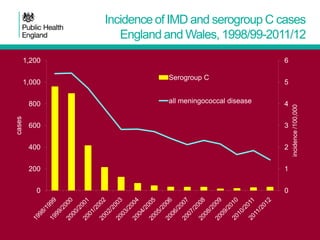
The MCC vaccine program in the UK has dramatically reduced MenC disease rates since its introduction. While protection wanes over time, herd immunity from reduced carriage in teenagers has sustained impact. To maintain control, the schedule is being updated to boost teenagers and address waning immunity. A booster will be added in year 10, and broader quadrivalent vaccines may be considered for this dose.