Diabetes Care Module
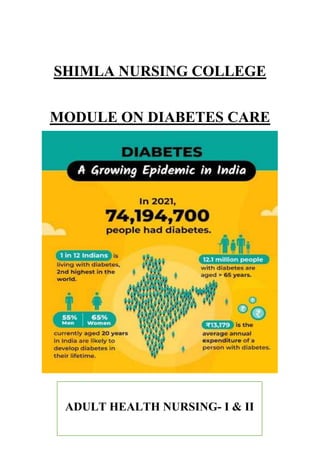
- 1. SHIMLA NURSING COLLEGE MODULE ON DIABETES CARE ADULT HEALTH NURSING- I & II
- 4. DIABETES CARE MODULE - 6 SESSIONS WITH CONTENT
- 5. SESSION -1 INTRODUCTION The earlist known record of diabetes was written on 3rd Dynasty Egyptian Papyrus by Physician ‘Hesy- Ra’. He started recurring urination as a sign of this illness. The Indian physician Sushruta in the 6th century B.C. noticed the sweet nature of urine in such patients and termed the condition MADHUMEHA. As per Indian Council of Medical Research – India Diabetes (ICMR INDIAB) study published in 2023, the prevalence of diabetes is 10.1 crores. Responding to the increasing burden of diabetes around the world, the World Health Organization has launched the Global Diabetes Compact. The launch coincides with the 100th anniversary of the discovery of insulin. The WHO Global Diabetes Compact has the vision of reducing the risk of diabetes, and ensuring that all people who are diagnosed with diabetes have access to equitable, comprehensive, affordable and quality treatment and care. The work undertaken as part of the Compact will also support the prevention of type 2 diabetes from obesity, unhealthy diet and physical inactivity. The WHO Global Diabetes Compact was launched at a Global Diabetes Summit, co-hosted by the World Health Organization and the Government of Canada, with the support of the University of Toronto, on 14 April 2021. Diabetes is one of the top five leading causes of death in most developed countries and substantial evidence is accumulating to suggest that it
- 6. will reach epidemic proportions in developing and newly industrialised countries [1]. It has been estimated that 2.1% of the world population may have diabetes, predicted to rise to 3% by the year 2010 [2]. The World Health Organisation (WHO) predict that the current diabetic population of 177 million (estimate 2000) people will increase to 370 million by the year 2030 [3]. Diabetes has become a major health issue in South-East Asia. It has been estimated by the International diabetes federation (IDF) that 23 million people currently have diabetes, which accounts for a sixth of the world's diabetic population. India has the largest diabetic population and one of the highest diabetes prevalence rates in the world. The prevalence rates for type 2 diabetes in India are still increasing sharply with the number of sufferers predicted to rise from 19.4 million in 1995 to 80.9 million in 2030 The number of people with diabetes rose from 108 million in 1980 to 422 million in 2014. Prevalence has been rising more rapidly in low- and middle-income countries than in high-income countries. Diabetes is a major cause of blindness, kidney failure, heart attacks, stroke and lower limb amputation. Between 2000 and 2019, there was a 3% increase in diabetes mortality rates by age. In 2019, diabetes and kidney disease due to diabetes caused an estimated 2 million deaths. A healthy diet, regular physical activity, maintaining a normal body weight and avoiding tobacco use are ways to prevent or delay the onset of type 2 diabetes. Diabetes can be treated and its consequences avoided or delayed with diet, physical activity, medication and regular screening and treatment for complications. DIABETES is a group of metabolic disease characterized by hyperglycemia resulting from defect in insulin secretion, insulin action or both. Globally: 382 million people had diabetes in 2013, by 2035 this number will rise to 592 million. India: 65.1 million people had diabetes in 2013, by 2035 this number will increase by 70.6%. The adult pancreas is a transversely oriented retroperitoneal organ extending from the “C” loop of the duodenum to the hilum of the spleen.
