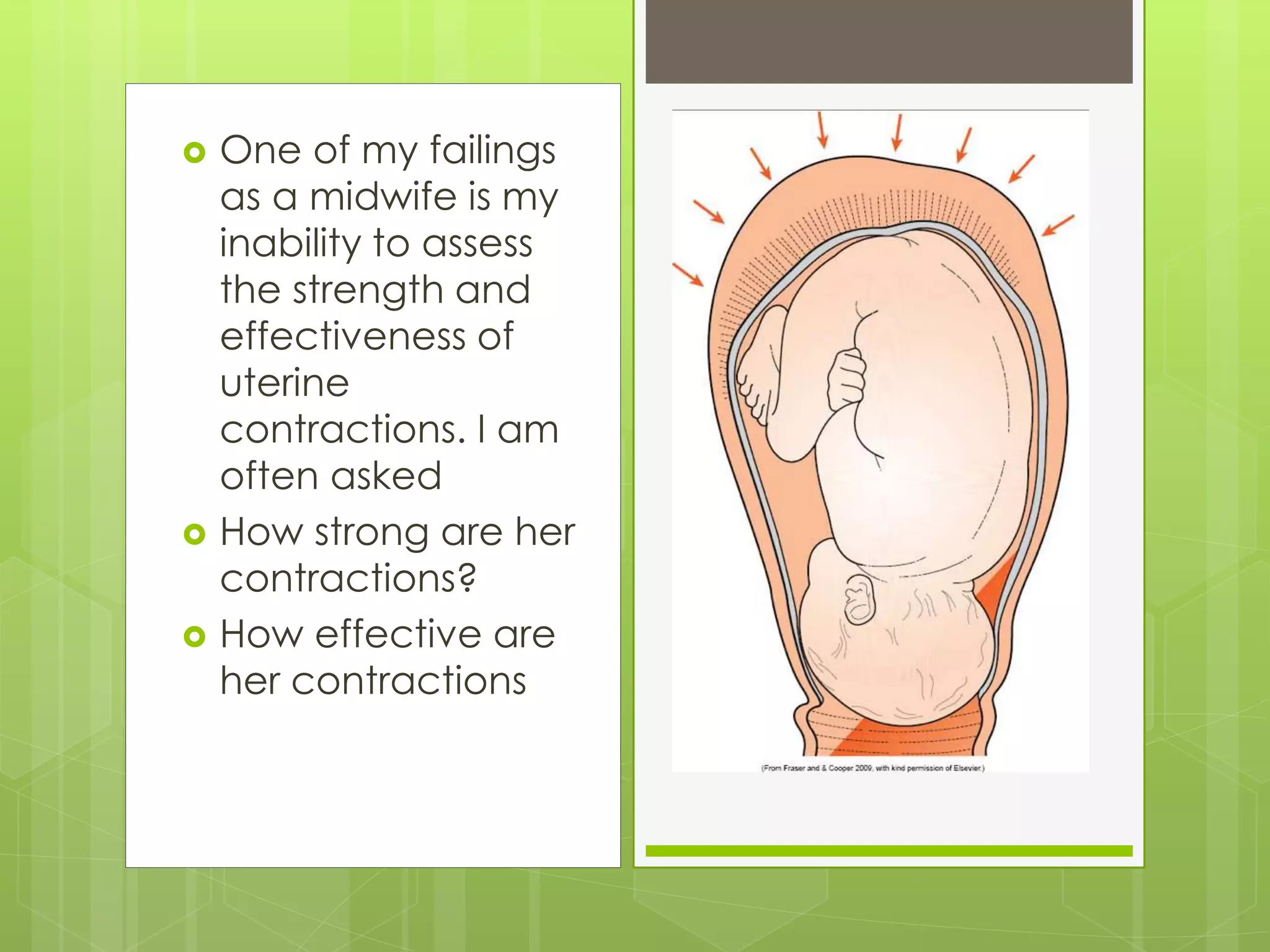
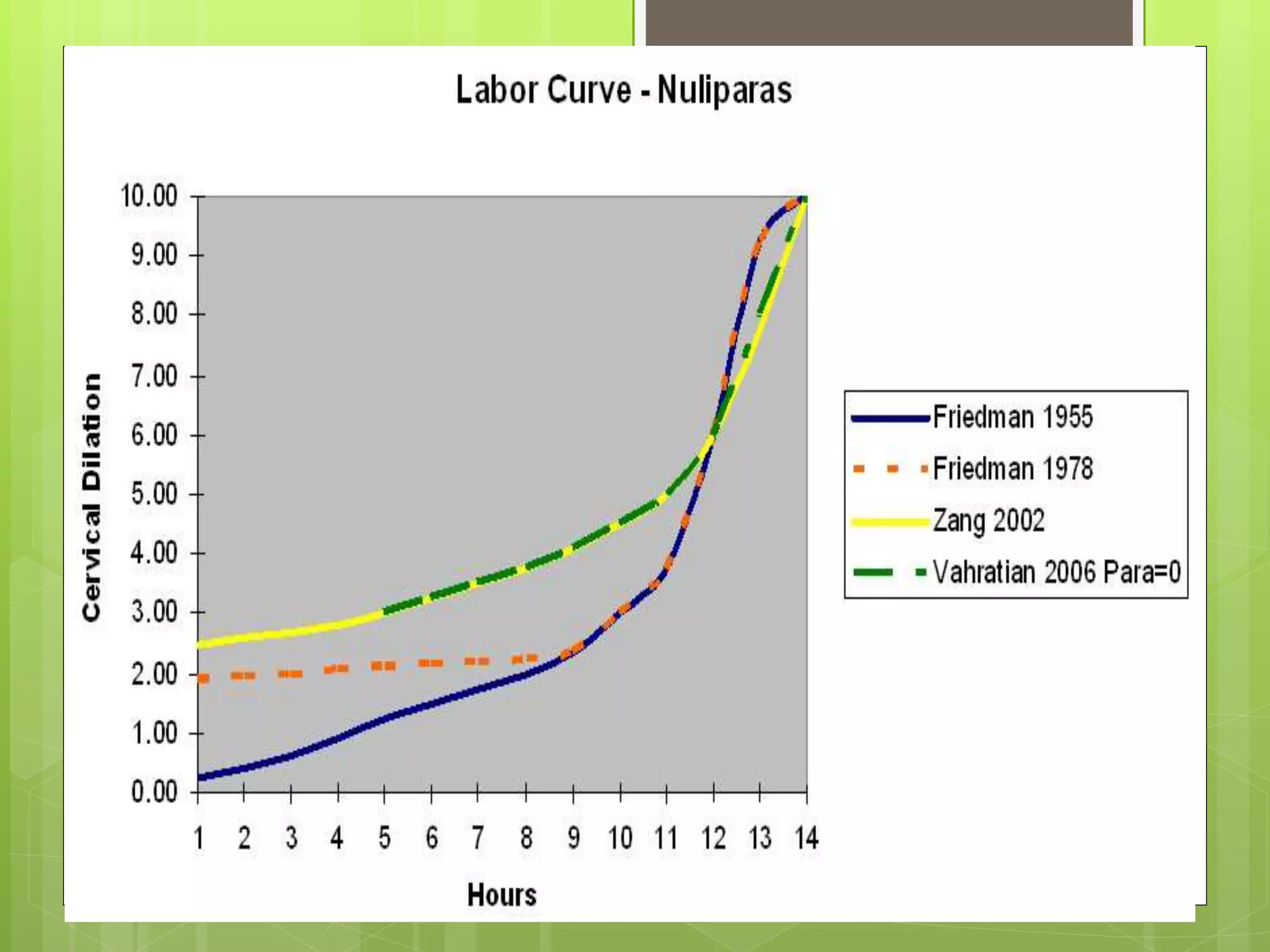
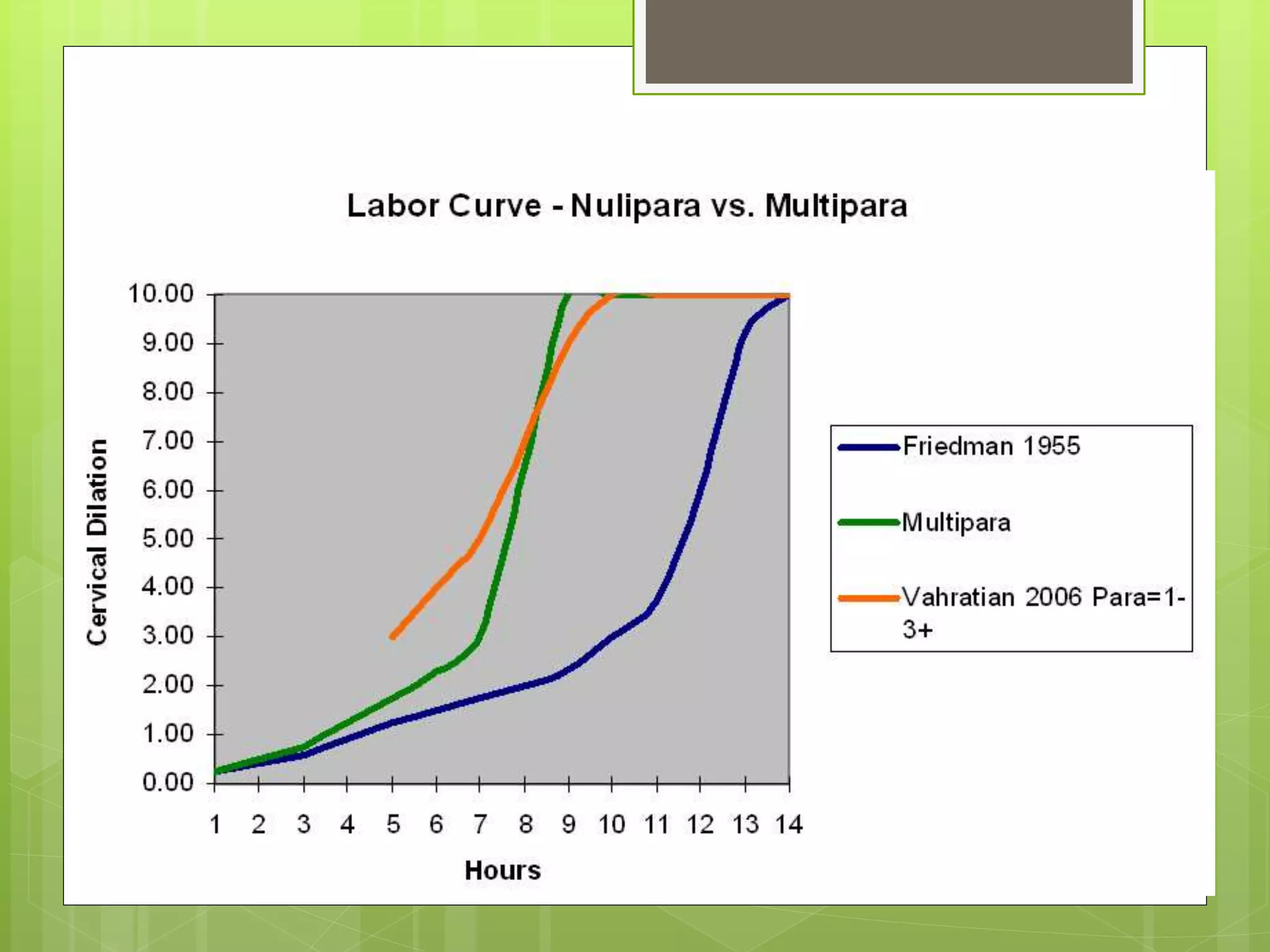
