Breast Anatomy and Mammography Techniques
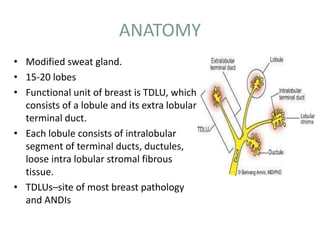
- 1. ANATOMY • Modified sweat gland. • 15-20 lobes • Functional unit of breast is TDLU, which consists of a lobule and its extra lobular terminal duct. • Each lobule consists of intralobular segment of terminal ducts, ductules, loose intra lobular stromal fibrous tissue. • TDLUs–site of most breast pathology and ANDIs
- 2. Mammography and Tomosynthesis • Dr Shamim Hyder Kalenchira
- 4. Lymphatic drainage • Axillary or lateral pathway – fed by Sappey’s Plexus, as well as by ducts satellite lymphatics and by most of the parenchymal lymphatics – this pathway runs around the inferior edge of the pectoralis major and reach the pectoral group of axillary nodes • internal mammary pathway – originates from both the lateral and medial halves of the breast and passes through the pectoralis major; connections may lead across the median plane and hence to the contralateral breast • retromammary pathway – comes from the posterior portion of the breast
- 5. Lymphatic drainage • Lymph of the breast drains as: – About 75% into axillary nodes(anterior group) – 20% ---- internal mammary nodes – 5% ---- posterior intercostal nodes • Internal mammary nodes drain the lymph not only from the inner half of the breast,but from the outer half as well there is a tendency for the lateral part of the breast to drain towards the axilla and the medial part to the internal mammary chain • Subareolar plexus of Sappey – plexus of lymph vessel present deep to the areola
- 7. MAMMOGRAPHY
- 8. Mammography equipment • Generator • Xray tube- fine focus of 0.2-0.5 mm with an additional 0.1mm focus for magnification. • Target- Molybdenum and rhodium. • Beryllium window-minimises absorption of radiation within the tube. • Molybdenum filter- by transmitting only characteristic radiation, absorbs unwanted radiation and forms a monoenergetic beam. • Compression device: 1-4mm thick plastic plate.
- 10. TARGET • The xray tubes are designed with tungsten, molybdenum , rhodium targets. • Tungsten target is operated under 30kVp with a 0.5 Aluminium filter- brehmsstrahlung and 12keV L-shell characteristic xrays. • Molybdenum target with Mo/Rh filter is more suitable for mammography. • Rhodium target filtered with Rh filter gives a similar spectrum as molybdenum. • Since the atomic number is higher, the brehmsstrahlung radiation is also higher than molybdenum.
- 11. FILAMENT • Positioned within a focussing cup with two focal spot sizes. • Filament types are either double wound/flat ribbon/ circular filament. • Focal spot size is very critical in mammography where high spatial resolution is required. • Small focal spot is used with small anode angle, which permits the use of high mA factors. • Usually the cathode is positioned towards the chest wall , which makes the patient positioning east and takes care of the heel effect.
- 12. FILTERS • Thin beryllium window or borosilicate glass window is used to reduce inherent filtration, since it offers low attenuation. • For a tungsten target x ray tube , Mo or Rh filter is recommended. • In case of rhodium target x ray tube , rhodium filter of 0.025 mm is used which gives high quality x rays with higher penetration. • Combination is suitable for thicker and dense breast imaging.
- 13. GRIDS • Stationary grids or grids placed in between the screen and the film are no longer used as the thin grid lines compromised on the quality of the image. • Covered tiny details such as micro calcifications. • Hence oscillating grids are used. • Grid ratio of 4:1 or 5:1. • The grid lines are eliminated by the motion of the grid. • Grids improve the image quality.
- 15. HEEL EFFECT • Shape of the breast requires higher intensity of radiation near the chest wall, to create uniform exposure to the screen film. • The cathode is positioned towards the chest wall and the anode is towards the nipple. • Permits easy positioning of the patient. • Increases the intensity of radiation near the chest wall, where greater penetration is needed. • The anode is often grounded with zero potential and the cathode is given higher potential.
