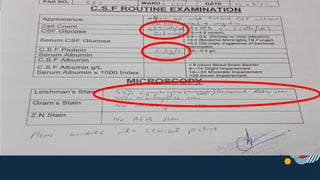
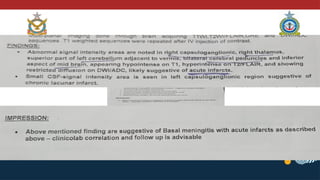
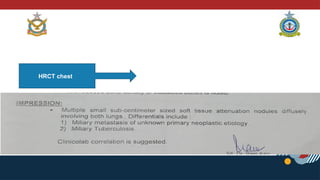
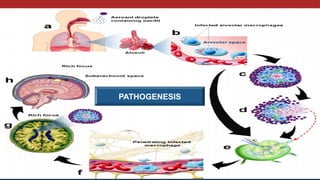
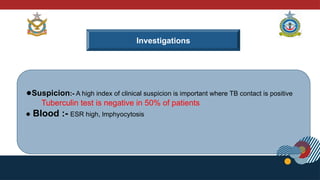
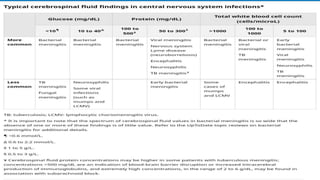
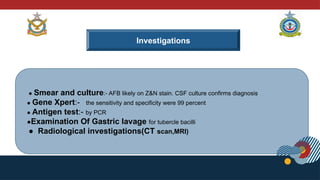
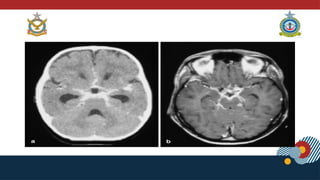
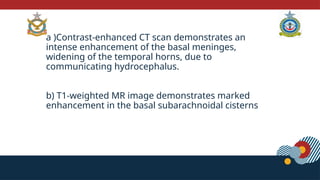
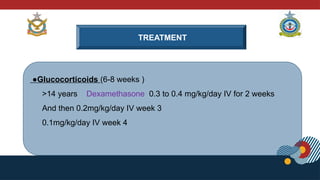
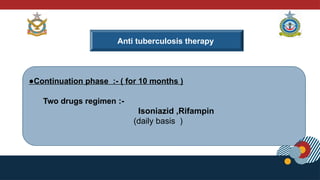
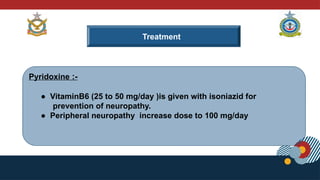
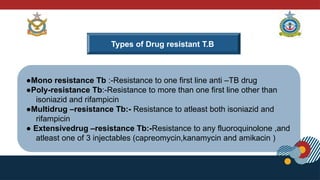
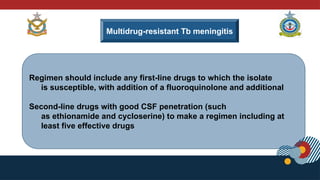
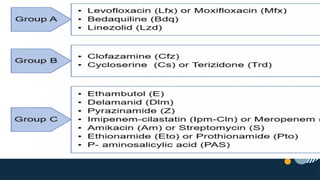
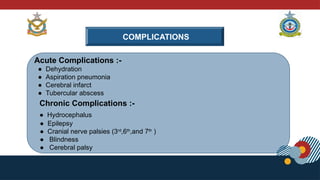
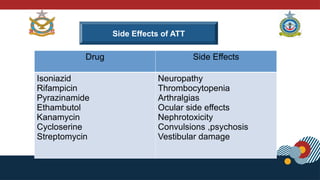
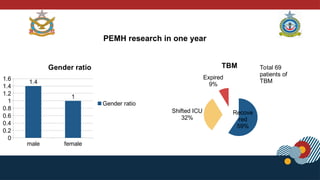
The document presents a detailed case study of a 66-year-old male with fever, headache, and altered sensorium, ultimately diagnosed with disseminated tuberculous meningitis (TBM). It outlines his medical history, clinical symptoms, diagnostic tests, and treatment regimen, highlighting the importance of early intervention and a high index of clinical suspicion for TBM, which can lead to significant neurological sequelae if untreated. The literature review notes recovery rates and outcomes for TBM cases at PAF Hospital Mushaf, emphasizing the critical role of effective therapy and monitoring.