This randomized clinical trial compared the effectiveness of mindfulness-based stress reduction (MBSR), cognitive behavioral therapy (CBT), and usual care for treating chronic low back pain. 342 adults with chronic low back pain were randomly assigned to receive MBSR, CBT, or usual care. At 26 weeks, participants receiving MBSR or CBT reported significantly greater improvement in back pain and functional limitations compared to usual care. There were no significant differences in outcomes between MBSR and CBT. These findings suggest that MBSR may be an effective treatment option for chronic low back pain.
![Copyright 2016 American Medical Association. All rights reserved.
Effect of Mindfulness-Based Stress Reduction vs
Cognitive Behavioral Therapy or Usual Care on Back Pain
andFunctionalLimitationsinAdultsWithChronicLowBackPain
A Randomized Clinical Trial
Daniel C. Cherkin, PhD; Karen J. Sherman, PhD; Benjamin H. Balderson, PhD; Andrea J. Cook, PhD;
Melissa L. Anderson, MS; Rene J. Hawkes, BS; Kelly E. Hansen, BS; Judith A. Turner, PhD
IMPORTANCE Mindfulness-based stress reduction (MBSR) has not been rigorously evaluated
for young and middle-aged adults with chronic low back pain.
OBJECTIVE To evaluate the effectiveness for chronic low back pain of MBSR vs cognitive
behavioral therapy (CBT) or usual care.
DESIGN, SETTING, AND PARTICIPANTS Randomized, interviewer-blind, clinical trial in an
integrated health care system in Washington State of 342 adults aged 20 to 70 years with
chronic low back pain enrolled between September 2012 and April 2014 and randomly
assigned to receive MBSR (n = 116), CBT (n = 113), or usual care (n = 113).
INTERVENTIONS CBT (training to change pain-related thoughts and behaviors) and MBSR
(training in mindfulness meditation and yoga) were delivered in 8 weekly 2-hour groups.
Usual care included whatever care participants received.
MAIN OUTCOMES AND MEASURES Coprimary outcomes were the percentages of participants
with clinically meaningful (Ն30%) improvement from baseline in functional limitations
(modified Roland Disability Questionnaire [RDQ]; range, 0-23) and in self-reported back pain
bothersomeness (scale, 0-10) at 26 weeks. Outcomes were also assessed at 4, 8, and 52 weeks.
RESULTS There were 342 randomized participants, the mean (SD) [range] age was 49.3 (12.3)
[20-70] years, 224 (65.7%) were women, mean duration of back pain was 7.3 years
(range, 3 months-50 years), 123 (53.7%) attended 6 or more of the 8 sessions, 294 (86.0%)
completed the study at 26 weeks, and 290 (84.8%) completed the study at 52 weeks. In
intent-to-treat analyses at 26 weeks, the percentage of participants with clinically meaningful
improvement on the RDQ was higher for those who received MBSR (60.5%) and CBT
(57.7%) than for usual care (44.1%) (overall P = .04; relative risk [RR] for MBSR vs usual care,
1.37 [95% CI, 1.06-1.77]; RR for MBSR vs CBT, 0.95 [95% CI, 0.77-1.18]; and RR for CBT vs usual
care, 1.31 [95% CI, 1.01-1.69]). The percentage of participants with clinically meaningful
improvement in pain bothersomeness at 26 weeks was 43.6% in the MBSR group and 44.9%
in the CBT group, vs 26.6% in the usual care group (overall P = .01; RR for MBSR vs usual care,
1.64 [95% CI, 1.15-2.34]; RR for MBSR vs CBT, 1.03 [95% CI, 0.78-1.36]; and RR for CBT vs
usual care, 1.69 [95% CI, 1.18-2.41]). Findings for MBSR persisted with little change at 52
weeks for both primary outcomes.
CONCLUSIONS AND RELEVANCE Among adults with chronic low back pain, treatment with
MBSR or CBT, compared with usual care, resulted in greater improvement in back pain and
functional limitations at 26 weeks, with no significant differences in outcomes between
MBSR and CBT. These findings suggest that MBSR may be an effective treatment option for
patients with chronic low back pain.