- 17. Compression peddle • Decreases the thickness of the breast, thus reduces the scattered radiation- improves the contrast. • Decreases the kinetic blur. • Reduces the geometric unsharpness by homogenously bringing the object close to the film. • Makes the breast thickness uniform in film density. • Differentiates the easily compressible cysts and fibroglandular tissue from the more rigid carcinomas. • Separates the super imposed breast lesions. • Reduces radiation dose to the breast tissue.
- 18. • The compression device is parallel to the receptor surface. • Radiolucent plate that is flat and parallel to the support table. • Should match the cassette size.
- 19. Automatic exposure control • AEC system employs phototimers to measure the x ray intensity and quality. • Kept closer to the image receptor, to minimize the object to image distance- improves spatial resolution. Two types: - Ionization chamber type. - Solid state diode type.
- 20. SCREEN FILM SYSTEM • The x ray film should have high resolution and small grain size and used along with single intensifying screen • The emulsion surface of the film must face the screen. • Prevents loss of resolution due to light diffusion in the screen. • Gadolinium oxysulifde activated with terbium is used as screen phospor.
- 23. RADIOLOGICAL ANATOMY OF THE BREAST • Schematically, the radiological examination may show the following normal anatomical structures: – Skin – Nipple and areola – Fatty tissue – The breast tissue proper, or corpus mammae – Blood vessels
- 25. Mammography • Overall breast density reflects ratio between glandular elements (higher density) and fat (lower density); usually symmetric between breasts. • Fatty involution typically begins in lower-outer quadrant; progresses with age to upper-outer quadrant • American College of Radiology Breast Imaging and Reporting and Database System (BI-RADS) density categories A: Almost entirely fat B: Scattered fibroglandular densities C: Heterogeneously dense D: Extremely dense
- 27. NIPPLE-AREOLA COMPLEX AND SKIN • Normal skin thickness is usually < 2 mm • Dermal papillae often visible as grooves in nipple • Nipple usually everted • Should be seen in profile on at least one of two standard mammographic views • New nipple inversion requires diligent search for subareolar pathology, esp. if unilateral Can be caused by periductal mastitis, esp. bilateral
- 28. Imaging Approaches • Screening mammography – CC and MLO views of each breast – Additional views performed as necessary to include all glandular tissue • Diagnostic mammography – Examination is tailored to clinical question, – performed under direct supervision of radiologist – Any number of views are used to answer the question – • Is there a real abnormality? – • If finding is real, what is the morphology and level of suspicion for cancer? – Final assessment may require additional modalities, e.g., ultrasound or (rarely) MR – Report should conclude with a Bl- RADS final assessment and a management recommendation – Rare use of BI-RADS 0 if MR needed due to inconclusive mammogram and US, finding too vague to biopsy
- 29. Conventional Vs Digital Mammography • Researches have proven that digital is superior to film for women under the age of 50 and for women with dense breasts. • 25% less radiation to the patient • Ease of storing, sharing and manipulating electronic images
- 30. Mammography In digital mammography screen-film system has been replaced by Detectors to give the digital images Conventional
- 31. DIGITAL MAMMOGRAPHY • The stages in digital imaging : • Image capture by digital detector • Conversion of latent image into digital data set • Processing of image data • Display of processed image • Transmission and archival of data set
- 33. IMAGE ACQUISITION DEVICES • CHARGE COUPLE DEVICE TECHNOLOGY • Digital detectors consist of a phosphor, which is optically coupled to the CCD. • ADVANTAGE- The slit collimation of the X-ray beam results in a significant reduction in scatter. • This eliminates the need for a grid, leading to potential dose savings .
- 34. SELENIUM-BASED DETECTORS • Selenium based detectors consist of a thin layer of amorphous selenium deposited on the imaging plate. A uniform positive charge is built up on the surface of the selenium. • When X-ray photons strike the surface of the selenium, electrons are freed. • This leads to a partial discharge of the uniform surface charge pattern. • The degree of discharge reflects the local radiation exposure, leadingto a latent image in the form of a charge distribution pattern. • This charge pattern is then “read” and the resultant electrical signal digitised.
- 35. ADVANTAGES OF DIGITAL MAMMOGRAPHY 1. Acquired in less than a minute as compared to conventional mammography . 2. Spot view digital systems are available to help guide breast biopsy . 3. Superior contrast resolution especially in dense breast tissues 4. Offers the possibility of three dimensional breast tomography using relatively low doses .