- 7. Exocrine Secretions: Pancreatic juice enzymes promote the digestion of carbohydrates, proteins and fats. Endocrine secretion: Insulin and glucagon-enter portal vein-transported directly to the liver-regulate metabolism of carbohydrates, proteins, and fats. 15-20% alpha cells synthesize and secrete GLUCAGON 70-80% beta cells synthesize and secrete INSULIN 1-8% delta cells synthesize and secrete STOMATOSTATIN and GASTRIN 1-2% F-cells Secrete PANCREATIC POLYPEPTIDE which decreases the absorption of food from the GIT Polypeptide hormone Produced by Beta cells of islets of Langerhans of pancreas. Insulin is a protein made of 2 chains-alpha and beta. Anabolic hormone Regulation of insulin secretion: Factors stimulate insulin secretion: Glucose, Amino acids, Gastrointestinal hormones. Factors inhibit insulin secretion: Epinephrine Action of insulin Stimulate activity of glycolytic enzymes Reduces the activity of the enzymes of gluconeogenesis Increased synthesis of glycogen Increased uptake of glucose by resting skeletal muscles Reduction of blood glucose level Reduction of lipolysis and stimulation of lipid synthesis Pancreas secretes 40-50 units of insulin daily in two steps: Secreted at low levels during fasting, increased level after eating, an early burst of insulin occurs within 10 minutes of eating, the proceeds with increasing release as long as hyperglycemia is present Classification by American diabetic association 2009 Type-1 diabetes Type-2 Diabetes GDM Secondary DM
- 8. Diabetes is a chronic disease that occurs either when the pancreas does not produce enough insulin or when the body cannot effectively use the insulin it produces. Insulin is a hormone that regulates blood glucose. Hyperglycaemia, also called raised blood glucose or raised blood sugar, is a common effect of uncontrolled diabetes and over time leads to serious damage to many of the body's systems, especially the nerves and blood vessels. In 2014, 8.5% of adults aged 18 years and older had diabetes. In 2019, diabetes was the direct cause of 1.5 million deaths and 48% of all deaths due to diabetes occurred before the age of 70 years. Another 460 000 kidney disease deaths were caused by diabetes, and raised blood glucose causes around 20% of cardiovascular deaths (1). Between 2000 and 2019, there was a 3% increase in age-standardized mortality rates from diabetes. In lower-middle-income countries, the mortality rate due to diabetes increased 13%. By contrast, the probability of dying from any one of the four main noncommunicable diseases (cardiovascular diseases, cancer, chronic respiratory diseases or diabetes) between the ages of 30 and 70 decreased by 22% globally between 2000 and 2019. DIABETES RISK FACTORS: Non-modifiable risk factors for Type 2 diabetes: Risk factors that increase your risk for developing prediabetes and Type 2 diabetes that can’t be changed are: Family history: Some factors that increase the risk of diabetes are inherited from our parents or close biological relatives. If you have a blood relative with diabetes, your risk for developing it is significantly increased. Share your family health history with your doctor to find out what it may mean for you. Race or ethnic background: If you’re of African-American, Asian- American, Latino/Hispanic-American, Native American or of Pacific- Islander descent, you have a greater chance of developing diabetes. Age: The older you are, the higher your risk for prediabetes and Type 2 diabetes. Type 2 diabetes generally occurs in middle-aged adults, most frequently after age 40. But health care professionals are diagnosing more and more children and adolescents with Type 2 diabetes. Gestational diabetes: If you developed diabetes during pregnancy, you are at increased risk of developing diabetes again later in life. Modifiable risk factors for Type 2 diabetes
- 9. You can — and should — do something about your modifiable risk factors. You can reduce your risk for diabetes or delay its development by making healthy changes: Weight: Being overweight or obese increases your risk of developing diabetes. Losing 5% to 10% of your body weight—in addition to getting regular physical activity—can significantly reduce your risk of developing diabetes. Your risk decreases even more as you lose more weight. For most people, a body mass index calculator will provide a good target weight for your height. Learn how to manage your weight. Physical activity: Physical inactivity is a key modifiable risk factor for prediabetes and Type 2 diabetes. Regular physical activity helps lower insulin resistance. This means your body can use its own insulin more effectively. Even a brisk 30-minute walk at least five days a week has been shown to significantly reduce the risk of diabetes and heart disease. For your overall cardiovascular health, aim for: o At least 150 minutes per week of moderate-intensity aerobic physical activity; o Or 75 minutes per week of vigorous-intensity aerobic physical activity (or a combination of the two); o And muscle-strengthening at least two days per week. Blood pressure: In addition to causing damage to the cardiovascular system, untreated high blood pressure has been linked to complications from diabetes. People with diabetes and HBP should maintain a blood pressure of less than 130/80 mm Hg. Normal blood pressure is below 120/80 mm Hg. Learn more about high blood pressure and how to control it. Cholesterol (lipid) levels: Diabetes is associated with atherosclerosis (hardening of the arteries) and blood vessel disease. Low HDL “good” cholesterol and/or high triglycerides can increase the risk for Type 2 diabetes and cardiovascular disease. Following a healthy eating plan, getting regular physical activity and reaching and maintaining a healthy weight can help improve abnormal lipid levels. Sometimes, medications are also needed. Smoking: If you smoke, there are a number of tools, medications and online resources that you can use to help you quit. Talk to your health care team about the best options for you. Diet: It’s important to eat healthy foods in the right amounts. Diet is one of the most important modifiable risk factors for prediabetes and Type 2
- 10. diabetes. The American Heart Association recommends an eating plan that includes fruits and vegetables, whole grains, skinless poultry, fish, legumes, non-tropical vegetable oils and unsalted nuts and seeds. A healthy diet should also replace saturated fats with monounsaturated and polyunsaturated fats, avoid trans fats, reduce cholesterol and sodium (salt) and limit red and processed meats, refined carbohydrates and sweetened beverages. Alcohol: Heavy use of alcohol can cause inflammation in the pancreas and limit its ability to produce enough insulin. Alcohol can cause liver damage and adds more sugar and starch to your diet that must either be used or stored as fat. Moderate your alcohol intake. That means no more than one drink per day for women or two drinks per day for men. Stress and well-being: Everyone feels stress, but people react differently. Managing the stress in our lives is an important part of healthy living, not only for diabetes but for heart disease and many other conditions. Find ways to address the causes of your stress and make time for things you enjoy. Learn how to take care of your mental health. Sleep: Adults should get seven to nine hours of sleep a night. Sleep benefits your whole body, including your heart and brain. It improves mood, memory and reasoning. Research also has shown that too little or too much sleep is linked to a high A1C in people with Type 2 diabetes. If you have insomnia (trouble going to sleep or waking up too soon) or sleep apnea (problems breathing while asleep), work with your health care team to diagnose and treat them. Learn why sleep is essential to overall health. Gestational Diabetes: Risk for gestational diabetes (diabetes while pregnant) if: Had gestational diabetes during a previous pregnancy. Have given birth to a baby who weighed over 9 pounds. Are overweight. Are more than 25 years old. Have a family history of type 2 diabetes. Have a hormone disorder called polycystic ovary syndrome (PCOS). Are an African American, Hispanic or Latino, American Indian, Alaska Native, Native Hawaiian, or Pacific Islander person. Gestational diabetes usually goes away after give birth, but increases risk for type 2 diabetes. Baby is more likely to have obesity as a child or teen, and to develop type 2 diabetes later in life. Before get pregnant, may be able to prevent gestational diabetes with lifestyle changes. These include losing weight if overweight, eating a healthy diet, and getting regular physical activity.
