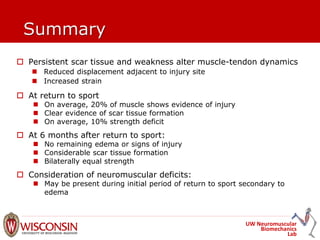
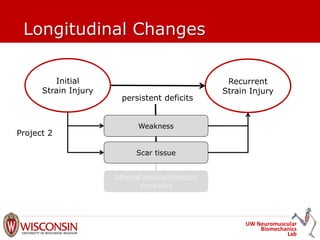
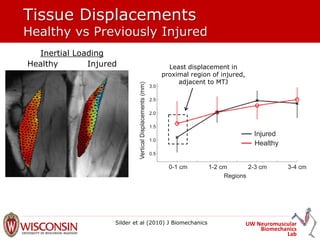
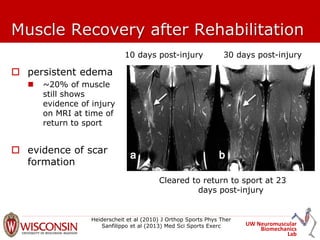
The document discusses MRI findings related to hamstring strain injuries and recovery, emphasizing the correlation between injury severity and recovery time. It highlights the increased risk of re-injury associated with specific factors such as previous strain injuries and persistent deficits in muscle function. The conclusions stress that a significant proportion of muscle remains injured at the time of return to sport, often accompanied by scar tissue formation and strength deficits.





















![UW Neuromuscular
Biomechanics
Lab
Predicting Time to Return to Sport
and Re-injury from MRI
MRI measures associated with increased recovery time:
Baseline: cradio-caudal length of injury on MRI (r=0.41)
Post-rehabilitation: none
Baseline MRI measures associated with re-injury
Cross sectional area of injury (% of total cross sectional
area)
Re-injury (n=4): 87% [95% CI: 68%, 100%]
No re-injury (n=25): 54% [95% CI: 43%, 65%]
Silder et al. (2013) J Orthop Sports Phys Ther](https://image.slidesharecdn.com/17muscletech14hamstringmrheiderscheit-141014075715-conversion-gate02/85/Bryan-Heiderscheit-MRI-findings-25-320.jpg)