- 37. Standard views: 45* Medio lateral Oblique (MLO view)/ Lundgren’s view Craniocaudal view (CC view) RCC RMLO LCC LMLO Left Craniocaudal Right Craniocaudal Right Mediolateral Oblique Left Mediolateral Oblique
- 38. Cranio caudal view • The casette is placed under the breast at the level of the inframammary fold. • The breast is then pulled until the inframammary fold is taut. • Compression is applied and x ray beam is directed vertically from above. • Postero medial aspect should also be included.
- 40. Mediolateral oblique view • Best view to image all of the breast tissue and the pectoral muscle. • The C arm of the mammographic unit is rotated to 45 degree so that the cassette is parallel to the pectoral muscle. • The film holder is kept high up in the axillary fossa and the patients arm is abducted at the elbow by 80 degrees. • The x ray beam enters the breast from the medial side- compression is applied to the pectoralis major muscle.
- 42. LAT Left Axillary Tail LCV Left Cleavage LFB Left From Below LLMO Left Lateromedial Oblique LML Let Mediolateral LRL Left Roll Lateral LRM Left Roll Medial LLM Left Lateromedial
- 43. MAMMOGRAPHIC SIGNS • The detection and identification of elementary mammographic signs form the basis for correctly interpreting breast pathologies and describing them accurately in the mammographic report. • The specific features are the basis for classifying the lesions as either benign or malignant. These features define the positive predictive value (PPV)
- 44. Mammographic signs can be described in terms of: – Opacity (mass) – Architectural distortion – Calcifications – Radiolucency – Asymmetry – Focal asymmetry – Skin thickening and retraction – Oedema and trabecular thickening – Asymmetrically dilated ducts
- 45. OPACITY • Definition – A space-occupying lesion visible in two projections, implying the concept of mass and volume. – An alteration visible in just one projection can be described as a density or focal asymmetry. • Shape: oval (may include 2 or 3 lobulations), round or irregular • Margins: circumscribed, obscured, microlobulated, indistinct, spiculated • Density: high, equal, low or fat-containing.
- 47. • The margin of a lesion can be: • Circumscribed (historically well-defined). This is a benign finding. • Obscured or partially obscured, when the margin is hidden by superimposed fibroglandular tissue. • Microlobulated. This implies a suspicious finding. • Indistinct (historically ill-defined). This is also a suspicious finding. • Spiculated with radiating lines from the mass is a very suspicious finding.
- 49. • The density of a mass is related to the expected attenuation of an equal volume of fibroglandular tissue. High density is associated with malignancy. It is extremely rare for breast cancer to be low density.
- 51. ARCHITECTURAL DISTORTION • The term architectural distortion is used, when the normal architecture is distorted with no definite mass visible. This includes thin straight lines or spiculations radiating from a point, and focal retraction, distortion or straightening at the edges of the parenchyma.. • Architectural distortion can also be seen as an associated feature. For instance if there is a mass that causes architectural distortion, the likelihood of malignancy is greater than in the case of a mass without distortion. • Classification – Marginal – Intra-parenchymal distortion.
- 52. Notice the distortion of the normal breast architecture on oblique view (yellow circle) and magnification view.
- 53. CALCIFICATIONS • Definition – Calcifications are amorphous, radiopaque, acellular entities produced by calcium deposits. – They reflect the secretory or degenerative processes of the breast. Malignant calcifications may be caused either by cellular secretion or by calcification of necrotic cancer cells. – Calcifications are among the most frequent mammographic signs and can also be amongst the most difficult to define and interpret. • In relation to their site of origin, calcifications are classified as – Intraductal – Lobular • Evaluation – Shape – Distribution – Site – Size – Number
- 54. • Lobular calcifications: This results in uniform, homogeneous and sharply outlined calcifications, that are often punctate or round. When the acini become very large, as in cystic hyperplasia, 'milk of calcium' may fill these cavities. • Intraductal calcifications: form a complete cast of the ductal lumen. This explains why they often have a fine linear or branching form and distribution. Intraductal calcifications are suspicious of malignancy and are classified as BI-RADS 4 or 5.
- 57. .