- 11. WHO aims to stimulate and support the adoption of effective measures for the surveillance, prevention and control of diabetes and its complications, particularly in low- and middle-income countries. To this end, WHO: Provides Scientific Guidelines For The Prevention Of Major Noncommunicable Diseases Including Diabetes; Develops Norms And Standards For Diabetes Diagnosis And Care; Builds Awareness On The Global Epidemic Of Diabetes, Marking World Diabetes Day (14 November); And Conducts Surveillance Of Diabetes And Its Risk Factors.
- 12. In April 2021 WHO launched the Global Diabetes Compact, a global initiative aiming for sustained improvements in diabetes prevention and care, with a particular focus on supporting low- and middle-income countries. In May 2021, the World Health Assembly agreed a Resolution on strengthening prevention and control of diabetes. In May 2022 the World Health Assembly endorsed five global diabetes coverage and treatment targets to be achieved by 2030. An article in Current Diabetes Reports says, "An estimated 9.1% of the overall U.S. population has diagnosed diabetes, 5.2% has undiagnosed diabetes, and an additional 38.0% has prediabetes." The World Health Organization estimates diabetes as the seventh leading cause of death worldwide. These numbers are expected to continue to rise with increases in elderly population, sedentary lifestyle and widespread obesity. DIABETES PREVENTION The best way to stop the diabetes epidemic is prevention. The Centers for Disease Control and Prevention report that one in four people who have diabetes don't know it. This is why it is important for nurses to provide patient education, not only to those diagnosed with diabetes, but those who are at high risk for developing diabetes. Nurses can help by: Educating patients about risk factors, like family history, advancing age, excess weight and a sedentary lifestyle. Partnering with patients to develop personal prevention strategies like limiting sugar and carbohydrates, increasing activity, aiming toward their ideal body weight, and setting small weight loss goals. Teaching patients about critical lab values and how to recognize and report signs and symptoms of hypoglycemia or hyperglycemia. Providing education and counseling for patients who are borderline diabetic or have metabolic syndrome as well as patients diagnosed with diabetes. The Front Lines Nurses are at the forefront of diabetes care. They are often present at diagnosis and may care for patients throughout the life of the disease. Watch patients' lab values closely, particularly the A1C, C-reactive protein and fasting blood glucose values. Provide information on topics related to diabetes to both patients and caregivers.
- 13. Diabetes Education Topics Lifestyle Disease and Management Healthy food choices · Foods to eat (nuts, oatmeal) · Foods to avoid (sugar, white flour) Symptoms · Polyuria · Polydipsia · Polyphagia Exercise tips ·How much, how often, what type ·Ways to increase activity throughout the day Types of diabetes · Type I · Type II · Gestational · Pre-diabetes · Metabolic syndrome Smoking · Impact of smoking on diabetes · Smoking cessation strategies Management · Blood glucose monitoring ·Hypoglycemia signs and management · Insulin administration Diabetes and Mood: Diabetes does not just affect blood sugar — it can lead to mental health changes, causing emotional strain and therefore impacting relationships. It can cause mood swings, confusion, anxiety, depression and stress. With end-stage disease, diabetes contributes to caregiver
- 14. burden or distress. Nurses can listen to concerns and connect them with resources. Check out the Defeat Diabetes Foundation to find local diabetes support groups. Diabetes Nurse Educator: Nurses who want to specialize in diabetes education can become a Certified Diabetes Care and Education Specialist through the National Certification Board for Diabetes Educators, or become a diabetes nurse (although that requires an MSN). These roles are vital to help patients: Identify their risk factors Identify if they have diabetes or prediabetes Work through the emotional and physical response to a diagnosis Identify resources in their community Manage their disease throughout all stages of life to minimize nerve damage and other symptoms Patients with diabetes must follow a lifelong care plan that includes a modified diet, weight management, medications and lifestyle changes. It's a complex disease, and it often falls to the nurse to educate patients about how to manage diabetes and recognize signs that their plan is not working for them. Finally, diabetes research continually advances our understanding of the disease and provides new treatment approaches. It is the responsibility of the nurse to stay abreast of these new developments and incorporate them into practice. RN to BSN programs provide the latest information on diabetes, training in evidence- based nursing care, and skills necessary to educate patients with all levels of health literacy.
