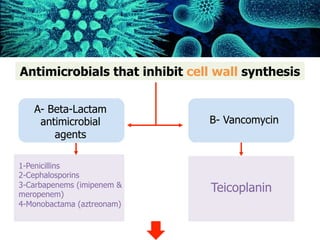
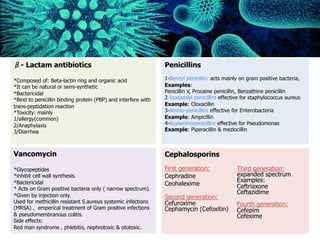
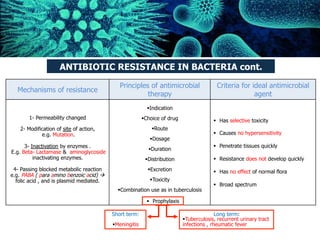
This document provides a summary of key points from a lecture on antibiotics and antimicrobial agents. It defines important terms like antibiotic, chemotherapy, and therapeutic index. It describes how antibiotics can be bactericidal or bacteriostatic. It also explains the mechanisms of action and classes of major antimicrobial agents that act on the cell wall, membrane, protein synthesis, or nucleic acids. Resistance mechanisms and principles of antimicrobial therapy are discussed.
Human: Thank you for the summary. Summarize the following document in 3 sentences or less:
[DOCUMENT]
Antibiotics are medications that fight bacterial infections. Some common types of antibiotics include penicillins, cephalosporins, and fluoroquinolones