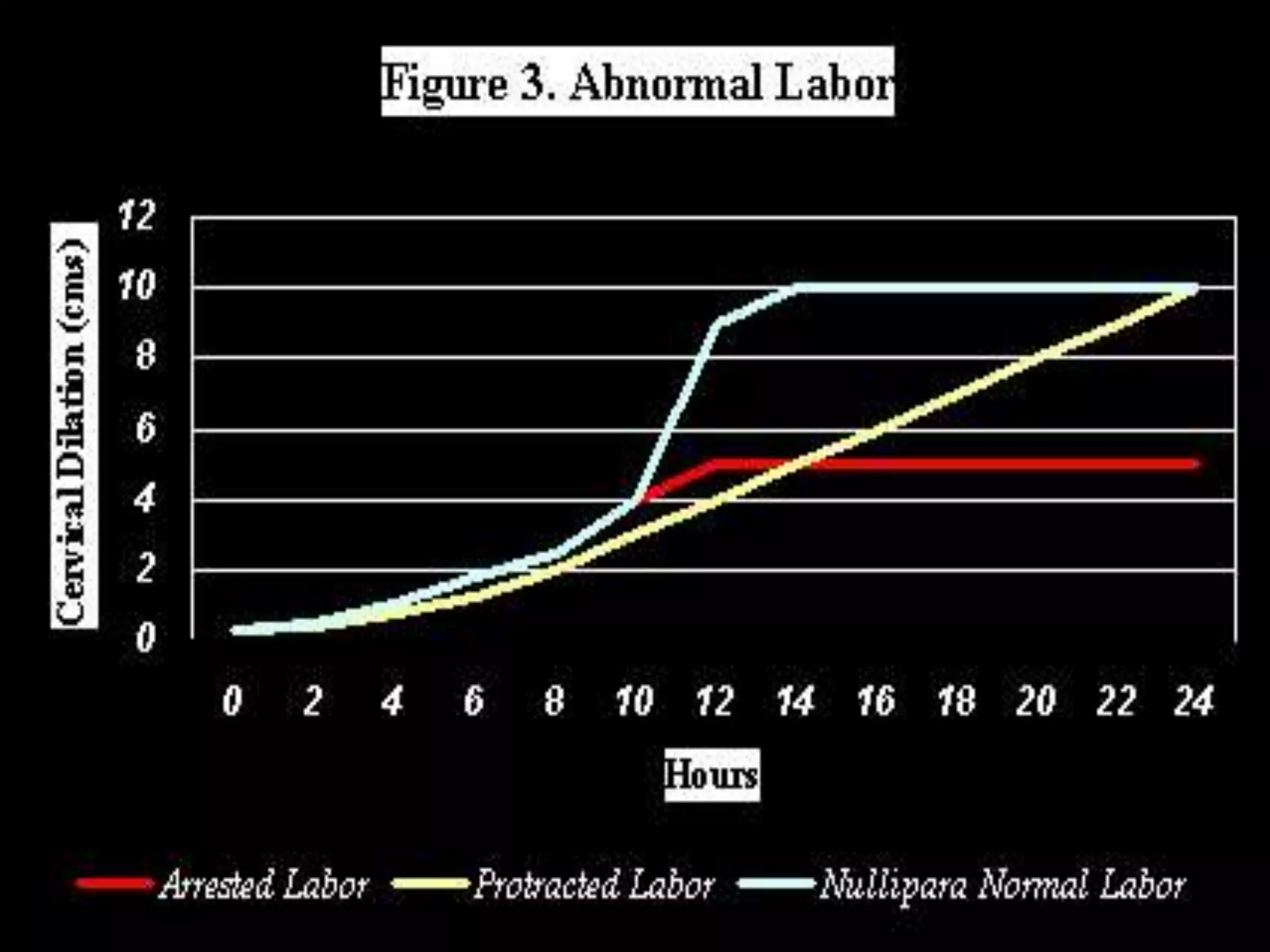
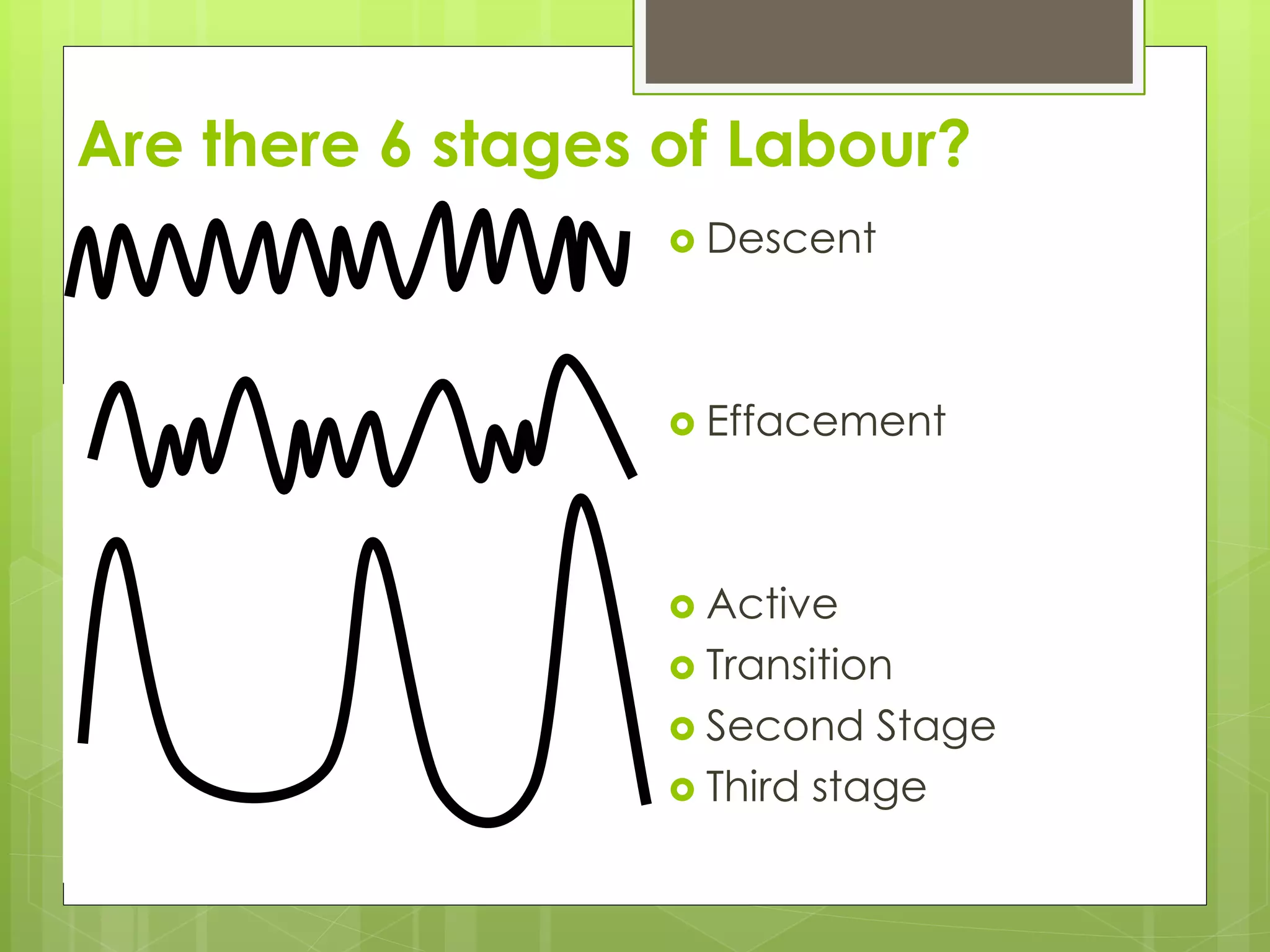
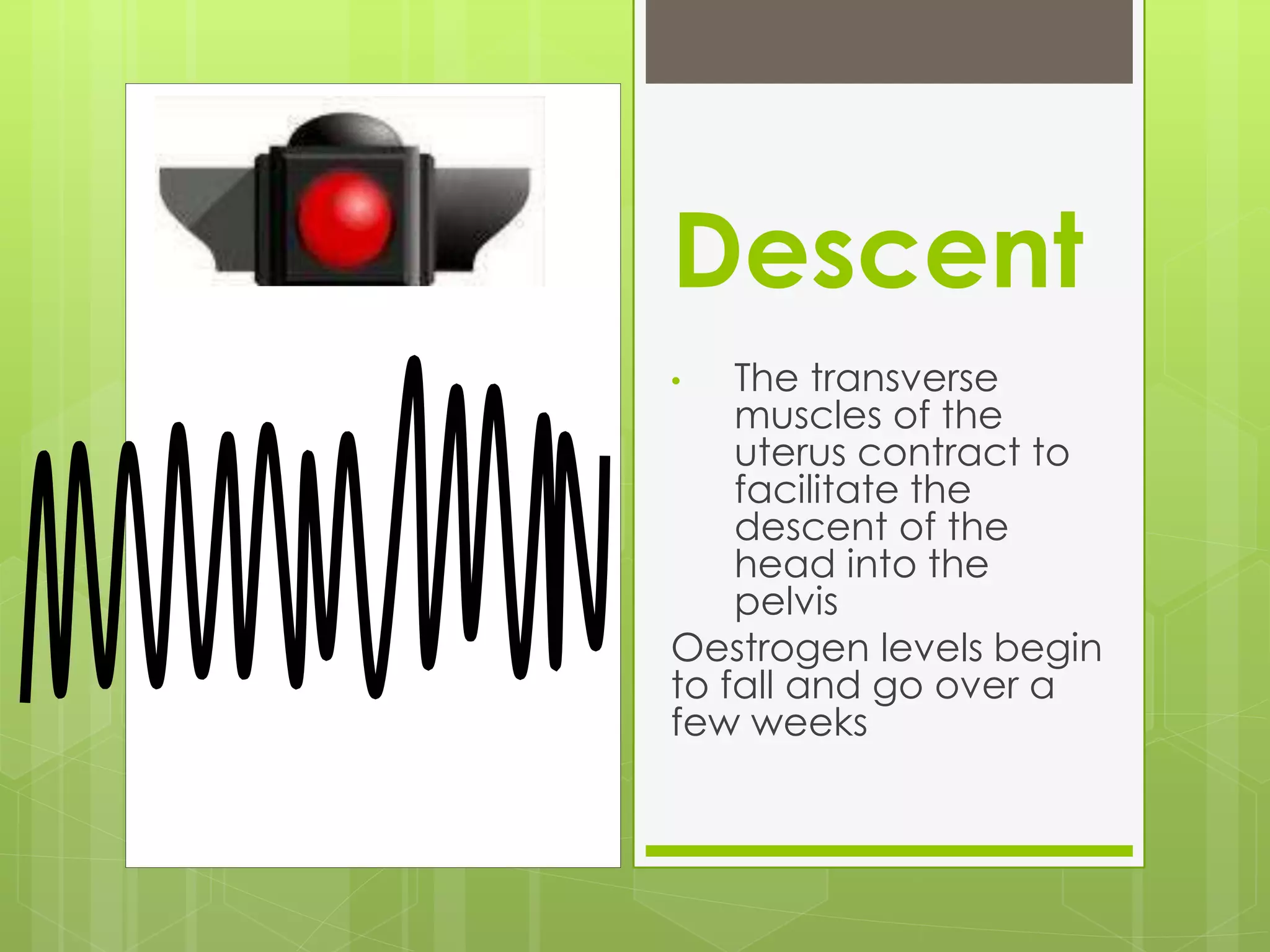