- 59. Suspicious morphology • Amorphous (BI-RADS 4B) So small and/or hazy in appearance that a more specific particle shape cannot be determined. • Coarse heterogeneous (BI-RADS 4B) Irregular, conspicuous calcifications that are generally between 0,5 mm and 1 mm and tend to coalesce but are smaller than dystrophic calcifications. • Fine pleomorphic (BI-RADS 4C) Usually more conspicuous than amorphous forms and are seen to have discrete shapes, without fine linear and linear branching forms, usually < 0,5 mm. • Fine linear or fine-linear branching (BI-RADS 4C) Thin, linear irregular calcifications, may be discontinuous, occasionally branching forms can be seen, usually < 0,5 mm.
- 61. Distribution of calcifications • The arrangement of calcifications, the distribution, is at least as important as morphology. These descriptors are arranged according to the risk of malignancy: • Diffuse: distributed randomly throughout the breast. • Regional: occupying a large portion of breast tissue > 2 cm greatest dimension • Grouped (historically cluster): few calcifications occupying a small portion of breast tissue: lower limit 5 calcifications within 1 cm and upper limit a larger number of calcifications within 2 cm. • Linear: arranged in a line, which suggests deposits in a duct. • Segmental: suggests deposits in a duct or ducts and their branches.
- 63. • Site: Before starting to analyse calcifications, it is advisable to ascertain that calcifications are truly intra-mammary, to rule out skin or pseudocalcifications due to artifacts. • Size: Many different dimensions are reported, but calcifications associated with malignancies are generally between 0.5 and 2 mm, though often even smaller. • Number: There is no consensus . The number of calcifications must be evaluated together with their morphology and distribution.
- 64. RADIOLUCENCY • A sharp-edged radiolucent mass may be seen/ with a radiopaque rim that is generally complete or only partly broken. Varying in size and sometimes occupying the whole breast. • These may be round, oval or more rarely lobulated. • They are usually caused by lipomas/ pseudolipomas and foci of fat necrosis.
- 66. ASYMMETRIC BREAST TISSUE • Significant areas of fibroglandular tissue on one side that appear different compared with the contralateral breast, because they are either of greater extent or of higher density. If there are no other abnormalities, this is simply a normal variant of breast structure.
- 67. FOCAL ASYMMETRY • Areas of glandular tissue without the characteristics of a true mass, but recognizable with similar appearance in the craniocaudal , lateral and oblique projection. • These may simply be normal local asymmetries but further investigation is justified, with targeted magnification views and if necessary ultrasound.
- 68. SKIN THICKENING AND RETRACTION • Skin thickening and retraction can be diffuse or focal. Skin thickening or even ulceration can occur as a result of tumor direct invasion or through thickening and retraction of Coopers ligaments. • Skin changes can result from a contiguous malignancy, infection or inflammation, primary skin disorders, lymphatic or vascular obstruction. and systemic diseases affecting the skin. • Post-surgical scarring and fat necrosis can also cause skin thickening and retraction.
- 69. • A high density, stellate opacity with radiating spicules into the surrounding parenchyma is seen in the inner subareolar location with thickened and retracted overlying areolar skin.
- 70. OEDEMA • Diffuse oedema causes generalized thickening of the trabecular stromal net. There may also be thickening of the skin. • This finding is typical of benign processes such as mastitis, post-radiotherapy changes and congestive heart failure secondary to kidney failure. • Thickened skin also invariably accompanies inflammatory carcinoma in which a focal opacity may be visible mammographically. • Post-therapy follow-up may be advisable in these cases to permit a differential diagnosis.
- 71. ASYMMETRICALLY DILATED DUCTS • Linear, ribbon-like, tubular or branching, single or multiple opacities, parallel and radiating in the retroareolar space. • This appearance is typical of ectactic ducts and, less commonly, of intraductal papilloma or carcinoma.
