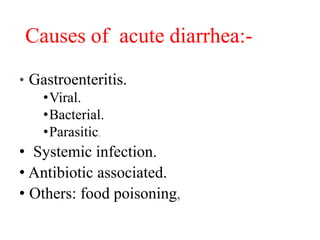
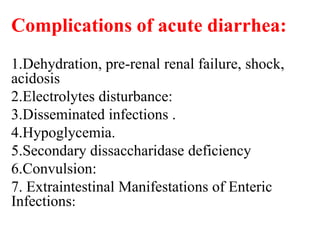
Acute diarrhea in children is commonly caused by viral, bacterial, or parasitic gastroenteritis acquired through the fecal-oral route. Rotavirus is a frequent cause of winter diarrhea and presents with vomiting lasting 3-4 days and watery diarrhea for 7-10 days. Vibrio cholerae causes a profuse, painless watery diarrhea and can lead to severe dehydration if not treated promptly with oral rehydration and antibiotics. Shigella infection presents with bloody mucus diarrhea and may develop into disseminated infection. Preventing diarrhea requires exclusive breastfeeding, vaccination, clean water sources, and proper hygiene.