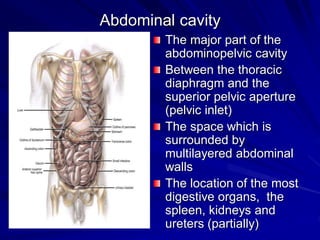
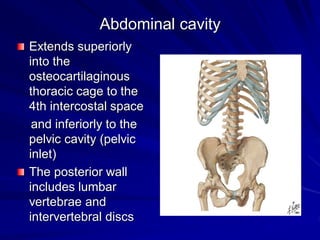
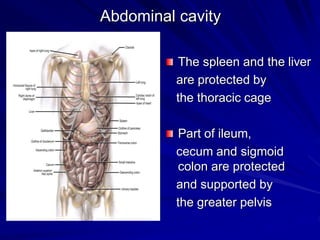
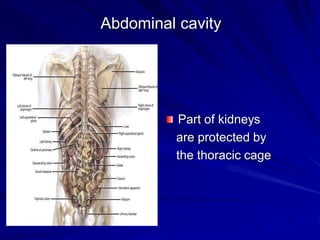
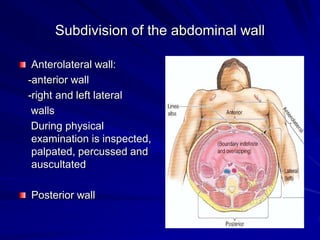
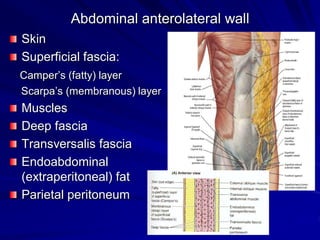
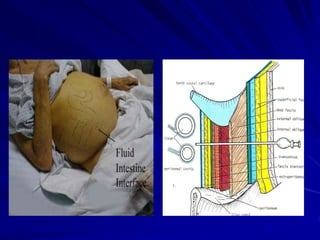
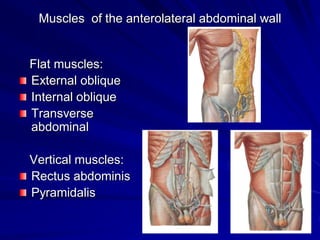
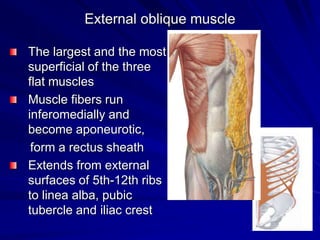
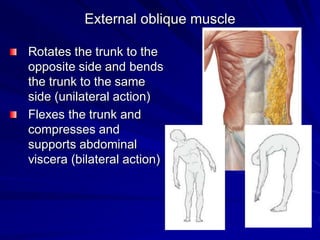
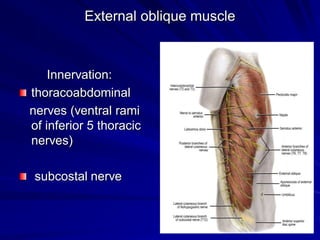
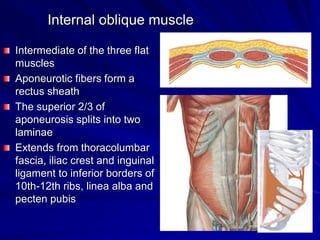
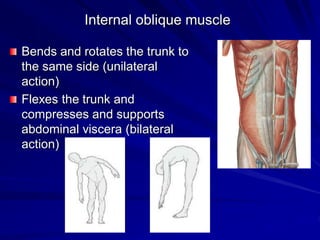
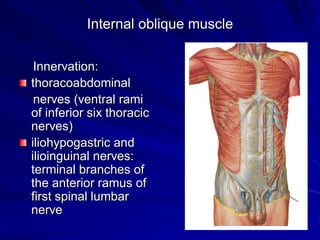
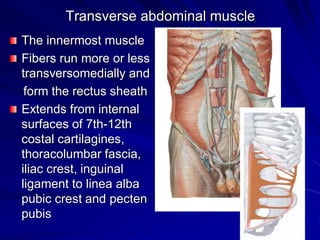
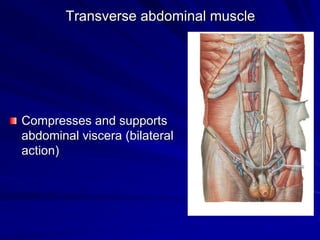
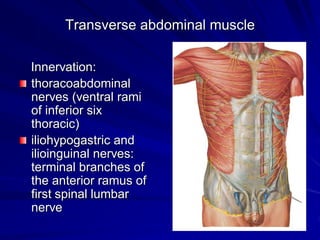
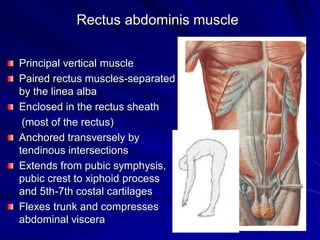