TRIAL REGISTRATION clinicaltrials.gov Identifier: NCT01467843
JAMA. 2016;315(12):1240-1249. doi:10.1001/jama.2016.2323
Editorial page 1236
Author Video Interview and
JAMA Report Video at
jama.com
Supplemental content at
jama.com
CME Quiz at
jamanetworkcme.com
Author Affiliations: Group Health
Research Institute, Seattle,
Washington (Cherkin, Sherman,
Balderson, Cook, Anderson, Hawkes,
Hansen); Department of Health
Services, University of Washington,
Seattle (Cherkin); Department of
Family Medicine, University of
Washington, Seattle (Cherkin);
Department of Epidemiology,
University of Washington, Seattle
(Sherman); Department of
Biostatistics, University of
Washington, Seattle (Cook);
Department of Psychiatry and
Behavioral Sciences, University of
Washington, Seattle (Turner);
Department of Rehabilitation
Medicine, University of Washington,
Seattle (Turner).
Corresponding Author: Daniel C.
Cherkin, PhD, Group Health
Research Institute, 1730 Minor Ave,
Ste 1600, Seattle, WA 98101
(cherkin.d@ghc.org).
Research
Original Investigation
1240 (Reprinted) jama.com
Copyright 2016 American Medical Association. All rights reserved.
Downloaded From: http://jama.jamanetwork.com/ by Paul Coelho on 05/07/2016](https://image.slidesharecdn.com/mbsrvscbt-160507153023/75/MBSR-vs-CBT-1-2048.jpg)

![Copyright 2016 American Medical Association. All rights reserved.
adherence to the protocol, either in person or via audio re-
cording, for at least 1 session per group.
MBSR was modeled closely after the original MBSR
program9
—adaptated from the 2009 MBSR instructor’s
manual18
byaseniorMBSRinstructor.TheMBSRprogramdoes
not focus specifically on a particular condition such as pain.
All classes included didactic content and mindfulness prac-
tice (body scan, yoga, meditation [attention to thoughts, emo-
tions, and sensations in the present moment without trying
to change them, sitting meditation with awareness of breath-
ing, and walking meditation]).
The CBT protocol included CBT techniques most com-
monly applied and studied for chronic low back pain.8,19-22
The intervention included (1) education about chronic pain,
relationships between thoughts and emotional and physical
reactions, sleep hygiene, relapse prevention, and mainte-
nance of gains; and (2) instruction and practice in changing
dysfunctional thoughts, setting and working toward behav-
ioral goals, relaxation skills (abdominal breathing, progres-
sive muscle relaxation, and guided imagery), activity pacing,
and pain-coping strategies. Between-session activities
included reading chapters of The Pain Survival Guide: How to
Reclaim Your Life.21
Mindfulness, meditation, and yoga tech-
niques were proscribed in CBT; methods to challenge dys-
functional thoughts were proscribed in MBSR.
Follow-up
Trained interviewers, masked to treatment group, collected
data by telephone at baseline (before randomization) and af-
ter randomization at weeks 4 (midtreatment), 8 (posttreat-
ment), 26 (primary end point), and 52. Participants were com-
pensated $20 for each interview.
Measures
Sociodemographic and back pain information was obtained at
baseline (Table 1). All primary outcome measures were admin-
istered at each time point; secondary outcomes were as-
sessed at all time points except 4 weeks.
Coprimary Outcomes
Back pain–related functional limitation was assessed by the
RDQ16
and modified to 23 (vs the original 24) items and to
ask about the past week rather than today only. Higher
scores (range 0-23) indicate greater functional limitation.
The original RDQ has demonstrated reliability, validity, and
sensitivity to clinical change.23
Back pain bothersomeness in
the past week was measured on a 0 to 10 scale (0 indicates
not at all bothersome; 10 indicates extremely bothersome).
Primary analyses of this study examined the percentages of
participants with clinically meaningful improvement (≥30%
improvement from baseline)24
on each measure. Secondary
Figure. Flow of Participants Through Trial Comparing Mindfulness-Based Stress Reduction With Cognitive Behavioral Therapy and Usual Care
for Chronic Low Back Pain
1425 Excluded
412 Pain <3 months
338 Unable to attend classes
357 Other
122 Pain rated <4 on 0-10 scale
196 Activity interference <3 on 0-10 scale
1767 Individuals assessed for eligibility
342 Randomized
113 Randomized to receive usual care 116 Randomized to receive mindfulness-
based stress reductiona
13 Did not attend any classes
3 Time conflict or logisticsc
2 Illness or injury
8 Unknown
113 Randomized to receive cognitive
behavioral therapyb
13 Did not attend any classes
4 Time conflict or logisticsc
4 Illness or injury
5 Unknown
113 Included in analysis of coprimary
and secondary outcomes
116 Included in analysis of coprimary
and secondary outcomes
112 Included in analysis of coprimary
and secondary outcomes
1 Excluded (missing baseline data)
100 Followed up at 4 wk
94 Followed up at 8 wk
95 Followed up at 26 wk
92 Followed up at 52 wk
97 Followed up at 4 wk
98 Followed up at 8 wk
92 Followed up at 26 wk
92 Followed up at 52 wk
108 Followed up at 4 wk
106 Followed up at 8 wk
107 Followed up at 26 wk
106 Followed up at 52 wk
a
Of the 116 participants randomized to receive mindfulness-based stress
reduction, 103 attended at least 1 class and 59 attended at least 6 classes. For
those who attended at least 1 class, the median (interquartile range [IQR]) was
6 (3-7) classes per participant. Participants were recruited in 10 separate
waves (median 12.5 [IQR, 7-16] participants per wave).
