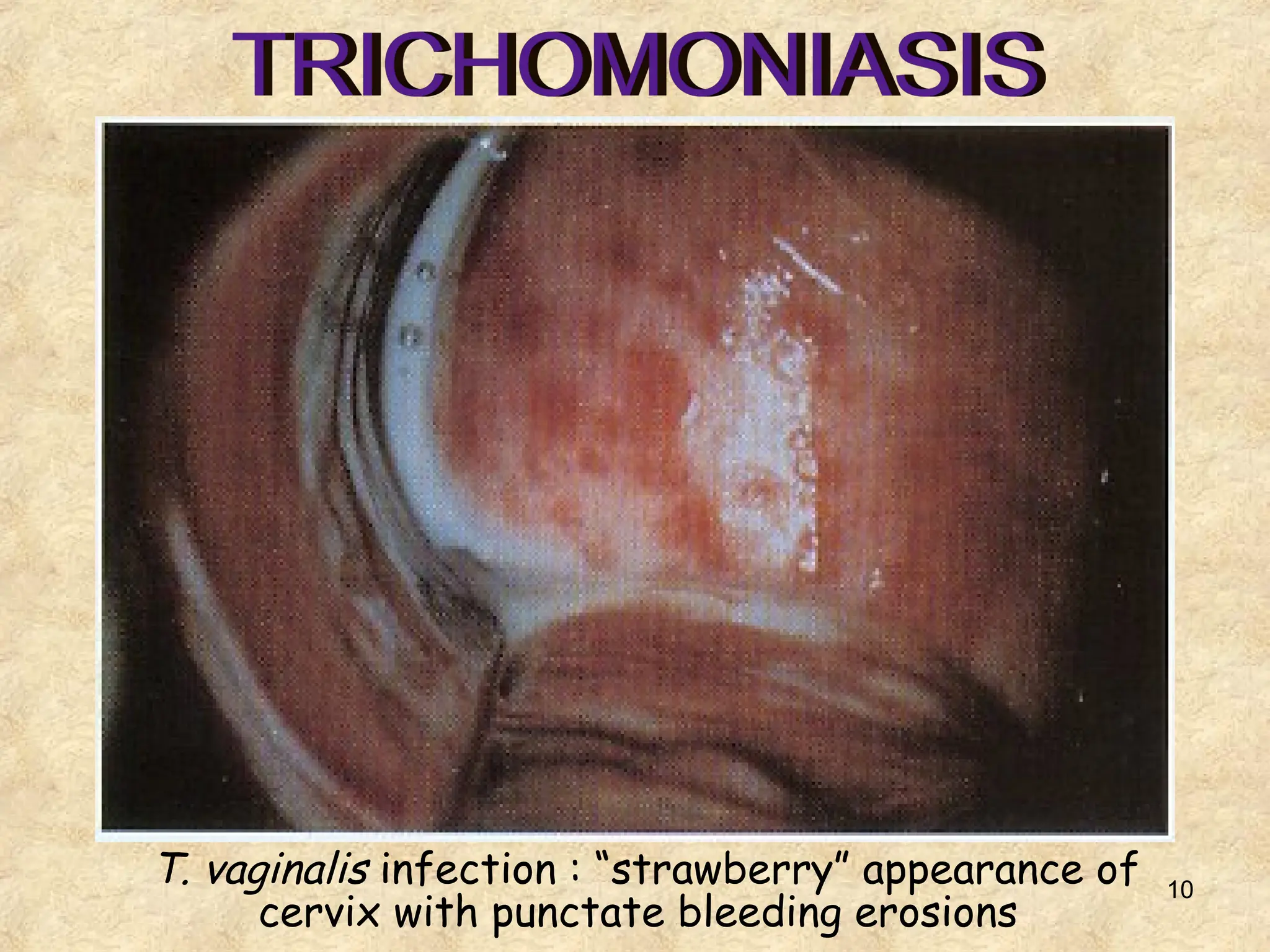
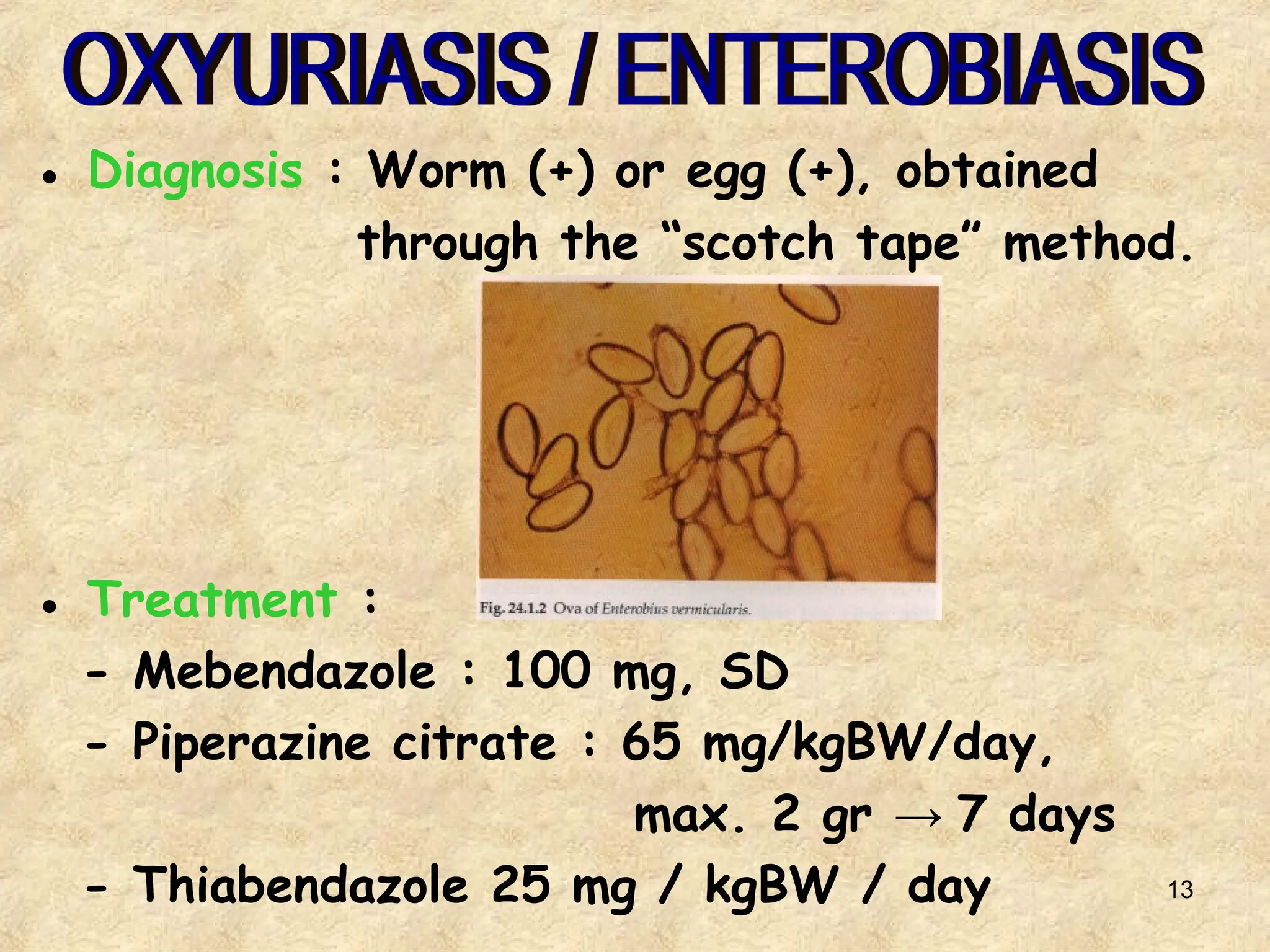
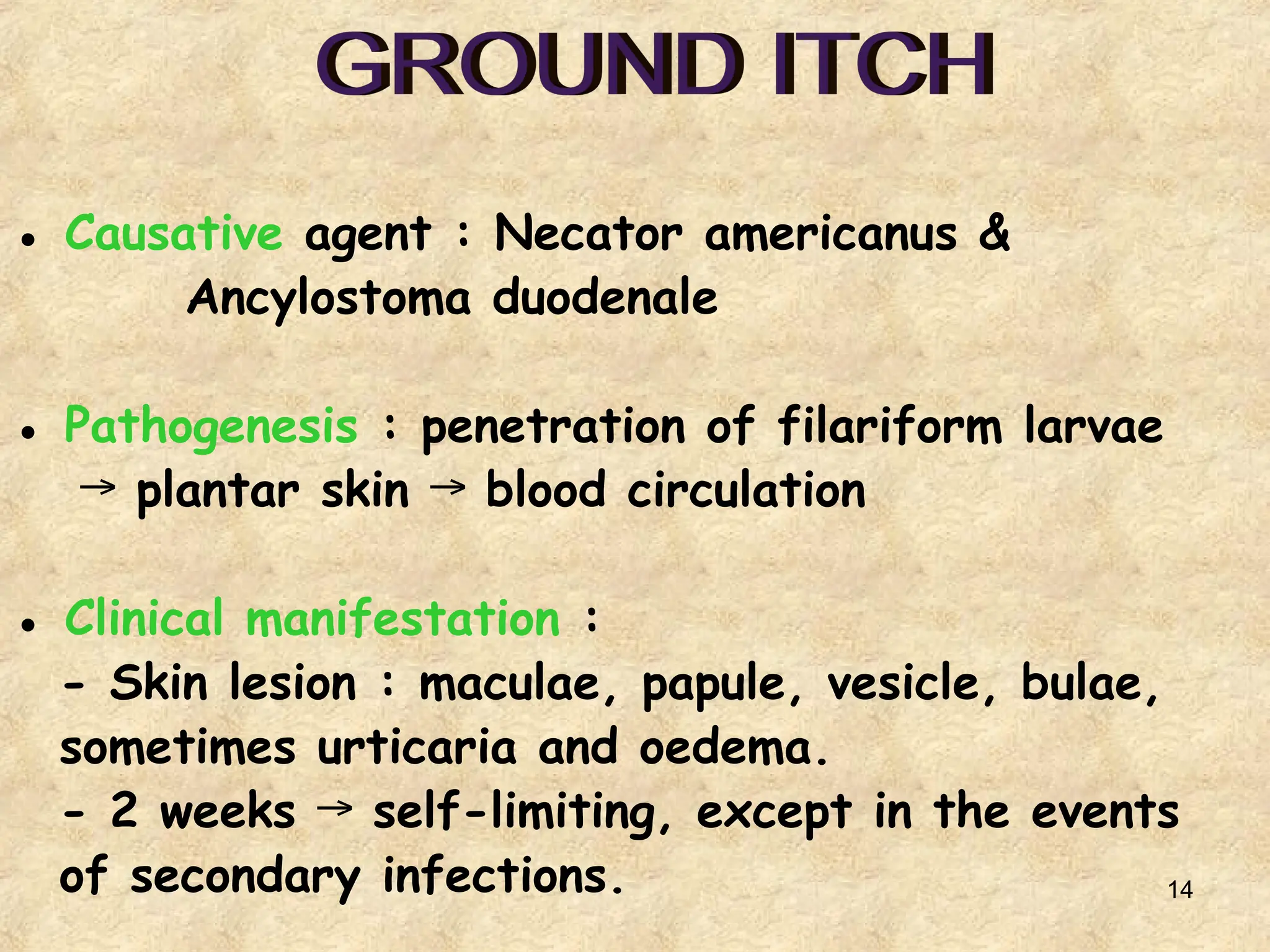