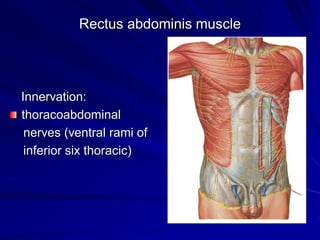
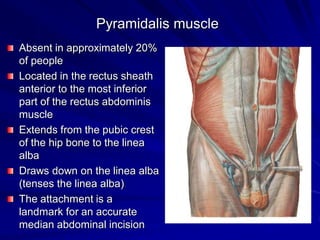
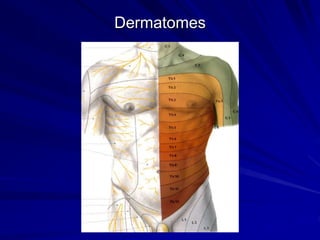
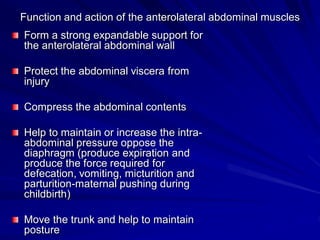
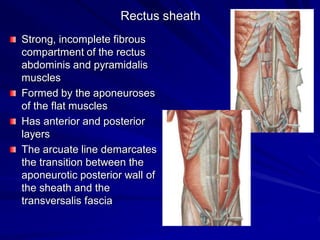
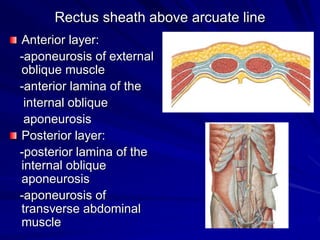
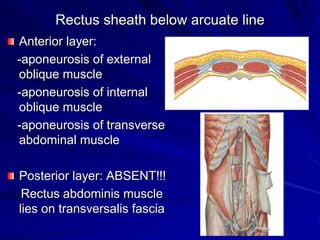
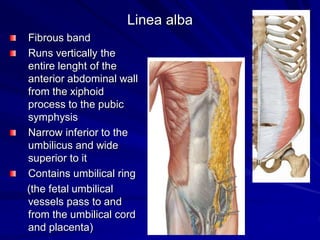
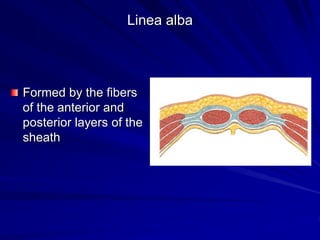
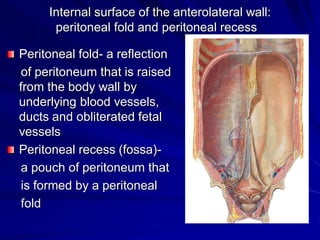
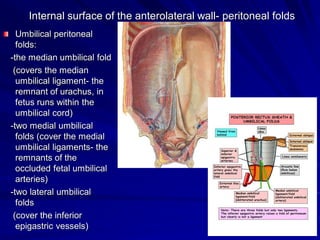
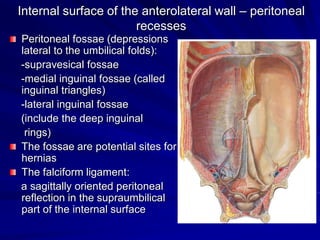
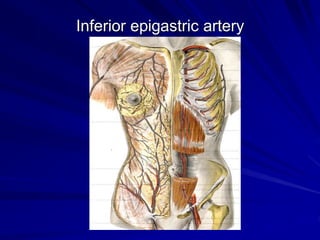
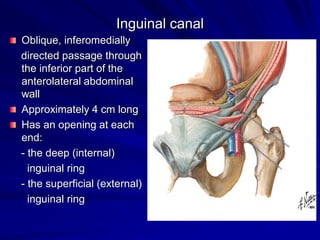
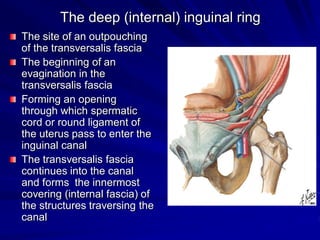
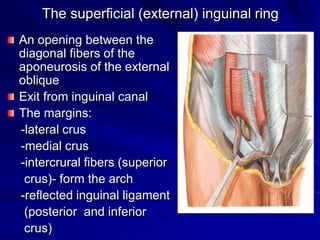
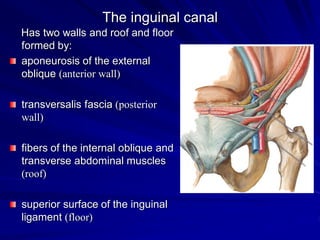