b
Of the 113 participants randomized to receive cognitive behavioral therapy,
100 attended at least 1 class and 64 attended at least 6 classes. For those who
attended at least 1 class, the median (IQR) was 6 (3-7) classes per participant.
Participants were recruited in 10 separate waves (median 13 [IQR, 5-14]
participants per wave).
c
Logistics, given as a reason for not attending any classes, specifically refers to
transportation problems (no car or acceptable bus schedules) or obtaining
child care during classes.
Research Original Investigation Mindfulness-Based Stress Reduction vs Cognitive Behavioral Therapy
1242 JAMA March 22/29, 2016 Volume 315, Number 12 (Reprinted) jama.com
Copyright 2016 American Medical Association. All rights reserved.
Downloaded From: http://jama.jamanetwork.com/ by Paul Coelho on 05/07/2016](https://image.slidesharecdn.com/mbsrvscbt-160507153023/75/MBSR-vs-CBT-3-2048.jpg)
![Copyright 2016 American Medical Association. All rights reserved.
analyses compared the adjusted mean change from baseline
between groups.
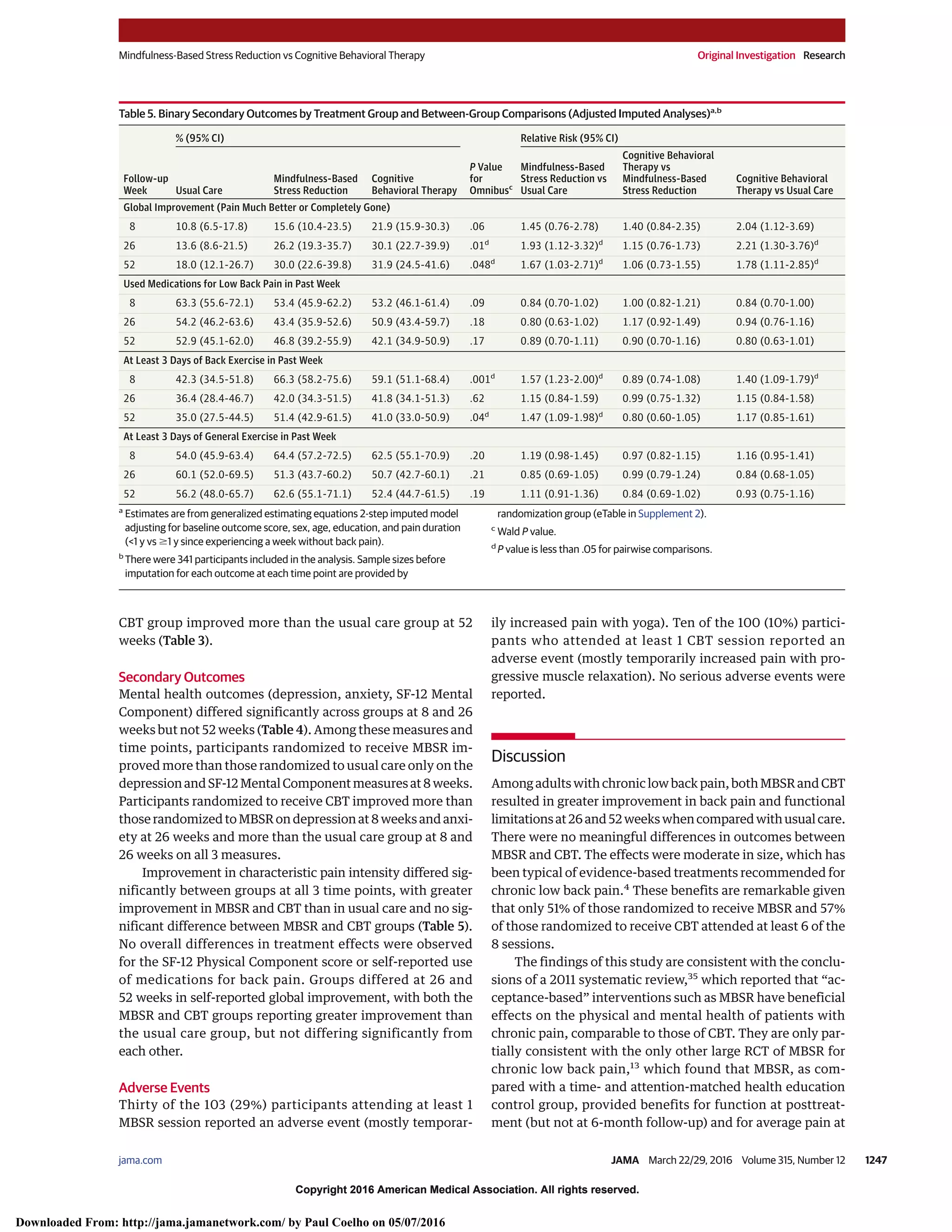
Secondary Outcomes
Depressive symptoms were assessed using the Patient Health
Questionnaire-8 (PHQ-8; range, 0-24; higher scores indicate
greater severity).25
Anxiety was measured using the 2-item
Generalized Anxiety Disorder scale (GAD-2; range, 0-6; higher
scores indicate greater severity).26
Characteristic pain inten-
sity was assessed as the mean of 3 ratings (gauged on a 0-10
scale; current, worst, and average back pain in the previous
month; range; higher scores indicate greater intensity) from
Table 1. Baseline Characteristics of Participants by Treatment Group
No. (%)
All
(n = 341)
Usual Care
(n = 113)
Mindfulness-Based
Stress Reduction
(n = 116)
Cognitive Behavioral
Therapy
(n = 112)
Sociodemographic Characteristics
Age, mean (SD), y 49.3 (12.3) 48.9 (12.5) 50.0 (11.9) 49.1 (12.6)
Women 224 (65.7) 87 (77.0) 71 (61.2) 66 (58.9)
Education
≤High school 26 (7.6) 5 (4.4) 14 (12.1) 7 (6.3)
Some college or vocational
school
114 (33.4) 37 (32.7) 41 (35.3) 36 (32.1)
College graduate 201 (58.9) 71 (62.8) 61 (52.6) 69 (61.6)
Race
White 278 (82.5) 88 (80.0) 97 (84.4) 93 (83.0)