- 15. SESSION -2 PATHOPHYSIOLOGY AND DIAGNOSIS OF DIABETES Diabetes is on the rise worldwide, and is a serious, lifelong disease that can lead to heart disease, stroke, and lasting nerve, eye and foot problems. Diabetes around the world in 2021 537 million adults (20-79 years) are living with diabetes - 1 in 10. This number is predicted to rise to 643 million by 2030 and 783 million by 2045. Over 3 in 4 adults with diabetes live in low- and middle-income countries. Diabetes is responsible for 6.7 million deaths in 2021 - 1 every 5 seconds. Diabetes caused at least USD 966 billion dollars in health expenditure – a 316% increase over the last 15 years. 541 million adults have Impaired Glucose Tolerance (IGT), which places them at high risk of type 2 diabetes. An organ in body called the pancreas produces insulin, a hormone that controls the levels of blood sugar. When have too little insulin in body, or when insulin doesn't work right in body, can have diabetes, the condition where have abnormally high glucose or sugar levels in blood. Normally when eat food, glucose enters bloodstream. Glucose is body's source of fuel. Pancreas makes insulin to move glucose from bloodstream into muscle, fat, and liver cells, where body turns it into energy. People with diabetes have too much blood sugar because their body cannot move glucose into fat, liver, and muscle cells to be changed into and stored for energy. There are three major types of diabetes. Type 1 diabetes happens when the body makes little or no insulin. It usually is diagnosed in children, teens, or young adults.
- 16. But about 80% of people with diabetes have what's called Type 2 diabetes. This disease often occurs in middle adulthood, but young adults, teens, and now even children are now being diagnosed with it linked to high obesity rates. In Type 2 diabetes, fat, liver, and muscle cells do not respond to insulin appropriately. Another type of diabetes is called gestational diabetes. It's when high blood sugar develops during pregnancy in a woman who had not had diabetes beforehand. Gestational diabetes usually goes away after the baby is born. But, still pay attention. These women are at a higher risk of type 2 diabetes over the next 5 years without a change in lifestyle. If doctor suspects have diabetes, will probably have a hemoglobin A1c test. This is an average of blood sugar levels over 3 months. You have pre-diabetes if your A1c is 5.7% to 6.4%. Anything at 6.5% or higher indicates you have diabetes. Type 2 diabetes is a wakeup call to focus on diet and exercise to try to control blood sugar and prevent problems. If do not control blood sugar, could develop eye problems, have problems with sores and infections in feet, have high blood pressure and cholesterol problems, and have kidney, heart, and problems with other essential organs. People with Type 1 diabetes need to take insulin every day, usually injected under the skin using a needle. Some people may be able to use a pump that delivers insulin to their body all the time. People with Type 2 diabetes may be able to manage their blood sugar through diet and exercise. But if not, they will need to take one or more drugs to lower their blood sugar levels. The good news is, people with any type of diabetes, who maintain good control over their blood sugar, cholesterol, and blood pressure, have a lower risk of kidney disease, eye disease, nervous system problems, heart attack, and stroke, and can live, a long and healthy life.
- 17. Diabetes can affect many major organs, including your heart, eyes, kidneys, and brain. When the disease isn't well-controlled, it can lead to many serious comorbidities, which are conditions that occur alongside diabetes. For people with type 1 and type 2 diabetes, finding a treatment plan that works is vital to avoid these problems Heart: The heart is part of the cardiovascular or circulatory system. This body system also includes blood vessels, which transport oxygen and nutrients to organs and tissues. Blood vessels also help remove carbon dioxide, toxins, and waste. There are four main parts of the circulatory system. Each part has a specific job: Capillaries: These are your body's smallest blood vessels. They carry oxygen and nutrients to distant parts of the body and deliver waste products to the kidneys and liver. They also transport carbon dioxide to the lungs so it can be exhaled. Veins: Your veins carry blood that has had the oxygen removed back to the heart. Arteries: Arteries transport oxygen-rich blood from the heart throughout the circulatory system. Heart: The heart is the muscle that pumps blood throughout the entire body. The American Heart Association lists diabetes as one of the seven major controllable risk factors for cardiovascular disease (CVD). CVDs include all types of heart disease, stroke, and blood vessel disease. The most common type of CVD is coronary artery disease (CAD). It is caused by the build-up of plaque (cholesterol) in the walls of the arteries. Diabetes can put you at higher risk for CAD because it can cause problems with your platelets, the cells that help your blood clot. When you have diabetes, you may also form plaques that are more prone to breaking off and blocking blood flow. People with diabetes are twice as likely to develop cardiovascular disease than people without diabetes. Over time, diabetes can also cause damage to the blood vessels and nerves that control the heart. The longer you have diabetes, the higher the chances you will develop heart disease. People with diabetes often have other conditions that increase the risk of heart disease, including: High blood pressure, High cholesterol, High triglycerides
- 18. Kidneys: The kidneys are bean-shaped organs located below the rib cage and beside the spine. Each is roughly the size of a fist. They are part of the renal system, which also includes: Ureters are the tubes that take urine from your kidneys to bladder The bladder stores urine until it can be expelled The urethra removes urine from the body The kidneys work as a filtration system. They remove waste, extra fluid, and acid from the body. Healthy kidneys help keep a good balance of water, salts, and minerals in the blood. The kidneys also produce vitamin D and erythropoietin. Vitamin D helps your body absorb calcium and promotes a healthy immune system. Erythropoietin is a hormone that stimulates the production of red blood cells. Over time, high blood sugar caused by diabetes can damage blood vessels in your kidneys. This can impair their ability to clean the body, leading to a build-up of waste and fluid in the blood. This type of kidney disease is known as diabetic nephropathy. If left untreated, diabetic nephropathy can cause kidney failure, which can be life- threatening. About 18% of adult diagnosed with diabetes have chronic kidney disease in its advanced stages, according to the Centers for Disease Control and Prevention. Brain: High blood sugar can affect cognition, specifically thinking and memory. Research has also shown that diabetes can change the structure of your brain. Because of this, people with diabetes are at increased risk of cognitive decline and are 50% more likely to develop dementia than those without diabetes. Studies have shown that people with diabetes have lower levels of gray matter density and volume in various parts of the brain. Gray matter is a major part of the central nervous system. It plays a role in daily functioning. Reduced gray matter density or volume can affect a variety of brain and nerve functions. Diabetes can also damage small blood vessels in the brain. This can lead to strokes or the death of brain tissue. Lungs: Uncontrolled diabetes may reduce lung function. This can lead to mild complications like asthma or more severe complications like pulmonary fibrosis.