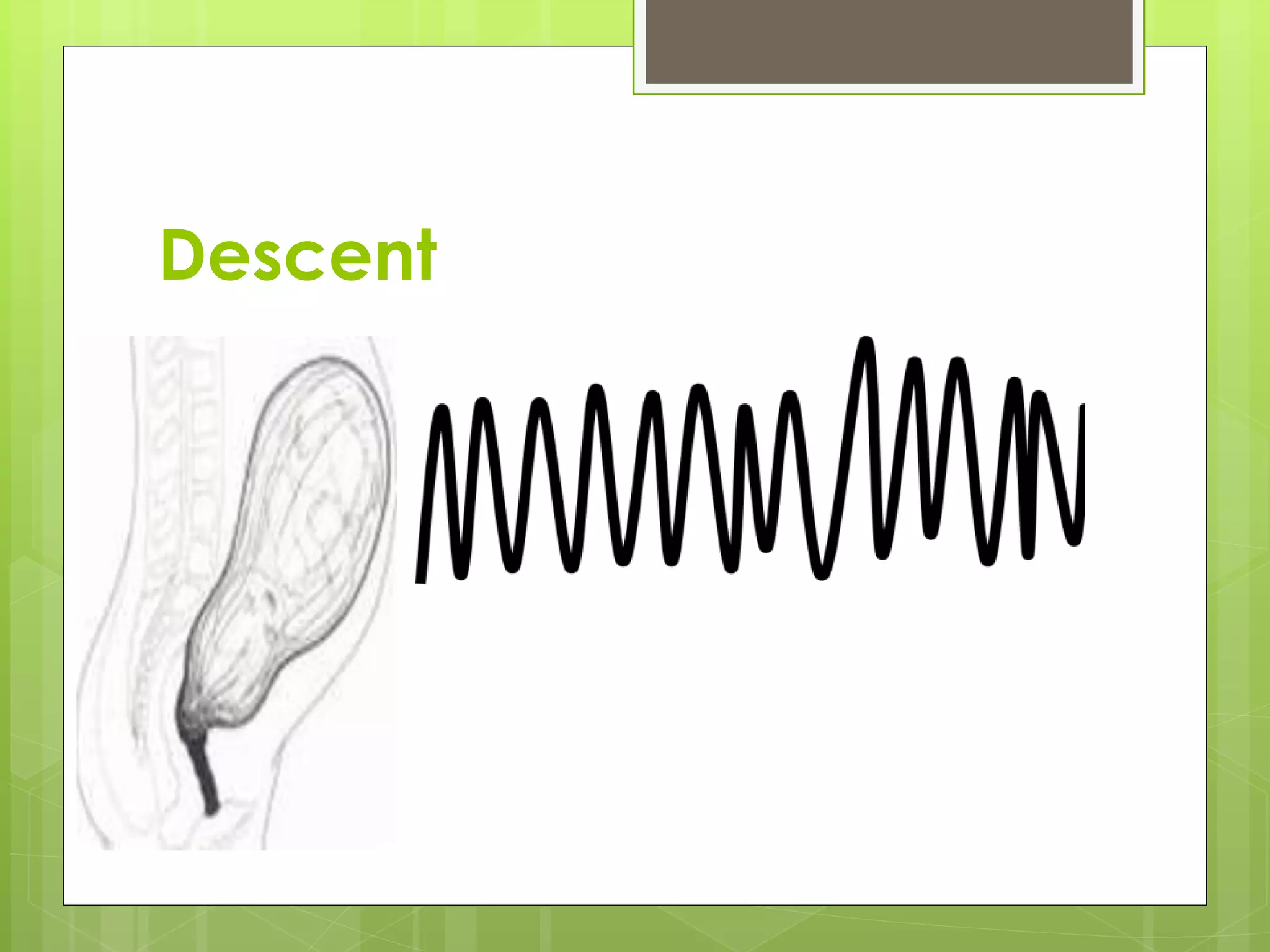
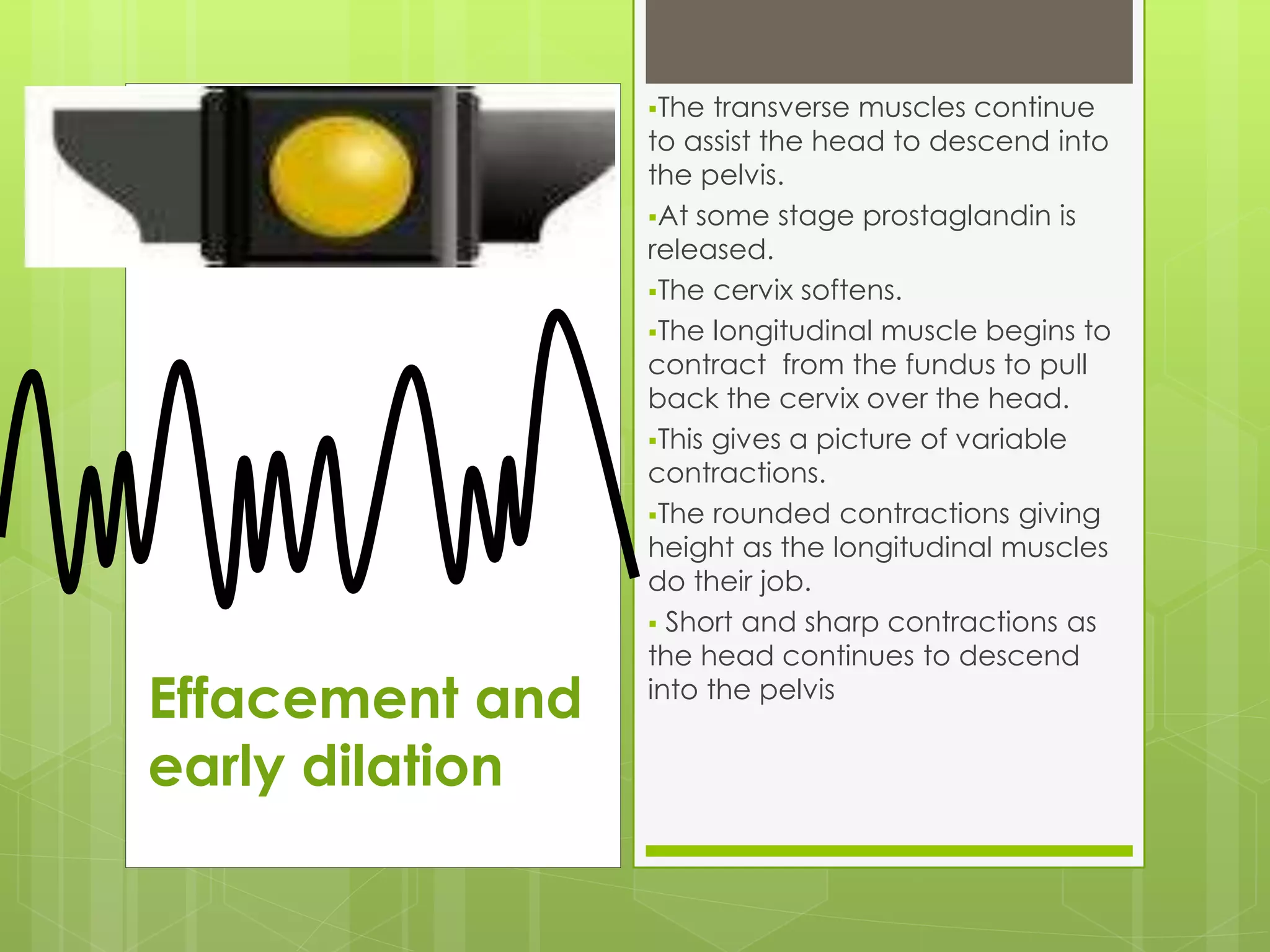
