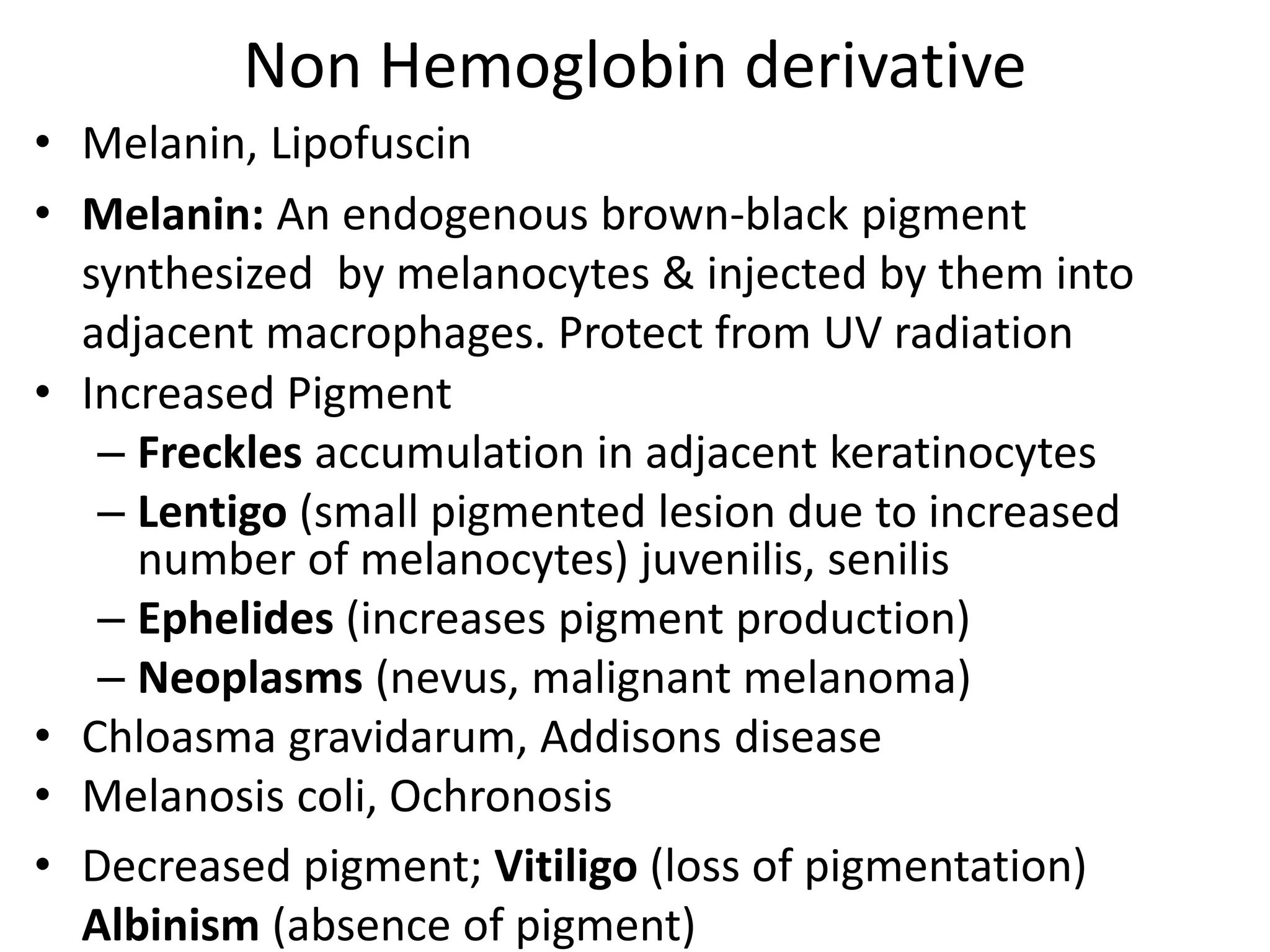
The document discusses intracellular accumulations, highlighting the abnormal buildup of various endogenous and exogenous substances in tissues, which can have either harmless or toxic effects. It outlines four pathways of such accumulations, including inadequate removal of normal substances, accumulation due to defects in metabolism, and the failure to degrade metabolites. The document also covers various types of accumulations like fatty change in the liver, protein accumulation, pigments, and pathologic calcification, detailing their morphology, causes, and potential consequences.