- 19. Researchers don't know why people with diabetes can have lung problems. Some think inflammation may be the root cause. Some studies suggest that drugs that treat low blood sugar may contribute to lung disease in people with diabetes. One found that different medications may affect the lungs in different ways. For example, the common diabetes drug Glucophage (metformin) is thought to work against lung disease, while insulin may make lung disease worse. Pancreas: Diabetes and the pancreas are closely linked. This is because pancreas produces insulin. High blood sugar can happen when pancreas doesn’t produce enough or any insulin. Type 1 diabetes is caused by this lack of insulin production. Type 2 diabetes, on the other hand, happens when your body builds up insulin resistance. This puts strain on the pancreas as it tries to produce more insulin than it normally needs to. Pancreatic cancer can be a consequence of diabetes, but it can also be the cause. People with type 2 diabetes are at increased risk of developing pancreatic cancer, and pancreatic cancer can also lead to the development of diabetes. Mouth and Teeth: Glucose is present in saliva. When diabetes is not controlled, high glucose levels in saliva help harmful bacteria grow. These can combine with food to form a soft, sticky film called plaque. Some types of plaque cause tooth decay or cavities. Others cause gum disease and bad breath. When have diabetes, gum disease can be more severe and take longer to heal. Having gum disease can also make blood glucose hard to control. Plaque can harden over time into tartar, making it more difficult to brush and clean between teeth. When this happens, the gums may become red and swollen, and bleed easily. These are signs of a gum disease called gingivitis. Untreated gingivitis can advance to a gum disease called periodontitis. When have this condition, the gums pull away from the teeth and form pockets. These pockets become infected, and the infection can last a long time. Untreated periodontitis can destroy the gums, bones, and tissue that support the teeth. Your teeth may become loose and might need to be removed. Stomach and Small Intestines: High blood sugar levels can damage the vagus nerve. This is the nerve that runs from the brainstem down to the abdomen. When the vagus nerve is damaged, it can cause a condition known as gastroparesis.
- 20. When you have this condition, your stomach empties food much slower than it's supposed to. This can lead to complications like: Dehydration Stomach acid that leaks into the food pipe, a condition known as gastroesophageal reflux disease (GERD) Malnutrition from the body not digesting food properly Unpredictable changes in blood sugar levels Roughly 20% to 50% of people with diabetes will experience gastroparesis. Eyes: Sometimes, eye symptoms like blurry vision are the first symptoms of diabetes. Over time, diabetes can lead to diabetic retinopathy. This condition can cause vision problems and blindness. High blood sugar can damage the retina and surrounding blood vessels. The retina is a layer of tissue in the back of the eye that is sensitive to light. When this happens, your body tries to compensate by producing new, abnormal blood vessels that are much weaker and prone to bleeding. Diabetic retinopathy can cause other eye problems, such as: Diabetic macular edema: The new, weaker blood vessels leak fluid and blood into the retina. This causes swelling of the macula, the center of the retina. Neovascular glaucoma: This secondary type of glaucoma occurs when new blood vessels close over the part of the eye where the cornea meets the iris. The cornea is the clear tissue at the front of your eye. The iris is the colored part of your eye. If have diabetes and are experiencing vision problems, seek medical care right away. These vision problems may be irreversible, and treatment can stop them from progressing to total blindness. Skin: High blood sugar can cause poor circulation. This can damage skin and make it hard for your body to repair wounds. Anyone can get a skin condition, but certain conditions only happen to people with diabetes. These include: Diabetic dermopathy: This causes small, round, brown lesions on the shins. Roughly 55% of people with diabetes will develop this condition. Necrobiosis lipoidica diabeticorum: In the early stages, this condition causes red bumps to form on the lower legs. In later stages, the lesions
- 21. become flat-topped and shiny and may be yellow or brown. Less than 1% of people with diabetes will develop this condition. Diabetic blisters: Diabetic blisters look like blisters that form after a burn, but they are not painful. They tend to develop in clusters. Eruptive xanthomatosis: This skin condition appears as small yellow and red bumps. Foot ulcers are also common in people with diabetes. They are typically found on the big toes and balls of the feet and can be mild or severe. Their severity is usually measured on a scale of 0 to 5. A possible healed lesion is a 0, while 5 is a severe case of gangrene (tissue death). Sexual Organs: Circulatory system damage causes a decrease in blood flow. This, along with damage to nerves and their ability to send signals, can impair blood flow to the penis. This can cause erectile dysfunction in males with diabetes. Sperm health also relies on body's ability to process glucose. When have diabetes, this ability is compromised, which can lead to poor sperm health. Mature sperm may not be able to fertilize an egg, and they may also be less mobile. Both males and females with diabetes can experience fertility issues. In males, diabetes can lead to low testosterone levels. This can affect sperm count and lead to a decrease in sex drive. Among females, diabetes can also cause nerve damage that can lead to vaginal dryness. Blood vessel damage can also result in a lack of blood flow to female reproductive organs. In females without diabetes, insulin helps drive the production of the hormones that maintain reproductive tissues and regulate ovulation. When you have diabetes, this process doesn't work as well. Diabetes has also been linked to polycystic ovary syndrome (PCOS). This condition is caused by high testosterone levels. It can impair ovulation or the release of an egg. This makes it difficult to get pregnant
- 24. Regulation of Blood glucose and insulin
- 26. Type 1 diabetes Type 1 diabetes (previously known as insulin-dependent, juvenile or childhood- onset) is characterized by deficient insulin production and requires daily administration of insulin. In 2017 there were 9 million people with type 1 diabetes; the majority of them live in high-income countries. Neither its cause nor the means to prevent it are known.