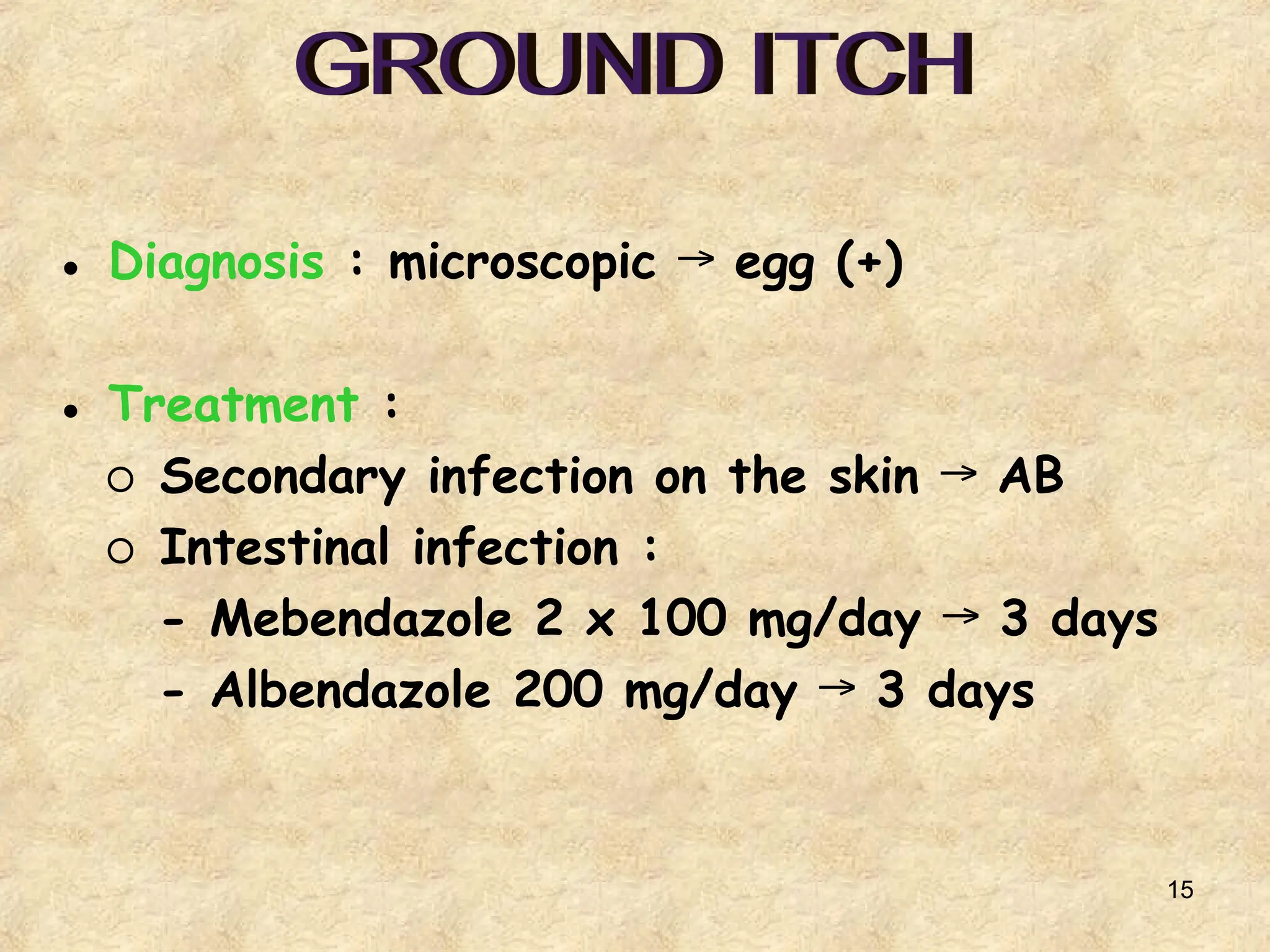
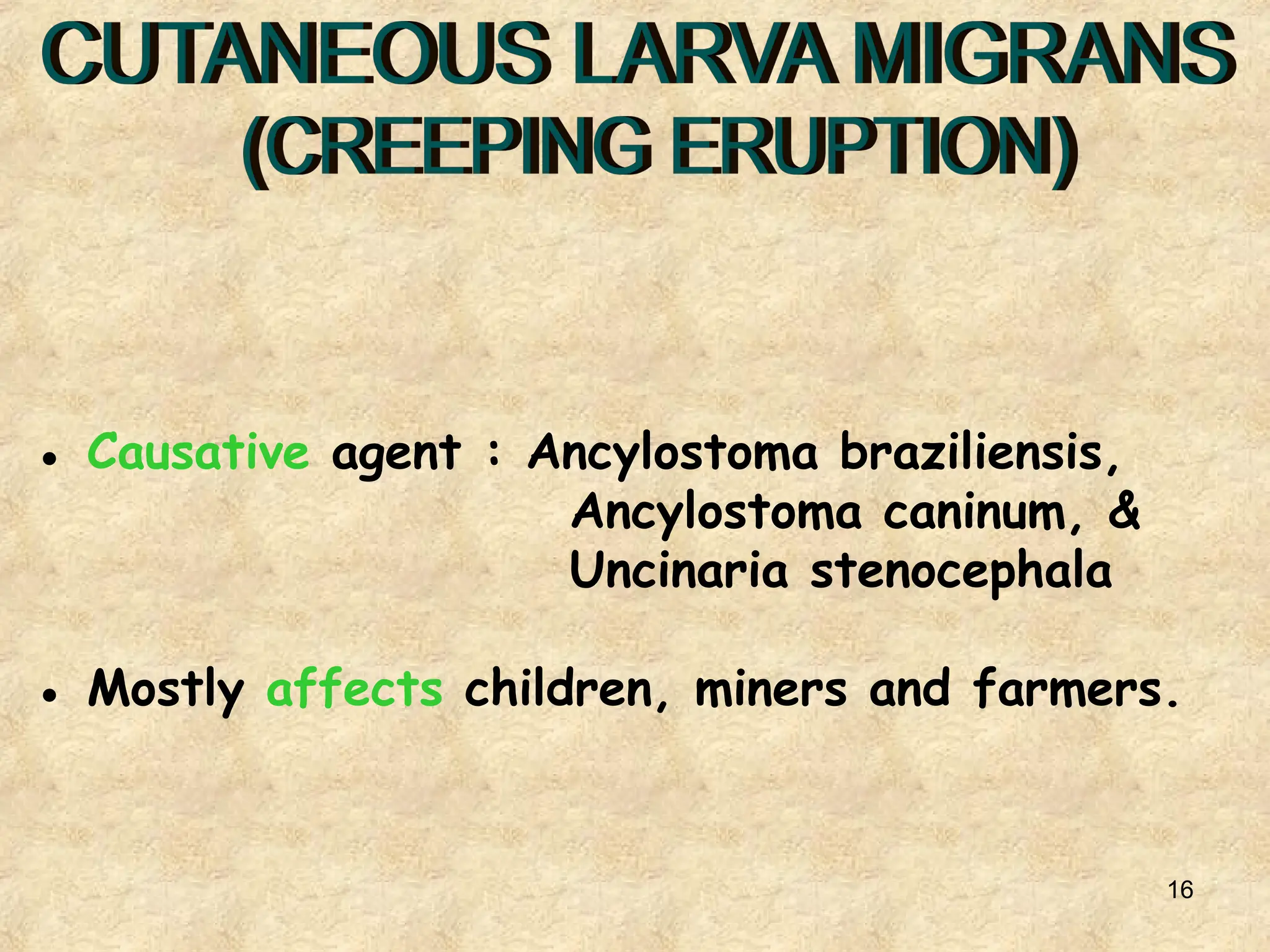
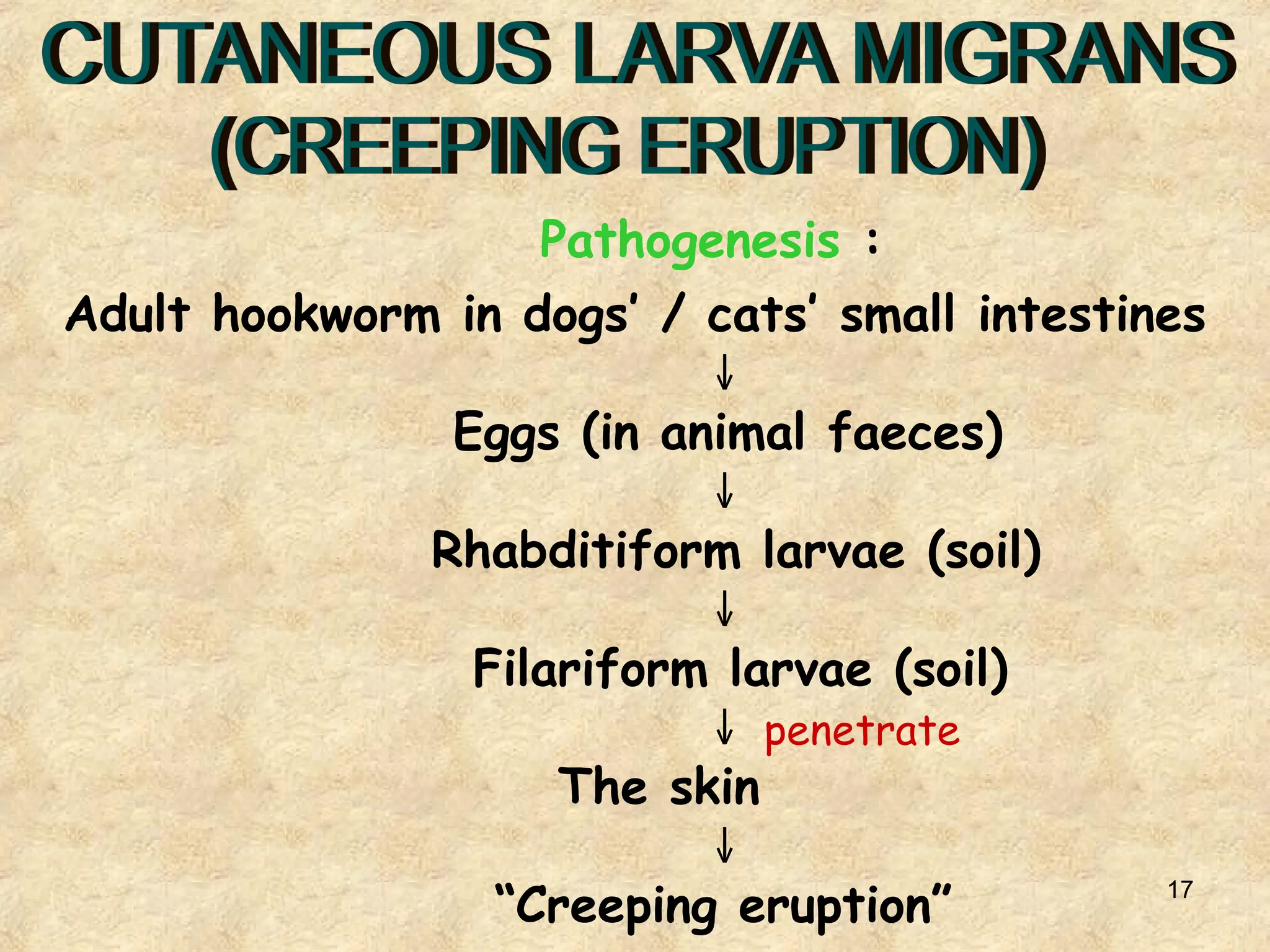