Asian 13 (3.9) 3 (2.7) 4 (3.5) 6 (5.4)
African American 11 (3.3) 3 (2.7) 4 (3.5) 4 (3.6)
Othera
35 (10.4) 16 (14.6) 10 (8.7) 9 (8.0)
Hispanic ethnicity 23 (6.8) 8 (7.1) 5 (4.3) 10 (8.9)
Married or living as married 249 (73.0) 79 (69.9) 85 (73.3) 85 (75.9)
Annual family income
> US $55 000
206 (62.6) 72 (66.1) 66 (58.4) 68 (63.6)
Employed 263 (77.1) 89 (78.8) 87 (75.0) 87 (77.7)
Back Pain History and Expectations
≥1 Year since 1 week without LBP 269 (78.9) 86 (76.1) 93 (80.2) 90 (80.4)
Had spinal injection for LBP 8 (2.7) 3 (3.1) 3 (3.0) 2 (2.0)
Currently reporting “a lot of pain”
in site other than back
100 (29.3) 35 (31.0) 34 (29.3) 31 (27.7)
Back pain in last 180 days,
median (IQR), d
160 (100-180) 160 (100-180) 170 (115-180) 160 (100-180)
Expects LBP to “be much better
or gone” in 1 year
101 (29.8) 36 (31.9) 34 (29.6) 31 (27.9)
Expects LBP self-management
program will be helpful,
mean (SD), scoreb
7.5 (1.9) 7.8 (1.8) 7.6 (2.0) 7.2 (1.8)
Baseline Measures of Primary Outcome Scores
RDQ (modified), mean (SD)c
11.4 (4.8) 10.9 (4.8) 11.8 (4.7) 11.5 (5.0)
Pain bothersomeness rating,
mean (SD)d
6.0 (1.6) 6.0 (1.6) 6.1 (1.6) 6.0 (1.5)
Baseline Measures of Secondary Outcome Scores
Characteristic pain intensity,
mean (SD)d
5.9 (1.3) 5.8 (1.3) 6.0 (1.3) 5.8 (1.2)
PHQ-8, mean (SD)e
5.6 (4.1) 5.3 (3.8) 5.7 (4.0) 5.7 (4.4)
GAD-2, mean (SD)f
1.4 (1.5) 1.5 (1.3) 1.4 (1.5) 1.4 (1.5)
GAD-2, median (IQR)f
1 (0-2) 1 (0-2) 1 (0-2) 1 (0-2)
SF-12 Physical, mean (SD)g
39.1 (7.9) 39.7 (7.6) 38.2 (7.5) 39.4 (8.6)
SF-12 Mental, mean (SD)g
39.9 (7.9) 39.8 (7.4) 40.6 (8.1) 39.4 (8.2)
Baseline Measures of Other Secondary Outcomes
Any medication use for LBP
in past week
252 (73.9) 82 (72.6) 85 (73.3) 85 (75.9)
Opioids use for LBP in past week 38 (11.1) 12 (10.6) 14 (12.1) 12 (10.7)
Back-specific exercise ≥3 days
in past week
137 (40.2) 44 (38.9) 48 (41.4) 45 (40.2)
General exercise ≥3 days
in past week
167 (49.0) 53 (46.9) 57 (49.1) 57 (50.9)
Abbreviations: GAD-2, Generalized
Anxiety Disorder-2; IQR, interquartile
range; LBP, low back pain;
PHQ-8, Patient Health
Questionnaire-8; RDQ, Roland
Disability Questionnaire;
SF-12, 12-Item Short Form
Health Survey.