- 27. Type 2 diabetes Type 2 diabetes affects how body uses sugar (glucose) for energy. It stops the body from using insulin properly, which can lead to high levels of blood sugar if not treated. Over time, type 2 diabetes can cause serious damage to the body, especially nerves and blood vessels. Type 2 diabetes is often preventable. Factors that contribute to developing type 2 diabetes include being overweight, not getting enough exercise, and genetics. Early diagnosis is important to prevent the worst effects of type 2 diabetes. The best way to detect diabetes early is to get regular check-ups and blood tests with a healthcare provider. Symptoms of type 2 diabetes can be mild. They may take several years to be noticed. Symptoms may be similar to those of type 1 diabetes but are often less marked. As a result, the disease may be diagnosed several years after onset, after complications have already arisen. More than 95% of people with diabetes have type 2 diabetes. Type 2 diabetes was formerly called non-insulin dependent, or adult onset. Until recently, this type of diabetes was seen only in adults but it is now also occurring increasingly frequently in children. Gestational diabetes Gestational diabetes is hyperglycaemia with blood glucose values above normal but below those diagnostic of diabetes. Gestational diabetes occurs during pregnancy. Women with gestational diabetes are at an increased risk of complications during pregnancy and at delivery. These women and possibly their children are also at increased risk of type 2 diabetes in the future. Gestational diabetes is diagnosed through prenatal screening, rather than through reported symptoms.
- 29. SCREENING FOR DIABETES MELLITUS
- 30. Anyone who has symptoms of diabetes or is at risk for the condition should be tested. People are routinely tested for gestational diabetes during their second trimester or third trimester of pregnancy. Blood tests to diagnose prediabetes and diabetes: The fasting plasma glucose (FPG) test measures your blood sugar after you’ve fasted for 8 hours. The A1C test provides a snapshot of your blood sugar levels over the previous 3 months. A 75-gram oral glucose tolerance test is also used. This checks the BG 2 hours after ingesting a sugary drink containing 75 grams of carbs. To diagnose gestational diabetes, your doctor will test blood sugar levels between the 24th week and 28th week of pregnancy. There are two types of tests: Glucose challenge test: During a glucose challenge test, blood sugar is checked an hour after drink a sugary liquid. If your results are standard, no more testing is done. If blood sugar levels are high, need to undergo a glucose tolerance test.
- 31. Glucose tolerance test: During a glucose tolerance test, blood sugar is checked after fast overnight. Then you’re given a sugary drink and blood sugar is re-tested after 1 hour and again after 2 hours. Gestational diabetes is diagnosed if any of these three readings come back noting high blood sugar.
- 34. SESSION -3 DIABETES TREATMENT OPTIONS Diabetes is a chronic, metabolic disease characterized by elevated levels of blood glucose (or blood sugar), which leads over time to serious damage to the heart, blood vessels, eyes, kidneys and nerves. The most common is type 2 diabetes, usually in adults, which occurs when the body becomes resistant to insulin or doesn't make enough insulin. In the past 3 decades the prevalence of type 2 diabetes has risen dramatically in countries of all income levels. Type 1 diabetes, once known as juvenile diabetes or insulin-dependent diabetes, is a chronic condition in which the pancreas produces little or no insulin by itself. For people living with diabetes, access to affordable treatment, including insulin, is critical to their survival. There is a globally agreed target to halt the rise in diabetes and obesity by 2025. About 422 million people worldwide have diabetes, the majority living in low- and middle-income countries, and 1.5 million deaths are directly attributed to diabetes each year. Both the number of cases and the prevalence of diabetes have been steadily increasing over the past few decades.