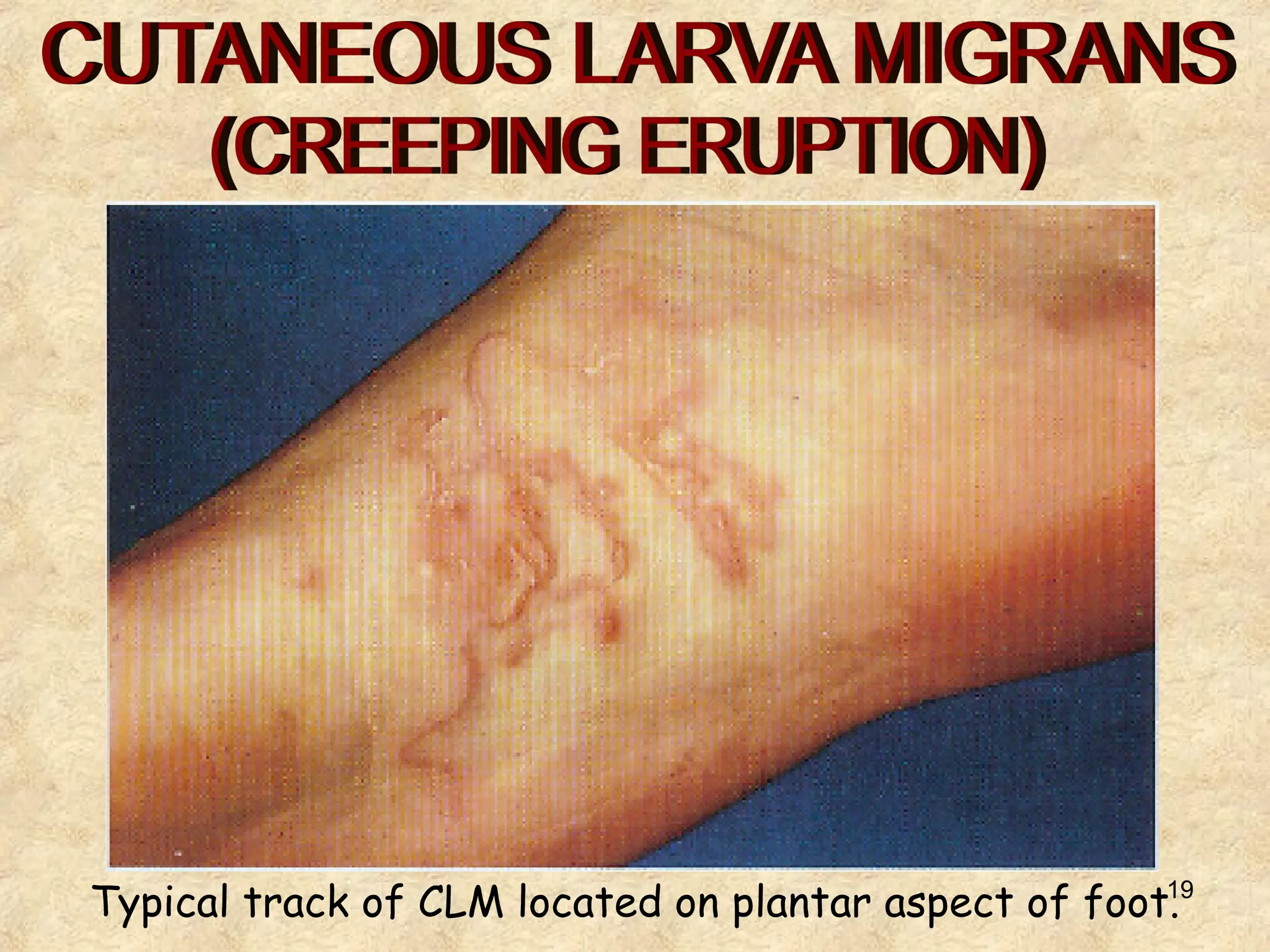
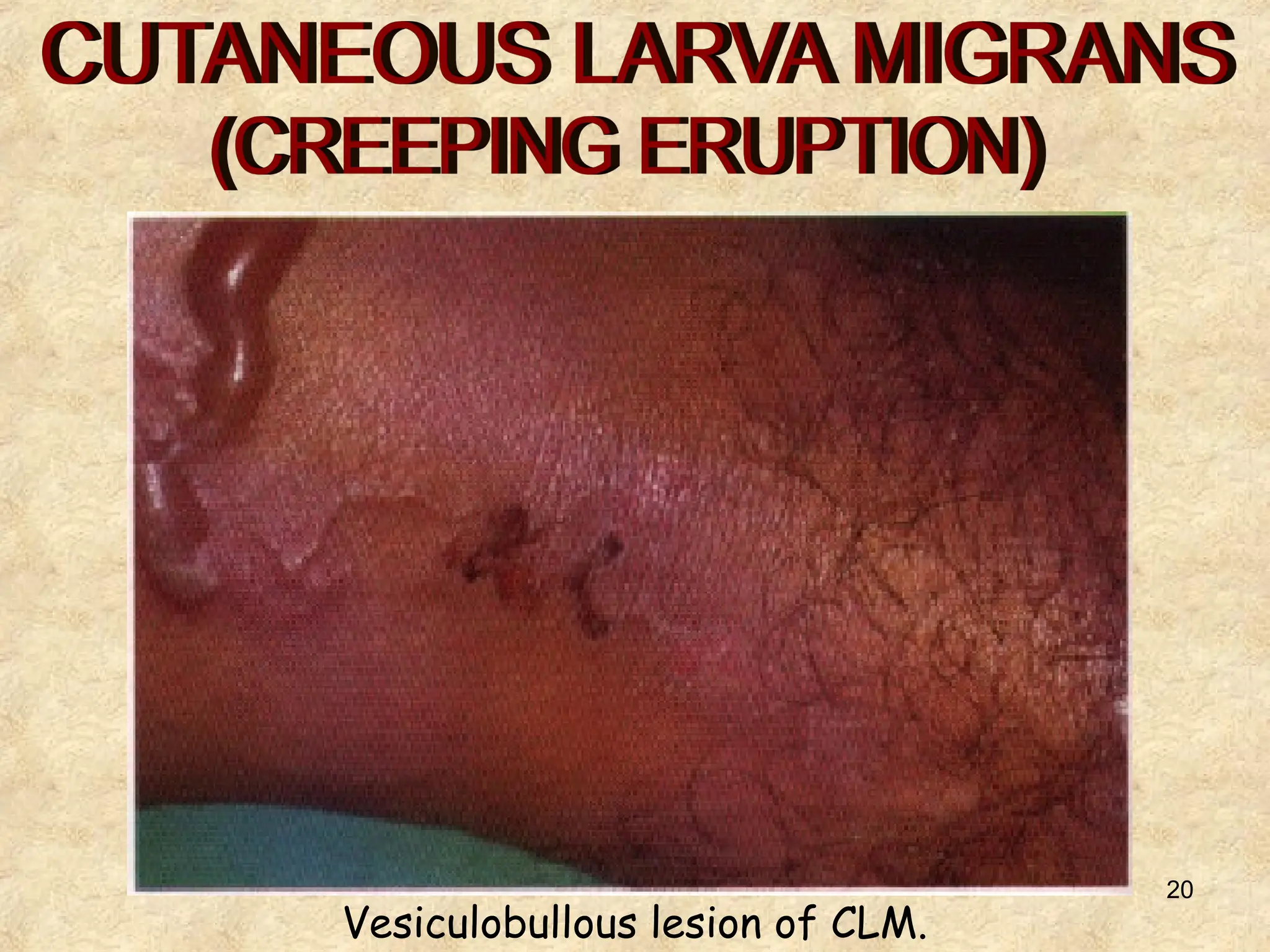
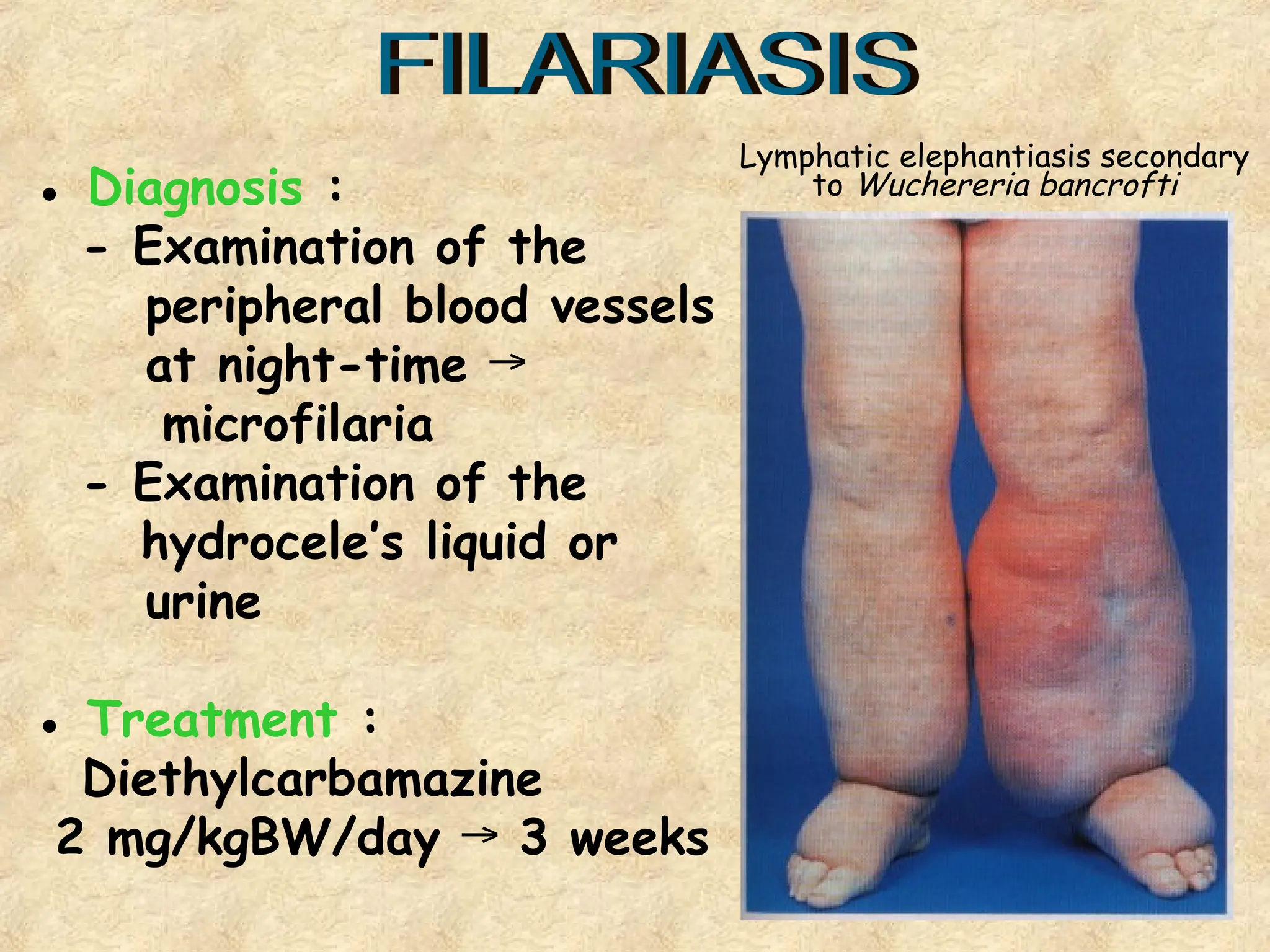