a
Race/ethnicity subcategory of Other
indicates multiracial (19), other (not
specified [9]), missing (5), Native
American/Pacific Islander (2).
b
LBP self-management score range is
0 to 10. Higher scores indicate more
program success.
c
Modified RDQ score range is 0 to
23. Higher scores indicate worse
function.
d
Pain bothersomeness rating and
characteristic pain intensity score
ranges are both 0 to 10. Higher
scores indicate greater pain.
e
PHQ-8 score range is 0 to 24.
Higher scores indicate more
depression.
f
GAD-2 score range is 0 to 6. Higher
scores indicate more anxiety.
g
SF-12 physical and mental
component scores range from 0 to
100. Lower scores indicate poorer
health status and higher ones
indicate higher function.
Mindfulness-Based Stress Reduction vs Cognitive Behavioral Therapy Original Investigation Research
jama.com (Reprinted) JAMA March 22/29, 2016 Volume 315, Number 12 1243
Copyright 2016 American Medical Association. All rights reserved.
Downloaded From: http://jama.jamanetwork.com/ by Paul Coelho on 05/07/2016](https://image.slidesharecdn.com/mbsrvscbt-160507153023/75/MBSR-vs-CBT-4-2048.jpg)

![Copyright 2016 American Medical Association. All rights reserved.
domized to receive MBSR attended the 6-hour retreat. Over-
all follow-up response rates ranged from 89.2% (305 partici-
pants) at 4 weeks to 84.8%(290 participants) at 52 weeks and
were higher in the usual care group (95.6% [108] at 4 weeks
and 93.8% [106] at 52 weeks).
At baseline, treatment groups were similar in sociodemo-
graphic and pain characteristics except for more women in
usual care and fewer college graduates in the MBSR group
(Table 1). Overall, 269 (78.9%) reported at least 1 year since a
week without back pain and most reported pain on at least 160
of the previous 180 days. Mean duration of back pain was 7.3
years (range, 3 months-50 years). The mean (SD) RDQ score
(11.4 [4.8]) and pain bothersomeness rating (6.0 [1.6]) indi-
cated moderate levels of severity. Opioids use for pain during
Table 2. Coprimary Outcomes: Percentage of Participants With Clinically Meaningful Improvement by Treatment Group and Relative Risks Comparing
Treatment Groups (Adjusted Imputed Analyses)a,b
Follow-up
Week
% (95% CI) With Clinically Meaningful Improvement
P Value
for Omnibusc
Relative Risk (95% CI)
Usual Care
Mindfulness-Based
Stress Reduction
Cognitive
Behavioral Therapy
Mindfulness-Based
Stress Reduction vs
Usual Care
Cognitive
Behavioral Therapy vs
Mindfulness-Based
Stress Reduction
Cognitive
Behavioral Therapy vs
Usual Care
Roland Disability Questionnaire Results
4 27.3 (20.3-36.6) 34.5 (26.8-44.3) 24.7 (18.1-33.8) .23 1.26 (0.86-1.86) 0.72 (0.48-1.07) 0.91 (0.59-1.39)
8 35.4 (27.6-45.2) 47.4 (38.9-57.6) 51.9 (43.6-61.7) .04d
1.34 (0.98-1.84) 1.10 (0.84-1.42) 1.47 (1.09-1.98)d
26 44.1 (35.9-54.2) 60.5 (52.0-70.3) 57.7 (49.2-67.6) .04d
1.37 (1.06-1.77)d
0.95 (0.77-1.18) 1.31 (1.01-1.69)d
52 48.6 (40.3-58.6) 68.6 (60.3-78.1) 58.8 (50.6-68.4) .01d
1.41 (1.13-1.77)d
0.86 (0.70-1.04) 1.21 (0.95-1.54)
Pain Bothersomeness Results
4 20.6 (14.6-28.9) 19.1 (13.3-27.4) 21.7 (15.3-30.6) .88 0.93 (0.56-1.52) 1.14 (0.69-1.87) 1.05 (0.65-1.71)
