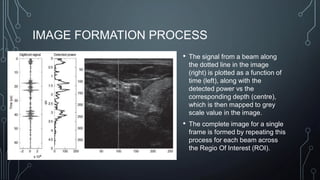
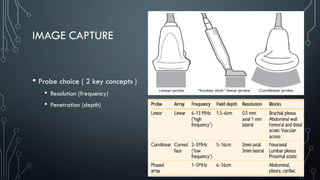
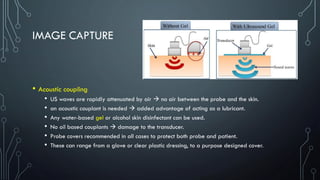
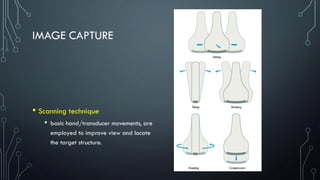
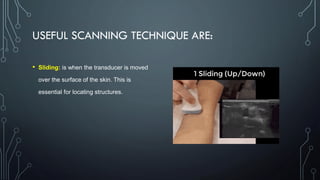
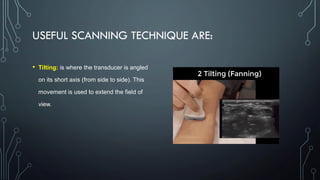
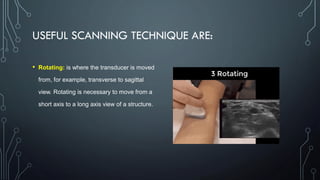
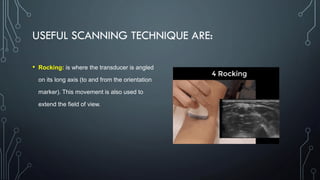
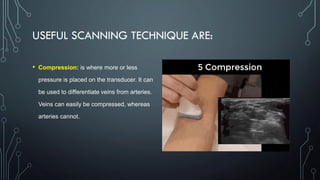
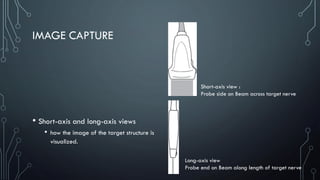
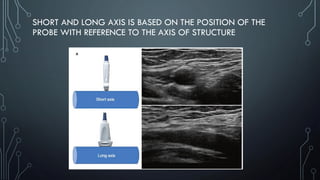
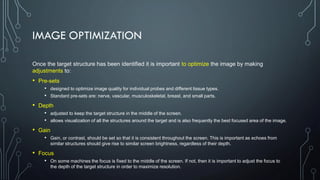
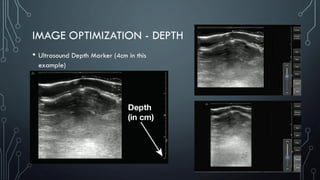
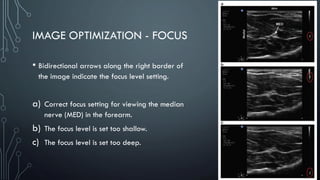
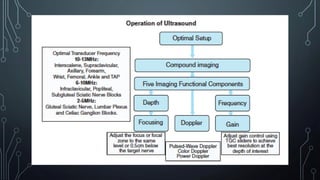
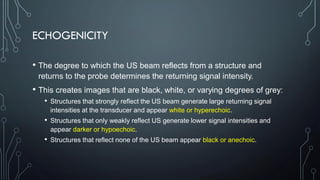
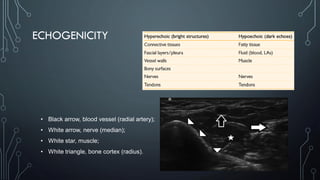
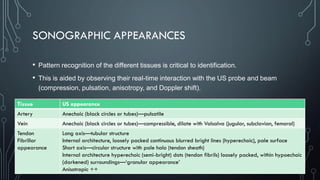
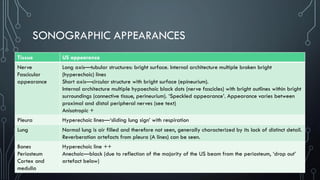
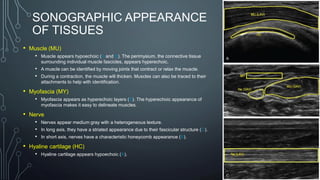
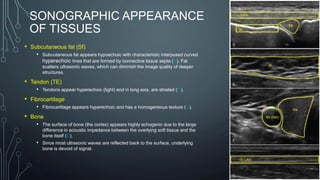
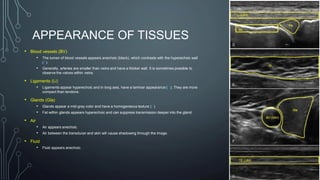
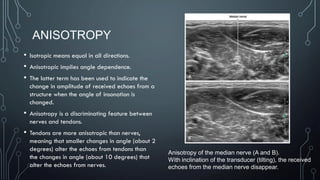
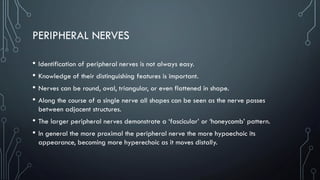
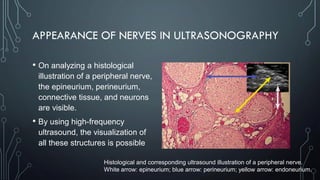
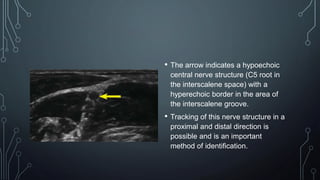
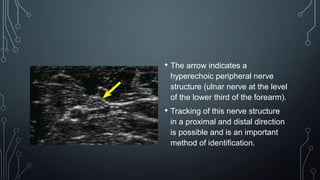
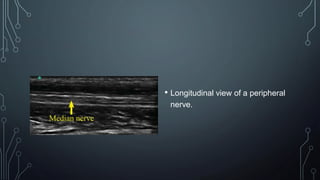
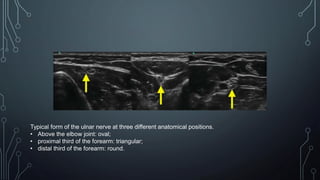
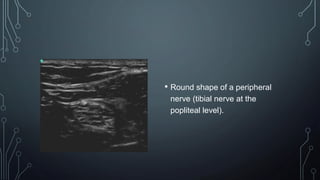