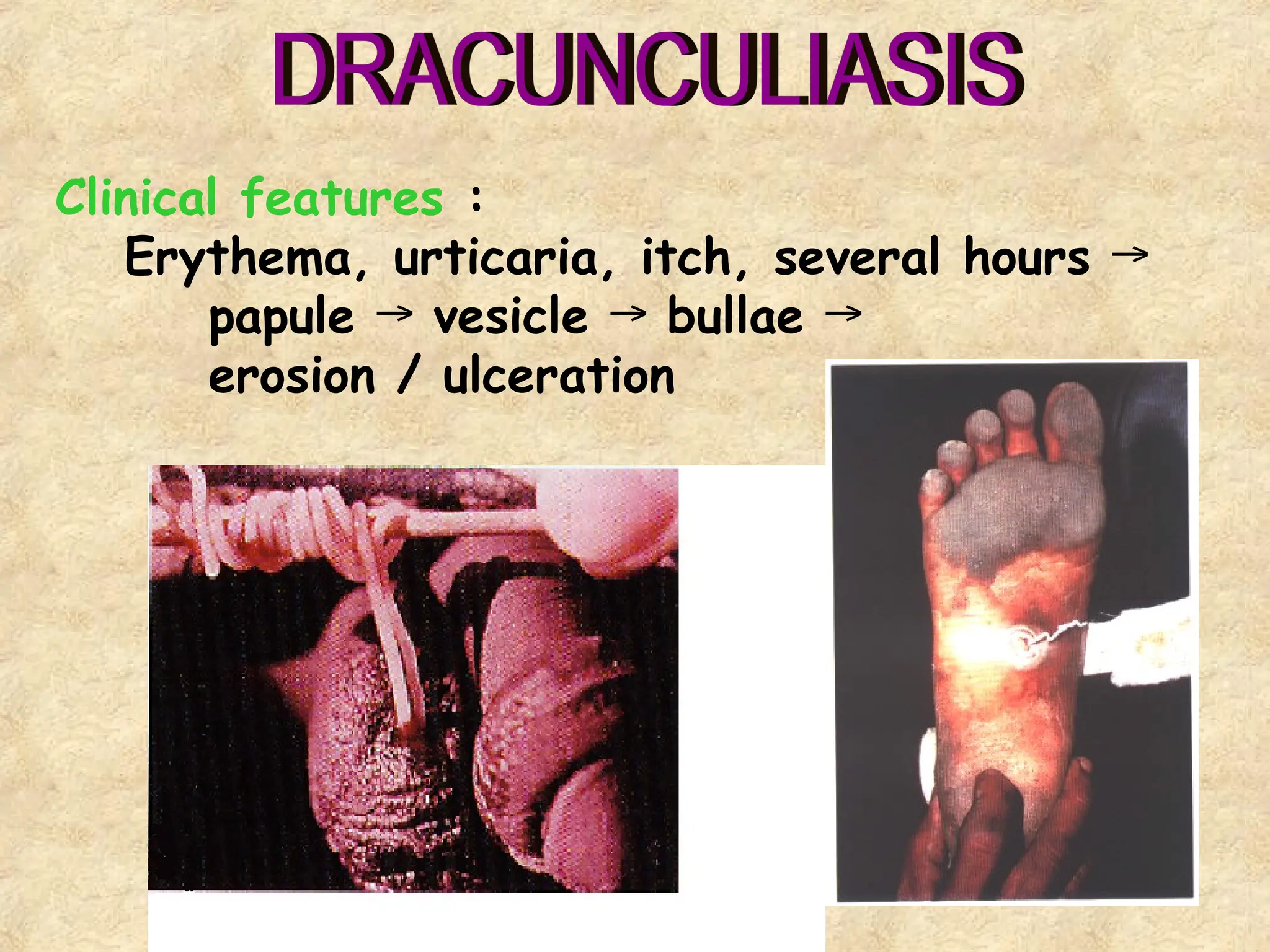
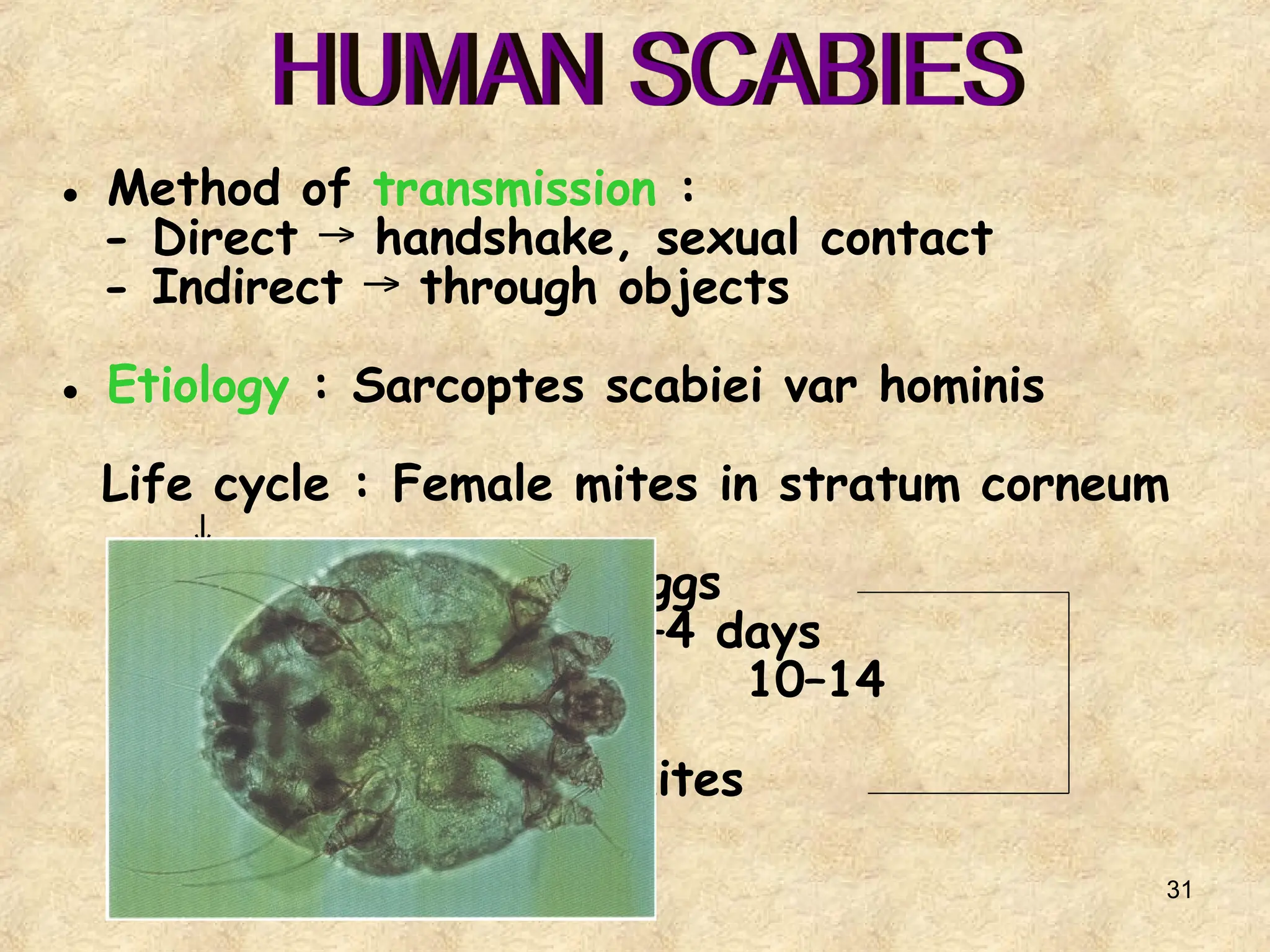
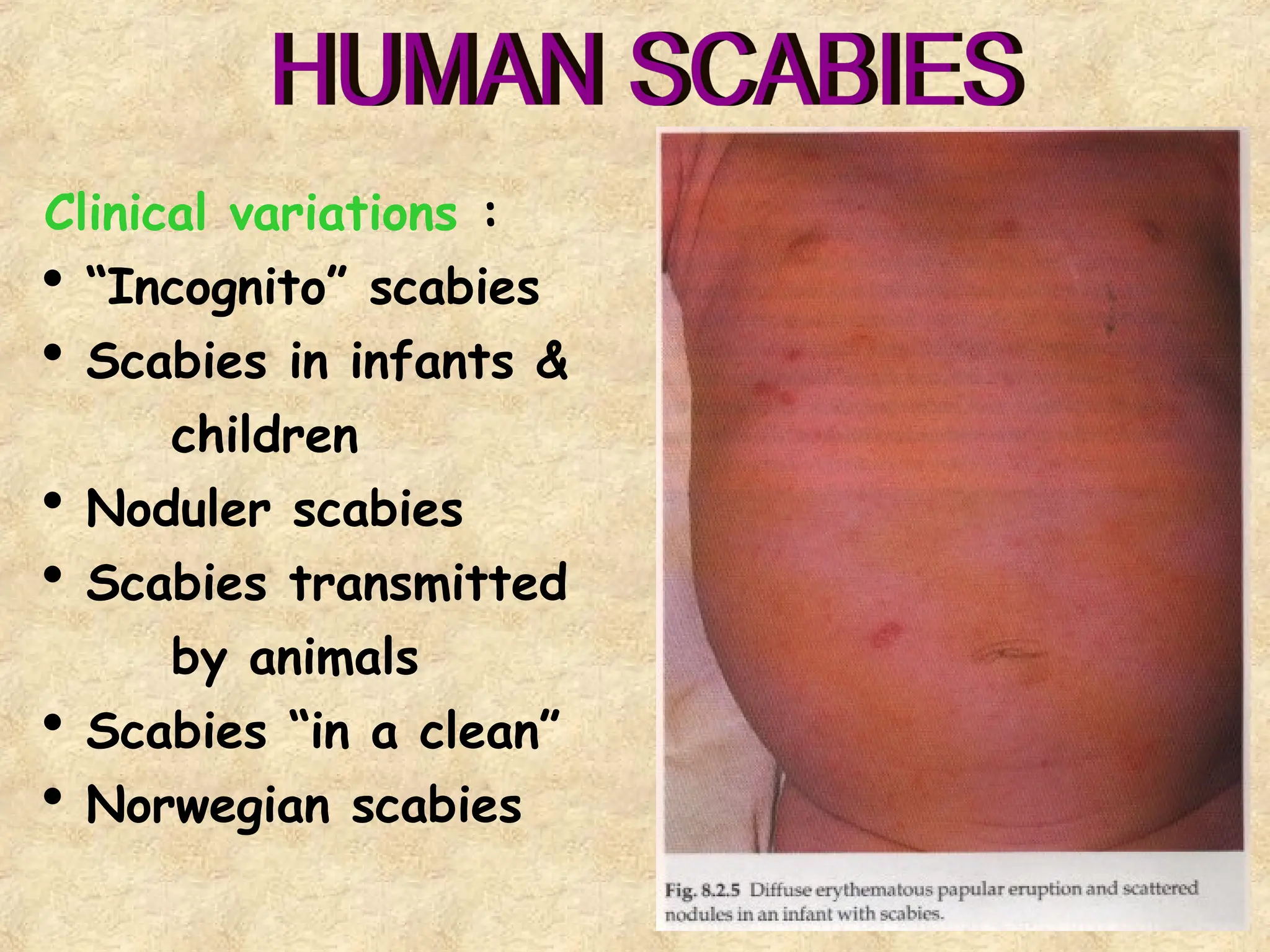
