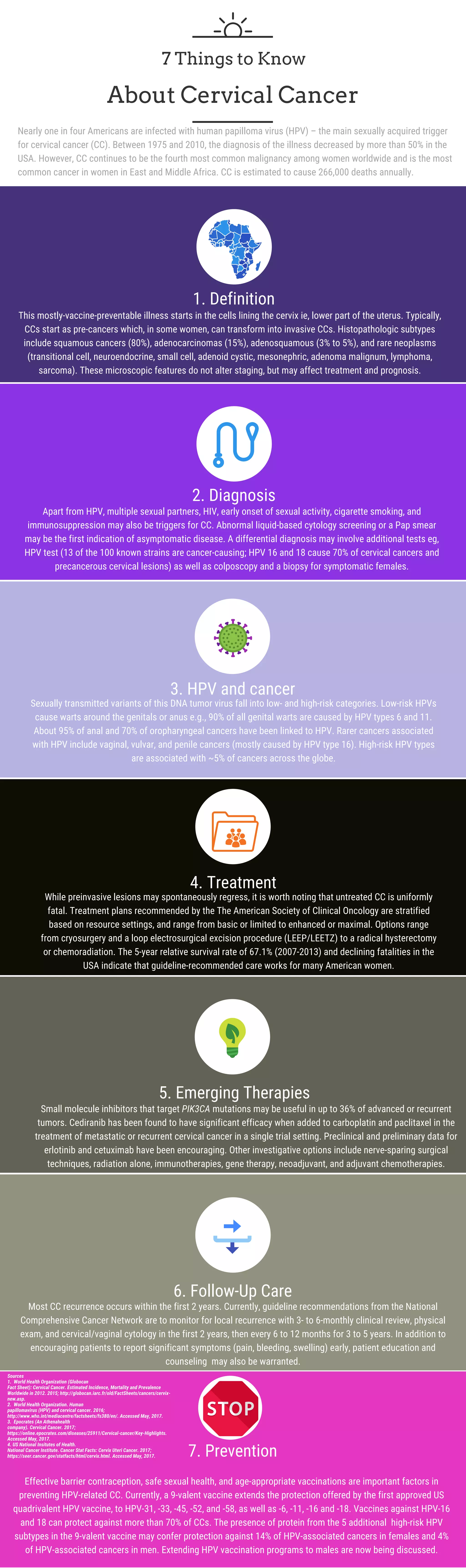
Human papilloma virus (HPV) affects nearly 25% of Americans and is a key trigger for cervical cancer (CC), which remains a leading cancer among women globally. Diagnosis often involves cytology screenings and HPV testing, while treatment options vary from surgery to chemoradiation, with a 5-year survival rate of approximately 67.1%. Prevention through vaccination and safe sexual practices is critical, as a 9-valent vaccine can protect against multiple high-risk HPV types associated with CC.