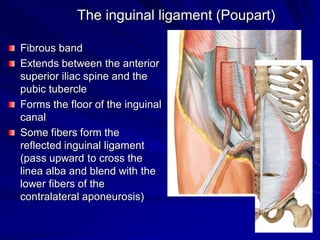
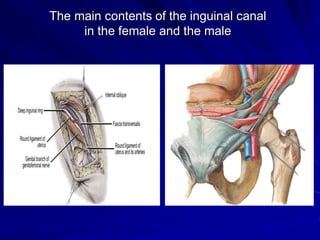
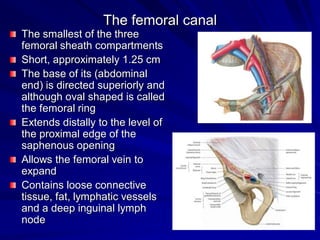
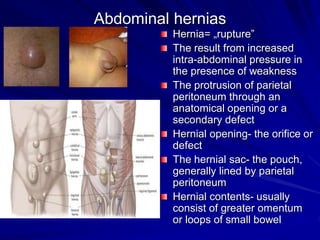
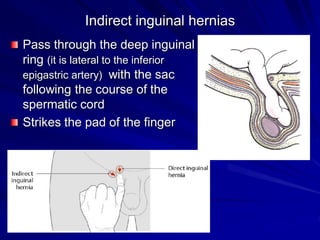
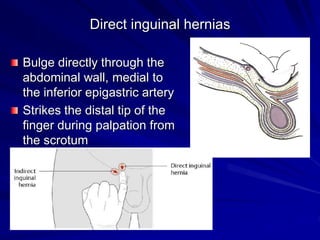
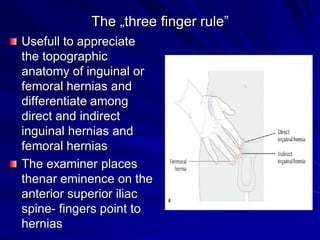
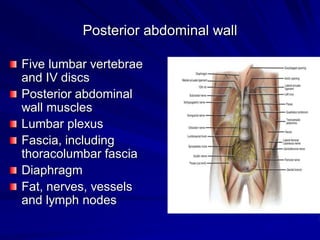
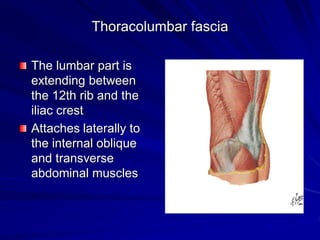
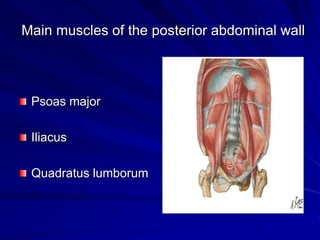
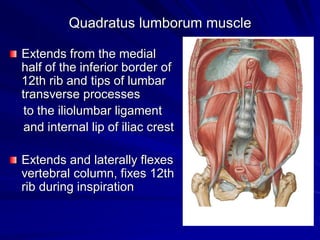
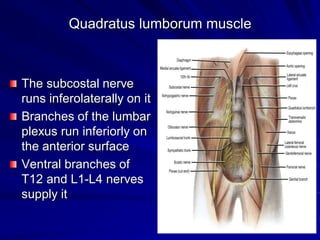
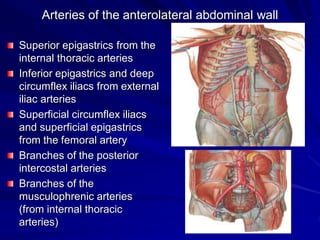
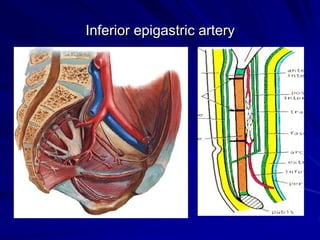
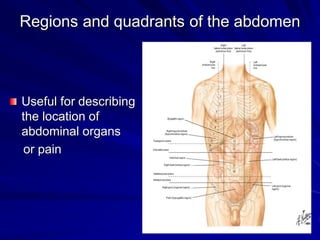
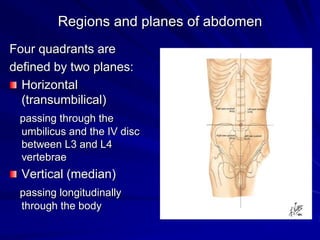
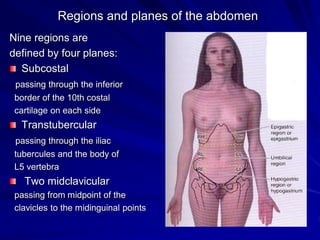
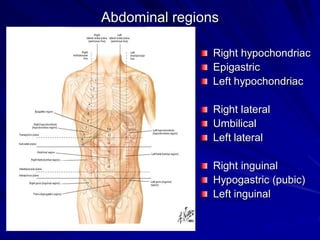