- 72. BI-RADS - Breast Imaging Reporting and Data System • BI-RADS 0: Screening mammogram with finding for which additional evaluation is needed – Also known as recall or call-back • BI-RADS 1: Negative mammogram • Bl-RADS 2: Mammogram with a benign finding • Bl-RADS 3: Mammogram with a probably benign finding, for which short-interval follow-up suggested
- 73. • BI-RADS 4: Mammogram with a suspicious abnormality for which biopsy should be considered • BI-RADS 5: Mammogram with a finding highly suggestive of malignancy, for which appropriate action should be taken • BI-RADS 6: Mammogram with a known biopsy-proven malignancy, for which appropriate action should be taken
- 76. Breast Ductography • Helps define the cause of unilateral, single- pore, spontaneous nipple discharge. • Allows diagnosis of the underlying condition, definition of the extent of disease, identification of central and peripheral lesions, and guidance of surgical excision. • It involves cannulation of the discharging duct, injecting contrast material within and obtaining 90 degree and craniocaudal views.
- 77. Normal ductogram
- 78. In this patient, contrast outlines (single arrows) a duct that is wider than normal (dilated), and the contrast column is disrupted by the presence of a tumor (double arrow). About half of the patients presenting with spontaneous nipple discharge are found to have papillomas, which are benign, non-cancerous tumors. The tiny, blunt- tipped needle used to inject the contrast is seen at the edge of the film (wide arrow).
- 79. Breast tomosynthesis • Modification of a digital mammography unit to enable the acquisition of a three-dimensional (3D) volume of thin-section data. • Images are reconstructed in conventional orientations by using reconstruction algorithms similar to those used in computed tomography (CT). • Reduces or eliminates tissue overlap.
- 80. In breast tomosynthesis, a moving x-ray source and a digital detector are used.
- 81. • The X-ray tube makes an arc, during which is acquired a series of images, each of which is delivered a dose equal to a fraction of that provided in a standard mammogram. During the acquisition any detector element receive in time sequence related information on each object volume element. The set of digital projections thus contains a complete structural information on all the object layers in the form of raw data
- 82. • Acquisitions may be performed either with the step-and-shoot method or with a continuous exposure method. • The image data are sent from the acquisition workstation to the reading workstation. Images are reconstructed by using a mathematical algorithm similar to those used in CT reconstructions, to generate a set of thin image sections parallel to the breast platform
- 84. • Tomosynthesis, therefore, does not provide direct projection images, but reconstructed images of any individual layers through several available algorithms, more or less efficient, each aimed to removing from reconstructed slice the upper and lower layers "structured noise". • DBT allows the detection of a greater number of expansive lesions and a better morphological analysis of masses and architectural distortions, thanks to the contrast of findings greater than the background, given by the more shade structures belonging to the upper and lower layers, and then to the smaller amount of noise. It is thus exceeded one of the limits of two-dimensional imaging, which is the masking of lesions caused by superimposition of normal structures.
- 85. • A further advantage of DBT is given by the lack of need for operator training (the breast is positioned just like a conventional mammography in MLO and / or CC projection) and for the radiologist (as he continues to perform diagnosis from images with mammograms features).
- 86. Comparison of screening mammography with breast tomosynthesis in a 57-year-old woman. (a) Digital mammogram shows a mass (arrows) in the lower outer part of the left breast. The mass is not clearly visible because of surrounding dense tissue. (b) Breast tomosynthesis image provides clearer depiction of the mass (arrows), which is well circumscribed.
- 87. Invasive ductal carcinoma in a 45-year-old woman with a lump in the left breast for 6 months. (a) Digital mammogram clearly shows an oval-shaped relatively well- circumscribed primary mass. (b) Breast tomosynthesis image provides better depiction of the microlobulated, spiculated border of the mass (arrows), a finding suggestive of malignancy.
- 88. Computer-Aided Detection • CAD programs are commercially available systems that use computer software to assist the mammographer in detecting or identifying potentially suspicious abnormalities on a mammogram. • The CAD program identifies potential abnormalities on the images and marks areas on the study that the computer considers to be suspicious. • The radiologist reviews the flagged areas to assure that nothing was missed. • DM readily provides images that can be used with CAD. Film screen mammography has to be digitized in order for CAD to be performed.
- 90. Bibliography • Bi-RADS for Mammography and Ultrasound 2013 Updated version Harmien Zonderland and Robin Smithuis • Diagnostic Radiology: Musculoskeletal and Breast Imaging by Berry Manorama, Chowdhury Veena, Mukhopadhyay Sima, and Suri Sudha