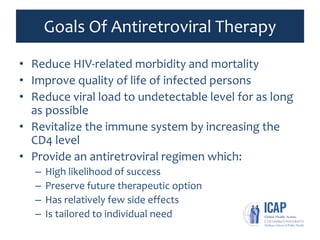
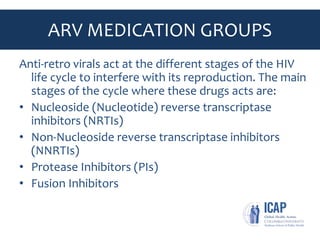
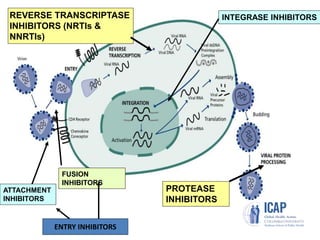
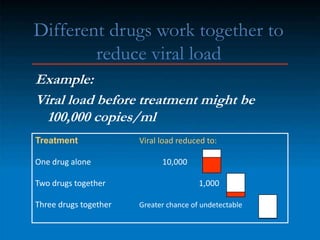
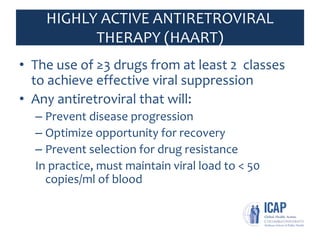
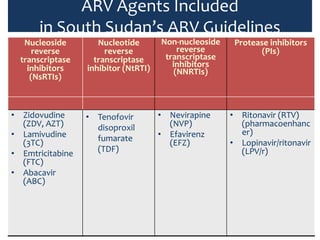
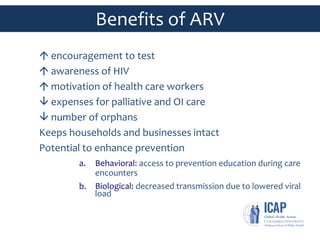
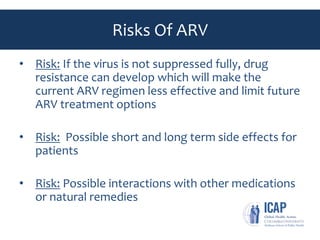
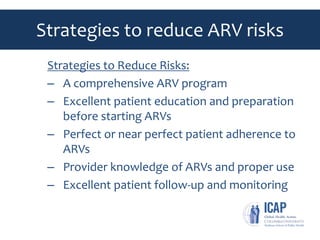
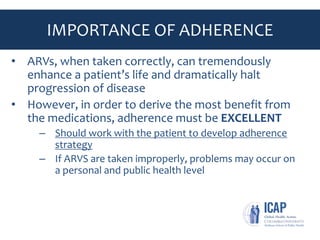
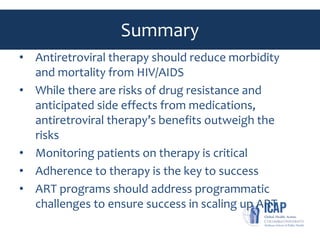
Antiretroviral therapy (ART) aims to suppress the HIV virus and improve health outcomes. It works by targeting different stages of the HIV lifecycle using combinations of antiretroviral drugs from several classes. Regular monitoring of viral load and CD4 levels helps assess treatment effectiveness and risk for disease progression. While ART has significant benefits if taken correctly, non-adherence risks developing drug resistance and limiting future treatment options. Ensuring strong patient education and support for following complex drug regimens is essential for ART programs to successfully reduce HIV-related morbidity, mortality and transmission at population levels.