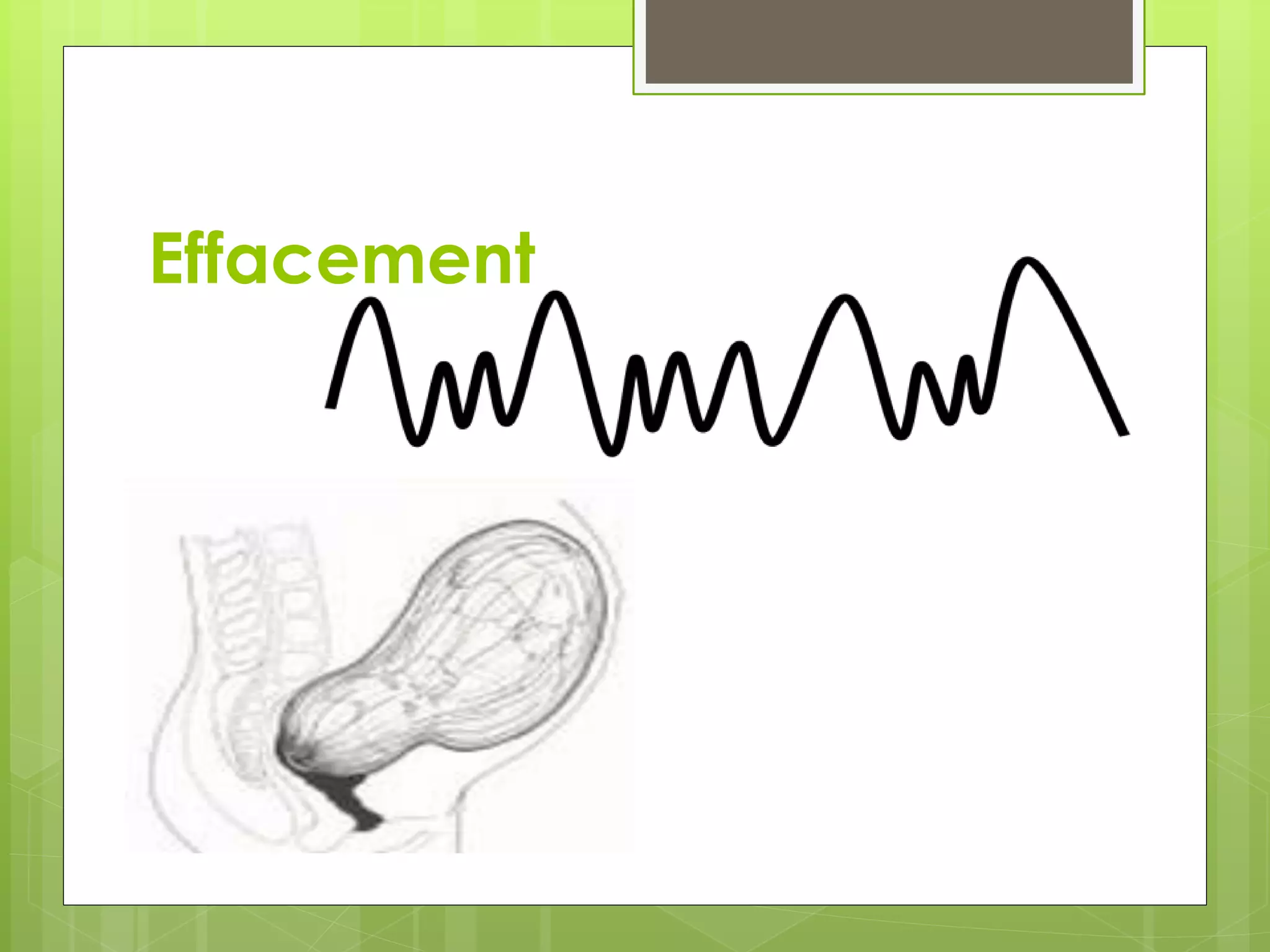
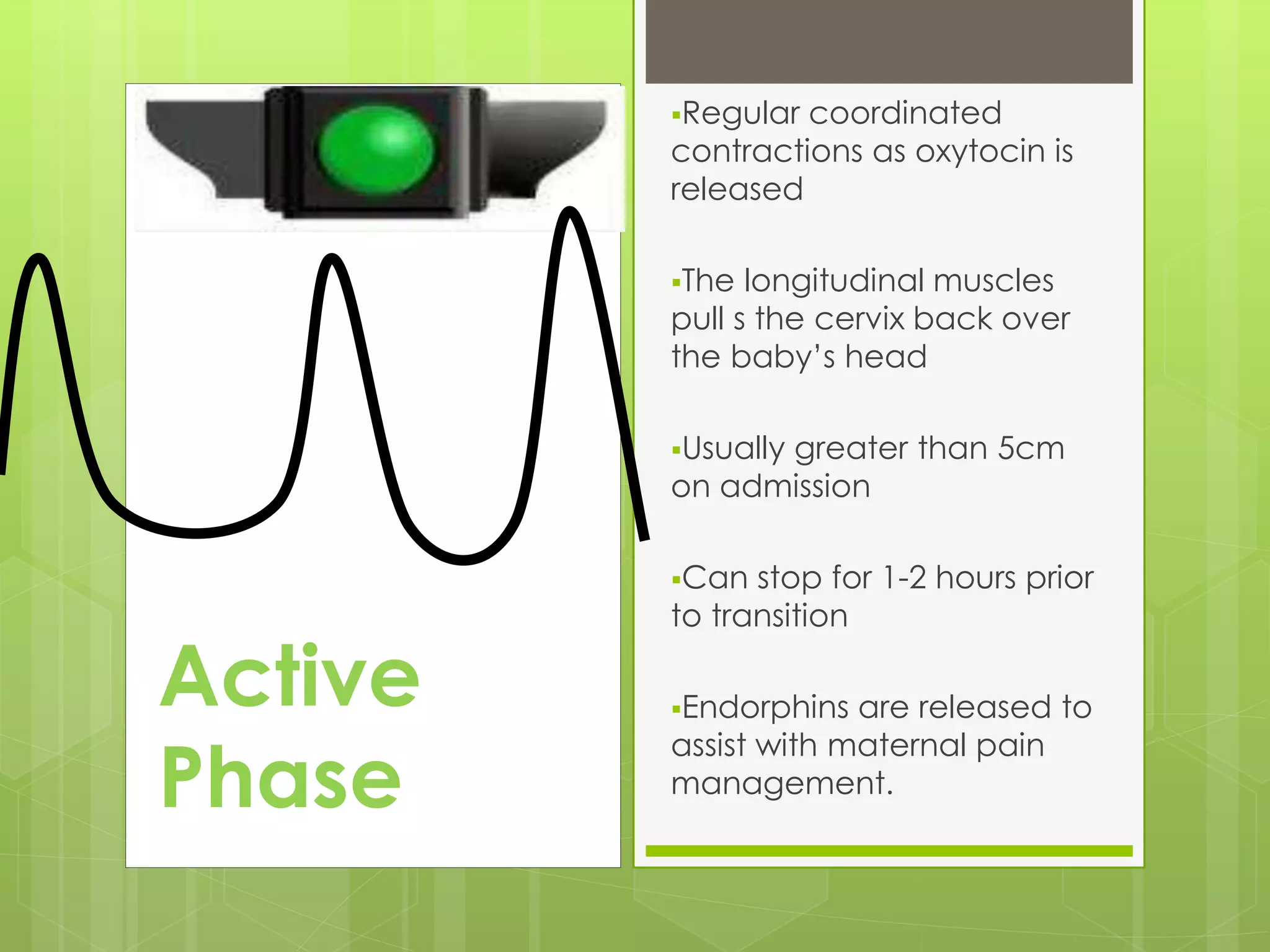
The document discusses how understanding the normal physiological processes of labour, including the contraction patterns and stages of labour, can help midwives support vaginal births and avoid unnecessary interventions. It emphasizes applying anatomy and physiology to assess each woman's individual situation based on factors like baby positioning and dilation. Recognizing the full spectrum of labour from latent to active phases and using non-medical approaches can result in higher rates of normal birth.