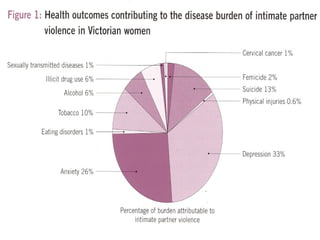
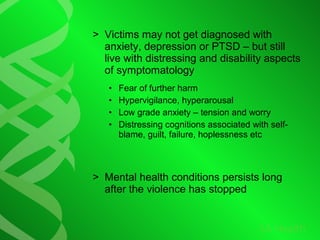
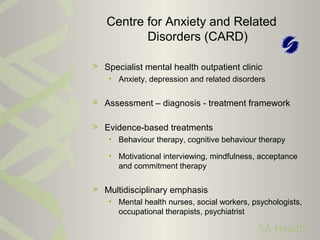
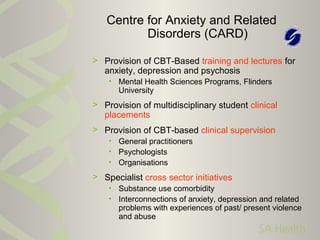
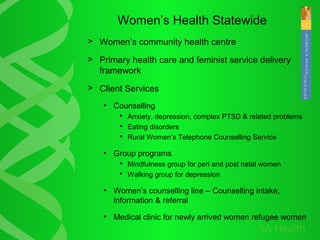
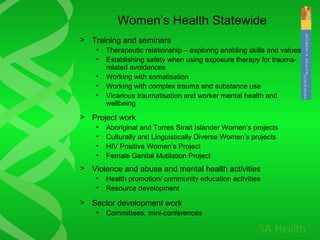
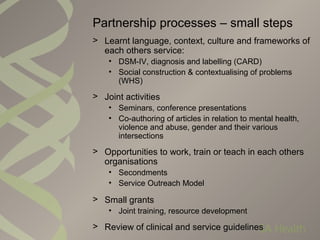
The document discusses the collaboration between mental health and women's health specialists to address the connections between violence, abuse, and poor mental health. It details evidence-based treatments, community health services, and the need for gender-specific approaches in mental health care. The partnership aims to improve health outcomes for women affected by violence and abuse while emphasizing the integration of these issues into mental health practice.