8 24.7 (18.1-33.6) 36.1 (28.3-46.0) 33.8 (26.5-43.2) .15 1.46 (0.99-2.16) 0.94 (0.67-1.32) 1.37 (0.93-2.02)
26 26.6 (19.8-35.9) 43.6 (35.6-53.3) 44.9 (36.7-55.1) .01d
1.64 (1.15-2.34)d
1.03 (0.78-1.36) 1.69 (1.18-2.41)d
52 31.0 (23.8-40.3) 48.5 (40.3-58.3) 39.6 (31.7-49.5) .02d
1.56 (1.14-2.14)d
0.82 (0.62-1.08) 1.28 (0.91-1.79)
a
Estimates from generalized estimating equations 2-step imputed model
adjusting for baseline outcome score, sex, age, education, and pain duration
(<1 y vs Ն1 y since experiencing a week without back pain).
b
n = 341 Included in the analysis; 1 randomized participant who did not
complete the baseline survey was excluded. Follow-up rates (sample sizes
before imputation) at each time point by randomization group are detailed in
the Figure. In addition, 1 participant in the mindfulness-based stress reduction
group at 8 weeks and 1 in the usual care group at 26 weeks were missing data
for the pain bothersomeness outcome. Sample sizes before imputation for
each outcome at each time point are provided by randomization group
(eTable in Supplement 2).
c
Wald P value.
d
P value is less than .05 for pairwise comparisons.
Table 3. Coprimary Outcomes: Mean (95% CI) Change by Treatment Group and Mean (95% CI) Differences Between Treatment Groups
(Adjusted Imputed Analyses)a,b
Follow-up
Week
Change From Baseline, Mean (95% CI)
P Value for
Omnibusc
Between-Group Differences, Mean (95% CI)
Usual Care
Mindfulness-Based
Stress Reduction
Cognitive
Behavioral Therapy
Mindfulness-Based
Stress Reduction vs
Usual Care
Cognitive
Behavioral Therapy vs
Mindfulness-Based
Stress Reduction
Cognitive
Behavioral Therapy vs
Usual Care
Roland Disability Questionnaire Results
4 −1.28
(−1.91 to −0.65)
−1.93
(−2.61 to −1.25)
−1.44
(−2.10 to −0.78)
.37 −0.65
(−1.59 to 0.28)
0.49
(−0.46 to 1.45)
−0.16
(−1.07 to 0.76)
8 −1.83
(−2.59 to −1.07)
−3.40
(−4.22 to −2.59)
−3.37
(−4.14 to −2.60)
.005d
−1.57
(−2.70 to −0.45)d
0.04
(−1.11 to 1.18)
−1.54
(−2.61 to −0.46)d
26 −2.96
(−3.79 to −2.14)
−4.33
(−5.16 to −3.51)
−4.38
(−5.3 to −3.47)
.03d
−1.37
(−2.55 to −0.19)d
−0.05
(−1.31 to 1.21)
−1.42
(−2.66 to −0.18)d
52 −3.43
(−4.33 to −2.52)
−5.3
(−6.16 to −4.43)
−4.78
(−5.67 to −3.89)
.01d
−1.87
(−3.14 to −0.60)d
0.51
(−0.75 to 1.78)
−1.36
(−2.63 to −0.08)d
Pain Bothersomeness Results
4 −0.68
(−0.98 to −0.38)
−0.57
(−0.87 to −0.27)
−0.79
(−1.13 to −0.44)
.66 0.11
(−0.32 to 0.53)
−0.21
(−0.67 to 0.25)
−0.11
(−0.56 to 0.35)
8 −0.67
(−1.02 to −0.33)
−1.40
(−1.71 to −1.10)
−1.28
(−1.62 to −0.94)
.005d
−0.73
(−1.19 to −0.27)d
0.12
(−0.34 to 0.58)
−0.61
(−1.09 to −0.12)d
26 −0.84
(−1.21 to −0.46)
−1.48
(−1.86 to −1.11)
−1.56
(−2.02 to −1.11)
.02d
−0.64
(−1.18 to −0.11)d
−0.08
(−0.68 to 0.51)
−0.73
(−1.32 to −0.13)d
52 −1.10
(−1.48 to −0.71)
−1.95
(−2.32 to −1.59)
−1.76
(−2.14 to −1.39)
.005d
−0.85
(−1.39 to −0.32)d
0.19
(−0.33 to 0.71)
−0.67
(−1.20 to −0.13)d
a
Estimates are from generalized estimating equations 2-step imputed
model adjusting for baseline outcome score, sex, age, education,
and pain duration (<1 y vs Ն1 y since experiencing a week without
back pain).