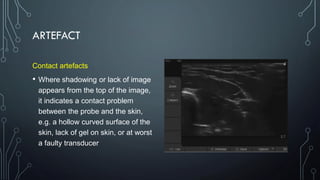
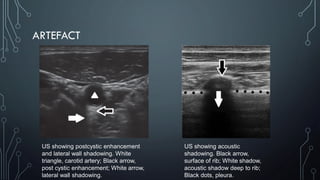
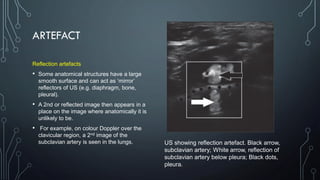
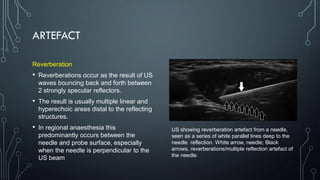
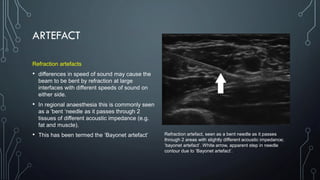
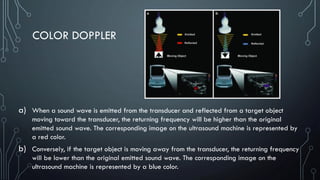
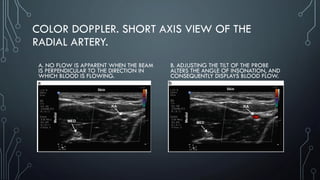
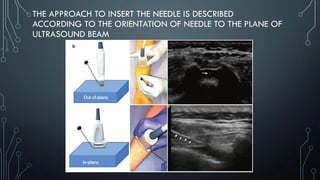
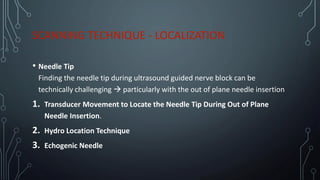
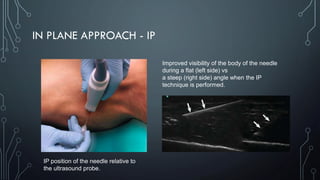
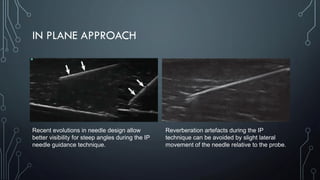
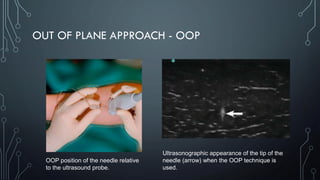
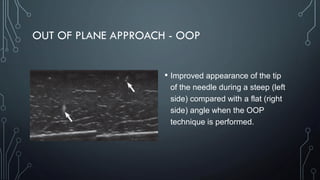
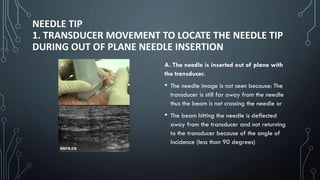
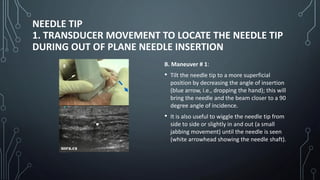
The document covers a workshop on basic ultrasound guidance for pain management, highlighting the importance of real-time visualization for accurately targeting nerves while noting limitations such as operator dependence and the need for substantial training. It details essential techniques for image capture, optimization, and interpretation, emphasizing the proper selection of equipment and scanning methods. Furthermore, it addresses common artifacts that can affect image clarity and the significance of understanding anatomy for effective ultrasound-guided procedures.