- 35. Life style modification 1. Eat healthy. This is crucial when have diabetes, because what eat affects blood sugar. No foods are strictly off-limits. Focus on eating only as much as body needs. Get plenty of vegetables, fruits, and whole grains. Choose non fat dairy and lean meats. Limit foods that are high in sugar and fat. Remember that carbohydrates turn into sugar, so watch your carb intake. Try to keep it about the same from meal to meal. This is even more important if you take insulin or drugs to control your blood sugars. 2. Exercise. If not active now, it’s time to start. Don't have to join a gym and do cross-training. Just walk, ride a bike, or play active video games. Goal should be 30 minutes of activity that makes sweat and breathe a little harder most days of the week. An active lifestyle helps you control diabetes by bringing down blood sugar. It also lowers chances of getting heart disease. Plus, it can help lose extra pounds and ease stress. 3. Get check ups. See your doctor at least twice a year. Diabetes raises your odds of heart disease. So learn numbers: cholesterol, blood pressure, and A1c (average blood sugar over 3 months). Get a full eye exam every year. Visit a foot doctor to check for problems like foot ulcers and nerve damage. 4. Manage stress. When stressed, blood sugar levels go up. And when anxious, you may not manage diabetes well. You may forget to exercise, eat right, or take medicines. Find ways to relieve stress -- through deep breathing, yoga, or hobbies that relax you. 5. Stop smoking. Diabetes makes more likely to have health problems like heart disease, eye disease, stroke, kidney disease, blood vessel disease, nerve damage, and foot problems. If you smoke, chance of getting these problems is even higher. Smoking also can make it harder to exercise. Talk with doctor about ways to quit. 6. Watch alcohol. It may be easier to control blood sugar if you don’t get too much beer, wine, and liquor. So if choose to drink, don't overdo it. The American Diabetes Association says that women who drink alcohol should have no more than one drink a day and men should have no more than two. Alcohol can make your blood sugar go too high or too low. Check your blood sugar before you drink, and take steps to avoid low blood sugars. If you use insulin or take drugs for your diabetes, eat when you're drinking. Some drinks -- like wine coolers -- may be higher in carbs, so take this into account when you count carbs. Prevention: Lifestyle changes are the best way to prevent or delay the onset of type 2 diabetes. To help prevent type 2 diabetes and its complications, people should: Reach And Keep A Health Body Weight
- 36. Stay Physically Active With At Least 30 Minutes Of Moderate Exercise Each Day Eat A Healthy Diet And Aoid Sugar And Saturated Fat Not Smoke Tobacco Diabetes and diet Healthy eating is a central part of managing diabetes. In some cases, changing your diet may be enough to manage the disease. Types 1 diabetes Blood sugar level rises or falls based on the types of foods you eat. Starchy or sugary foods make blood sugar levels rise rapidly. Protein and fat cause more gradual increases. Medical team may recommend that limit the amount of carbohydrates eat each day. You’ll also need to balance carb intake with insulin doses. Counting carbs helps to balance the carb intake with the insulin doses. Type 2 diabetes Eating the right types of foods can both manage blood sugar and help lose any excess weight. Carb counting is an important part of eating for type 2 diabetes. A dietitian can help you figure out how many grams of carbohydrates to eat at each meal. In order to keep blood sugar levels steady, try to eat small meals throughout the day. Emphasize healthy foods such as: fruits vegetables whole grains lean protein such as poultry and fish healthy fats such as olive oil and nuts Certain other foods can hurt efforts to manage blood sugar. Gestational diabetes: Eating a well-balanced diet is important for both and baby during these 9 months. Making the right food choices can also help avoid diabetes medications. Watch portion sizes, and limit sugary or salty foods. Although need some sugar to feed growing baby, should avoid eating too much. Check out other do’s and don’ts for healthy eating with gestational diabetes.
- 37. The bottom line: Work with a registered dietitian if you have access to one. They can help design an individualized diabetes meal plan. Getting the right balance of protein, fat, and carbs can help you manage your blood sugar. Diabetes and exercise: Along with diet and treatment, exercise plays an essential role in diabetes management. This is true for all types of diabetes. Staying active helps cells react to insulin more effectively and lower blood sugar levels. Exercising regularly can also help: Reach And Maintain A Healthy Weight Reduce Your Risk Of Diabetes-Related Health Complications Boost Mood Get Better Sleep Improve Memory If have type 1 or type 2 diabetes, general guidance is to aim for at least 150 minutes of moderate-intensity exercise each week. There are currently no separate exercise guidelines for people who have gestational diabetes. But if pregnant, start out slowly and gradually increase activity level over time to avoid overdoing it. Diabetes-friendly exercises include: Walking, swimming, dancing, cycling Talk with doctor about safe ways to incorporate activity into diabetes management plan. You may need to follow special precautions, like checking blood sugar before and after working out and making sure to stay hydrated. Consider working with a personal trainer or exercise physiologist who has experience working with people who have diabetes. They can help to develop a personalized workout plan tailored to your needs. Diabetes prevention Type 1 and type 1.5 diabetes are not preventable because they are caused by an issue with the immune system. Some causes of type 2 diabetes, such as your genes or age, aren’t under your control either. Yet many other diabetes risk factors are manageable. Most diabetes prevention strategies involve making simple adjustments to your diet and fitness routine.
- 38. If you’ve received a diagnosis of prediabetes, here are a few things you can do to delay or prevent type 2 diabetes: Get at least 150 minutes per week of aerobic exercises like walking or cycling. Cut saturated and trans fats, along with refined carbohydrates, out of your diet. Eat more fruits, vegetables, and whole grains. Eat smaller portions. Try to lose 5% to 7%Trusted Source of your body weight if you have overweight or obesity. These aren’t the only ways to prevent diabetes. Discover more strategies that may help you avoid this chronic health condition. Diabetes in pregnancy: People who’ve never had diabetes can suddenly develop gestational diabetes during pregnancy. Hormones produced by the placenta can make your body more resistant to the effects of insulin. Pre-gestational diabetes: People can have diabetes before they conceive and carry it with them into pregnancy. This is called pre-gestational diabetes.