b
There were 341 participants included in the analysis. Sample sizes before
imputation for each outcome at each time point are provided by
randomization group (eTable in Supplement 2).
c
Wald P value.
d
P value is less than .05 for pairwise comparisons.
Mindfulness-Based Stress Reduction vs Cognitive Behavioral Therapy Original Investigation Research
jama.com (Reprinted) JAMA March 22/29, 2016 Volume 315, Number 12 1245
Copyright 2016 American Medical Association. All rights reserved.
Downloaded From: http://jama.jamanetwork.com/ by Paul Coelho on 05/07/2016](https://image.slidesharecdn.com/mbsrvscbt-160507153023/75/MBSR-vs-CBT-6-2048.jpg)
![Copyright 2016 American Medical Association. All rights reserved.
the past week was reported by 38 participants (11.1%). Seven-
teen percent had at least moderate levels of depression (PHQ-8
scores ≥10) and 18% had at least moderate levels of anxiety
(GAD-2 scores ≥3).
Coprimary Outcomes
At the 26-week primary end point, the groups differed signifi-
cantly (P = .04) in percent with clinically meaningful improve-
ment on the RDQ (MBSR 60.5%, usual care 44.1%, CBT 57.7%;
Table 2). Participants randomized to receive MBSR were more
likely than those randomized to usual care to show meaning-
ful improvement on the RDQ (RR, 1.37 [95% CI, 1.06-1.77]) but
did not differ significantly from those randomized to CBT. The
overall difference among groups in clinically meaningful im-
provement in pain bothersomeness at 26 weeks was also sta-
tistically significant (MBSR 43.6%, usual care 26.6%, CBT
44.9%;P = .01).ParticipantsrandomizedtoreceiveMBSRwere
more likely to show meaningful improvement when com-
pared with usual care (RR, 1.64 [95% CI, 1.15-2.34]) but not
when compared with CBT (RR, 1.03 [95% CI, 0.78-1.36]). The
significant differences between MBSR and usual care and
the nonsignificant differences between MBSR and CBT, in
percent with meaningful function and pain improvement,
persisted at 52 weeks, with RRs similar to those at 26 weeks
(Table 2). CBT was superior to usual care for both primary out-
comesat26weeksbutnot52weeks.TreatmenteffectsofMBSR
and CBT were not apparent before end of treatment (8 weeks).
Generally similar results were found when the primary out-
comes were analyzed as continuous variables, although more
differences were statistically significant at 8 weeks, and the
Table 4. Mean Change From Baseline of Continuous Secondary Outcomes by Treatment Group and Between-Group Comparisons
(Adjusted Imputed Analyses)a,b
Follow-up
Week
Change Estimates, Mean (95% CI)
P Value for
Omnibusc
Between-Group Differences, Mean (95% CI)
Usual Care
Mindfulness-Based
Stress Reduction
Cognitive
Behavioral Therapy
Mindfulness-Based
Stress Reduction vs
Usual Care
Cognitive
Behavioral Therapy vs
Mindfulness-Based
Stress Reduction
Cognitive
Behavioral Therapy vs
Usual Care
Depression (PHQ-8)
8 −0.12
(−0.74 to 0.50)
−1.60
(−2.15 to −1.05)
−2.29
(−2.66 to −1.92)
<.001d
−1.48
(−2.31 to −0.64)d
−0.69
(−1.35 to −0.02)d
−2.17
(−2.89 to −1.45)d
26 −0.64