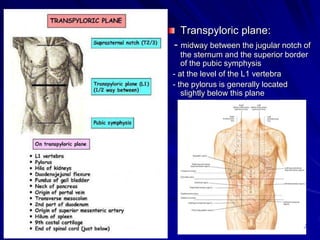
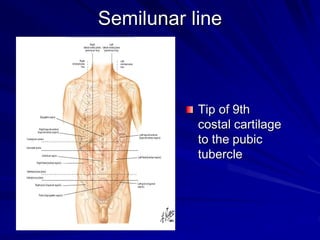
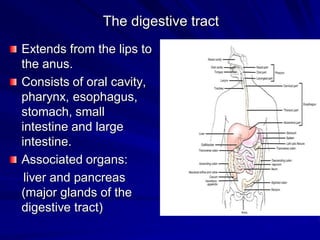
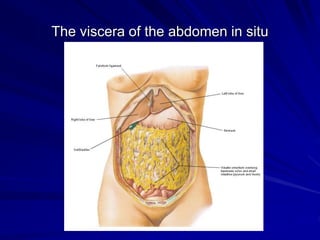
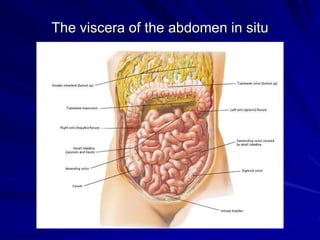
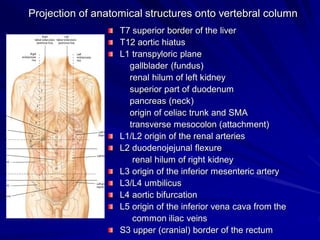
This document provides an overview of the abdominal cavity and abdominal wall. It describes the layers of the abdominal wall including muscles, fascia and peritoneum. It discusses the rectus sheath and linea alba. It details the inguinal canal and sites of hernias. It also summarizes the contents and regions of the abdominal cavity, as well as the arteries and veins of the abdominal wall. Key structures like the liver, stomach and intestines are located in relation to vertebral levels.