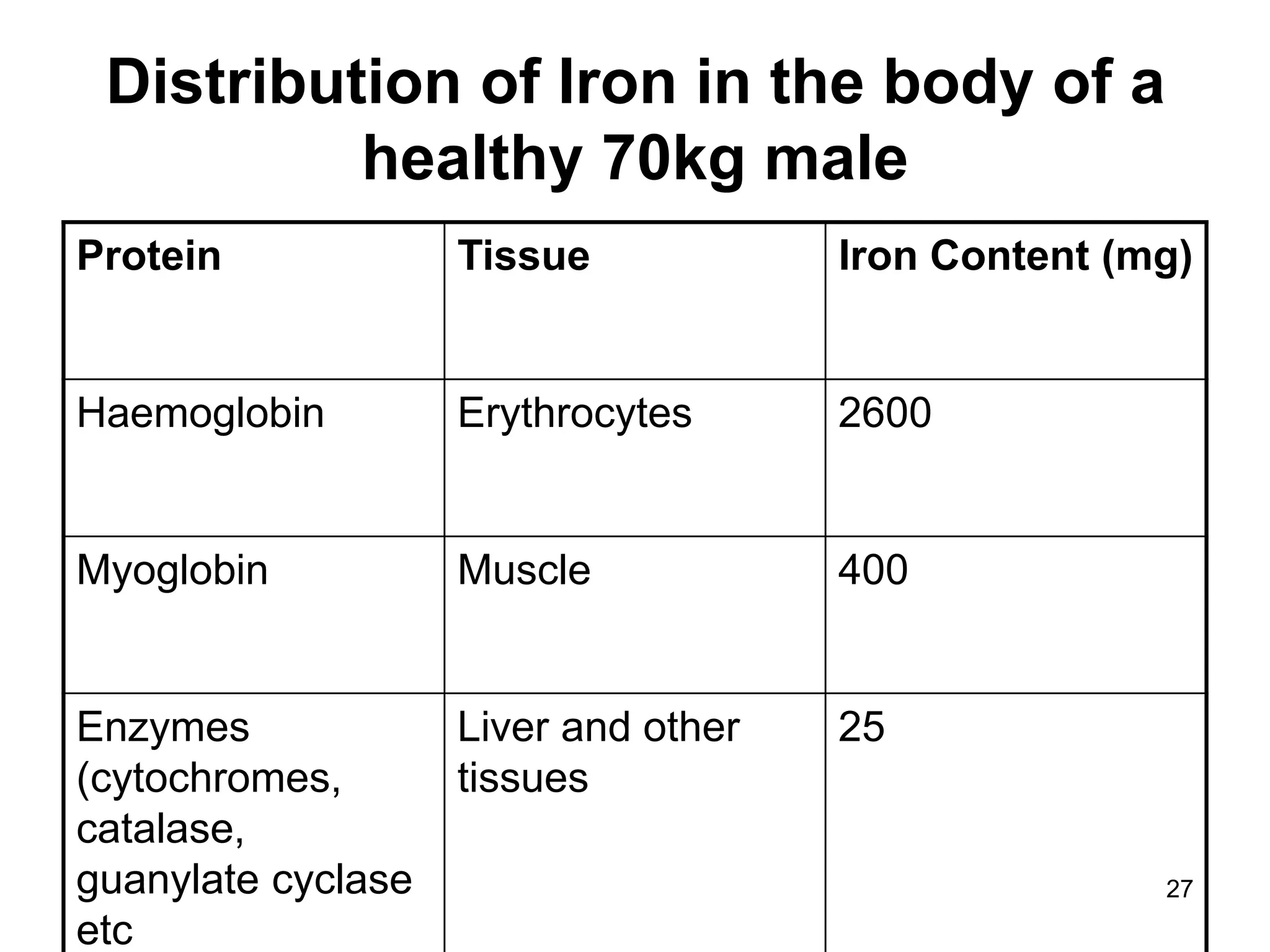
Iron, vitamin B12, and folic acid are important haematinic agents used to treat different types of anaemia. There are two main types of anaemia - iron deficiency anaemia, which occurs due to blood loss or malabsorption of iron, and megaloblastic anaemia, which can be caused by deficiencies in vitamin B12 or folic acid due to problems with absorption or diet. Haematinic agents work to treat the underlying cause of anaemia and help increase red blood cell production by providing the necessary nutrients.