(−1.23 to −0.06)
−1.32
(−1.81 to −0.83)
−1.80
(−2.35 to −1.26)
.02d
−0.68
(−1.45 to 0.09)
−0.48
(−1.21 to 0.26)
−1.16
(−1.95 to −0.37)d
52 −0.88
(−1.50 to −0.27)
−1.51
(−2.09 to −0.92)
−1.72
(−2.28 to −1.16)
.13 −0.62
(−1.48 to 0.23)
−0.21
(−1.03 to 0.61)
−0.83
(−1.67 to 0.00)
Anxiety (GAD-2)
8 −0.09
(−0.32 to 0.13)
−0.33
(−0.56 to −0.10)
−0.51
(−0.69 to −0.33)
.02d
−0.24
(−0.56 to 0.09)
−0.18
(−0.47 to 0.11)
−0.41
(−0.70 to −0.13)d
26 0.02
(−0.24 to 0.28)
0.00
(−0.28 to 0.28)
−0.49
(−0.72 to −0.25)
.005d
−0.02
(−0.41 to 0.37)
−0.49
(−0.85 to −0.12)d
−0.51
(−0.86 to −0.16)d
52 −0.14
(−0.40 to 0.12)
−0.15
(−0.40 to 0.10)
−0.39
(−0.59 to −0.18)
.23 0.00
(−0.37 to 0.36)
−0.24
(−0.56 to 0.08)
−0.24
(−0.58 to 0.09)
Characteristic Pain Intensity
8 −0.37
(−0.62 to −0.12)
−1.00
(−1.28 to −0.73)
−0.86
(−1.12 to −0.59)
.002d
−0.63
(−1.01 to −0.26)d
0.15
(−0.24 to 0.53)
−0.49
(−0.84 to −0.13)d
26 −0.65
(−0.95 to −0.35)
−1.10
(−1.42 to −0.77)
−1.15
(−1.44 to −0.86)
.04d
−0.45
(−0.89 to −0.01)d
−0.05
(−0.50 to 0.39)
−0.50
(−0.92 to −0.09)d
52 −0.79
(−1.10 to −0.48)
−1.42
(−1.72 to −1.12)
−1.40
(−1.74 to −1.05)
.007d
−0.63
(−1.06 to −0.19)d
0.02
(−0.44 to 0.48)
−0.61
(−1.07 to −0.14)d
SF-12 Physical Component Score
8 2.21
(1.12 to 3.30)
3.69
(2.61 to 4.77)
3.24
(2.21 to 4.27)
.16 1.48
(−0.06 to 3.02)
−0.45
(−1.95 to 1.05)
1.03
(−0.48 to 2.54)
26 3.27
(2.09 to 4.44)
3.58
(2.15 to 5.01)
3.78
(2.56 to 5.00)
.84 0.31
(−1.53 to 2.16)
0.20
(−1.69 to 2.10)
0.52
(−1.19 to 2.22)
52 2.93
(1.70 to 4.16)
3.87
(2.55 to 5.19)
3.79
(2.55 to 5.03)
.50 0.94
(−0.86 to 2.74)
−0.08
(−1.91 to 1.75)
0.86
(−0.87 to 2.60)
SF-12 Mental Component Score
8 −0.65
(−1.86 to 0.55)
1.68
(0.57 to 2.79)
1.77
(0.82 to 2.72)
.004d
2.33
(0.68 to 3.99)d
0.09
(−1.37 to 1.54)
2.42
(0.87 to 3.97)d
26 −1.11
(−2.39 to 0.17)
0.45
(−0.85 to 1.76)
2.13
(0.86 to 3.40)
.002d
1.57
(−0.27 to 3.40)
1.68
(−0.12 to 3.47)
3.24
(1.44 to 5.04)d
52 0.75
(−0.58 to 2.08)
2.01
(0.74 to 3.28)
1.81
(0.59 to 3.03)
.36 1.26
(−0.60 to 3.11)
−0.19
(−1.95 to 1.56)
1.06
(−0.75 to 2.88)
Abbreviations: GAD-2, Generalized Anxiety Disorder-2; PHQ-8, Patient Health
Questionnaire-8; SF-12, 12-Item Short Form Health Survey.
a
Estimates are from generalized estimating equations 2-step imputed model
adjusting for baseline outcome score, sex, age, education, and pain duration
(<1 y vs Ն1 y since experiencing a week without back pain).
b
There were 341 participants included in the analysis. Sample sizes before
imputation for each outcome at each time point are provided by
randomization group (eTable in Supplement 2).
c
Wald P value.
d
P value is less than .05 for pairwise comparisons.
Research Original Investigation Mindfulness-Based Stress Reduction vs Cognitive Behavioral Therapy
1246 JAMA March 22/29, 2016 Volume 315, Number 12 (Reprinted) jama.com
Copyright 2016 American Medical Association. All rights reserved.
Downloaded From: http://jama.jamanetwork.com/ by Paul Coelho on 05/07/2016](https://image.slidesharecdn.com/mbsrvscbt-160507153023/75/MBSR-vs-CBT-7-2048.jpg)