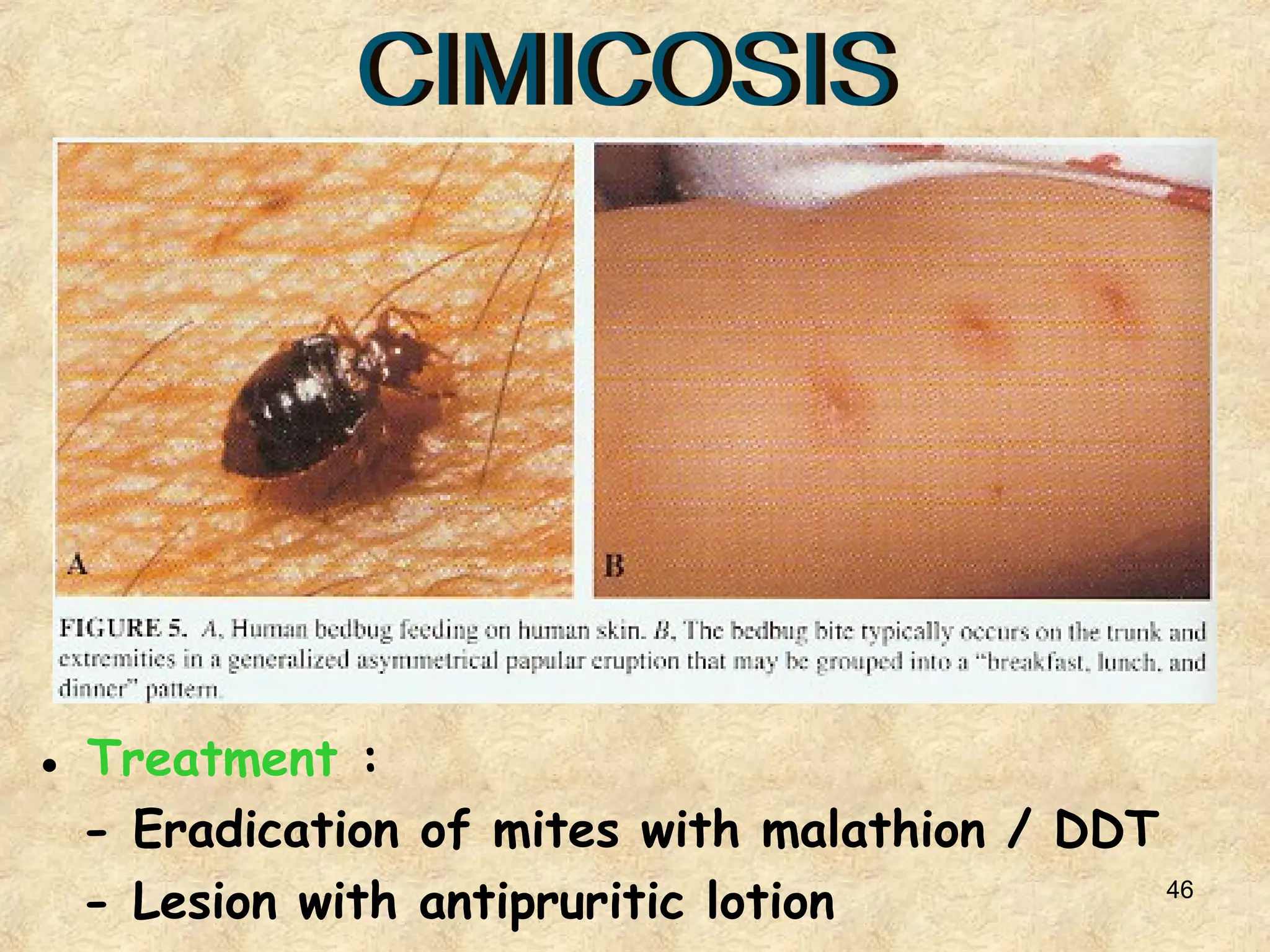
Dokumen membahas berbagai zoonosis yang disebabkan oleh parasit dan menekankan pentingnya diagnosis awal, pengobatan cepat, dan pendidikan kesehatan masyarakat untuk pencegahan. Jenis-jenis parasit yang dibahas termasuk protozoa, helminth, dan arthropoda, serta manifestasi klinis masing-masing infeksi. Pengobatan yang direkomendasikan mencakup metronidazole, mebendazole, dan lainnya tergantung pada infeksi spesifik yang terjadi.