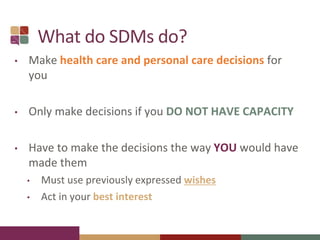
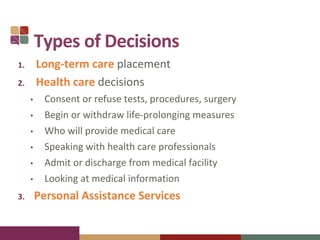
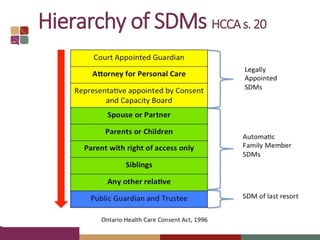
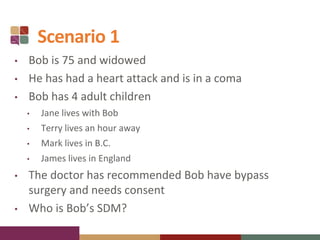
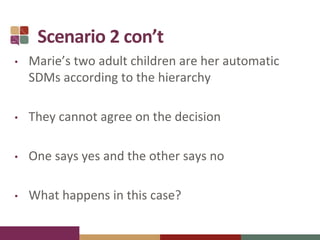
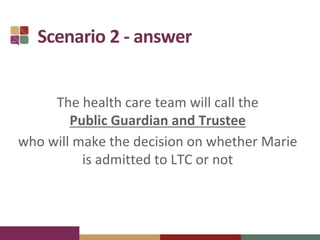
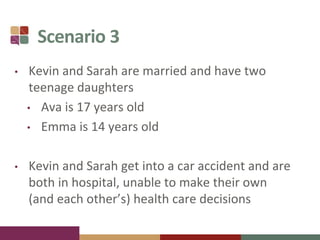
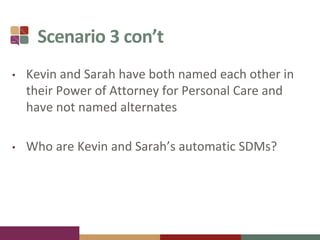
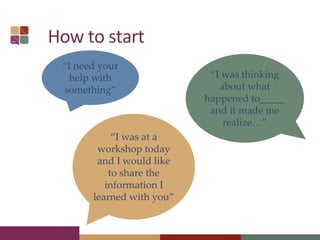
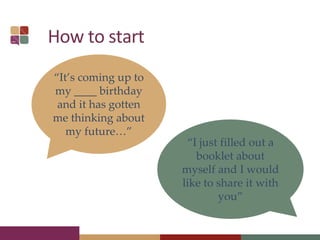
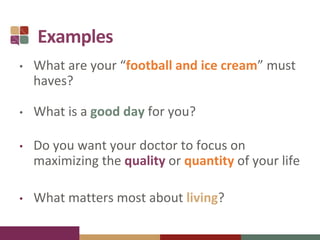
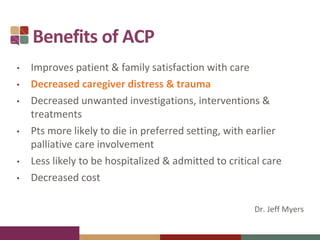
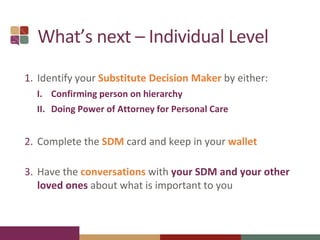
This document provides information about advance care planning in Ontario. It discusses identifying a substitute decision maker who can make healthcare decisions if someone is unable to speak for themselves. It provides scenarios to illustrate how substitute decision makers are determined. It emphasizes the importance of having conversations with one's substitute decision maker and loved ones to communicate what is important to an individual in terms of their healthcare values and priorities. The benefits of advance care planning include improved care experiences and outcomes. Resources are provided to help individuals engage in advance care planning.