- 39. Risks to newborn: Diabetes during pregnancy can lead to complications for your newborn, such as jaundice or breathing problems. If diagnosed with pre- gestational or gestational diabetes, need special monitoring to prevent complications. Gestational diabetes should go away after you deliver, but it does significantly increase your risk of getting diabetes later. About half Trusted Source of people with gestational diabetes will go on to develop type 2 diabetes. Diabetes in children; Children can get both type 1 and type 2 diabetes. Managing blood sugar is especially important in young people because diabetes can damage important organs such as the heart and kidneys. Type 1 diabetes; The autoimmune form of diabetes often starts in childhood. One of the main symptoms is increased urination. Kids with type 1 diabetes may start wetting the bed after they’ve been toilet trained. Extreme thirst, fatigue, and hunger are also signs of the condition. It’s important that children with type 1 diabetes get treatment right away. The condition can cause high blood sugar, dehydration, and diabetic ketoacidosis (DKA), which can be medical emergencies. Type 2 diabetes: Type 1 diabetes used to be called juvenile diabetes because type 2 was so rare in children. Now that more children have overweight or obesity, type 2 diabetes is becoming more common in this age group. Some children living with type 2 diabetes don’t experience symptoms. Others may experience: Increased thirst Frequent urination Extreme fatigue Blurry vision Type 2 diabetes is often diagnosed based on medical history, a physical exam, and blood work. Untreated type 2 diabetes can cause lifelong complications, including heart disease, kidney disease, and blindness. Healthy eating and exercise can help your child manage their blood sugar and prevent these problems. Type 2 diabetes is more prevalent than ever in young people.
- 40. DIAGNOSIS AND TREATMENT Early diagnosis can be accomplished through relatively inexpensive testing of blood glucose. People with type 1 diabetes need insulin injections for survival. One of the most important ways to treat diabetes is to keep a healthy lifestyle. Some people with type 2 diabetes will need to take medicines to help manage their blood sugar levels. These can include insulin injections or other medicines. Some examples include: Metformin Sulfonylureas Sodium-glucose co-transporters type 2 (sglt-2) inhibitors. Along with medicines to lower blood sugar, people with diabetes often need medications to lower their blood pressure and statins to reduce the risk of complications. Additional medical care may be needed to treat the effects of diabetes: Foot care to treat ulcers Screening and treatment for kidney disease Eye exams to screen for retinopathy (which causes blindness).
- 44. INSULIN THERAPY Insulin is a hormone produced by the pancreas to help the body use and store glucose (sugar). Glucose is a source of fuel for the body. In people with diabetes, the body cannot regulate the amount of glucose in the blood (called glycemia or blood sugar). Insulin therapy can help some people with diabetes maintain their blood sugar levels. Carbohydrates from food are broken down into glucose and other sugars. Glucose is absorbed from the digestive tract into the bloodstream. Insulin lowers blood sugar by allowing it to move from the bloodstream into muscle, fat, and other cells, where it can be stored or used as fuel. Insulin also tells the liver how much glucose to produce when you are fasting (have not had a recent meal). People with diabetes have high blood sugar because their body does not make enough insulin or because their body does not respond to insulin properly. In people with type 1 diabetes the pancreas produces little to no insulin. In people with type 2 diabetes the fat, liver, and muscle cells do not respond correctly to insulin. This is called insulin resistance. Over time, the pancreas stops making as much insulin. Insulin Doses and Types: Insulin therapy replaces the insulin the body would normally make. People with type 1 diabetes must take insulin every day. People with type 2 diabetes need to take insulin when other treatments and medicines fail to control blood sugar levels. Insulin doses are given in two main ways: Basal dose - provides a steady amount of insulin delivered all day and night. This helps maintain blood glucose levels by controlling how much glucose the liver releases (mainly at night when the time between meals is longer). Bolus dose - provides a dose of insulin at meals to help move absorbed sugar from the blood into muscle and fat. Bolus doses can also help correct blood sugar when it gets too high. Bolus doses are also called nutritional or meal-time doses. Sometimes, a bolus dose must also be taken with large snacks. There are several types of insulin available. Insulin types are based on the following factors: Onset - how quickly it starts working after injection Peak - time when the dose is the strongest and most effective Duration - total time the insulin dose stays in the bloodstream and lowers blood sugar Below are the different types of insulin:
- 45. Rapid-acting or fast-acting insulin starts working within 15 minutes, peaks in 1 hour, and lasts for 2 to 4 hours. It is taken right before or just after meals and snacks. It is often used with longer-acting insulin. Regular or short-acting insulin reaches the bloodstream 30 minutes after use, peaks within 2 to 3 hours, and lasts 3 to 6 hours. This is taken a half-hour before meals and snacks. It is often used with longer-acting insulin. Intermediate-acting insulin starts working within 2 to 4 hours, peaks in 4 to 12 hours, and lasts 12 to 18 hours. This is taken mostly either twice a day or once at bedtime. Long-acting insulin starts to work a few hours after injection and works for about 24 hours, sometimes longer. It helps control glucose throughout the day. It is often combined with rapid- or short-acting insulin as needed. Premixed or mixed insulin is a combination of 2 different types of insulin. It has both a basal and bolus dose to control glucose after meals and throughout the day. Inhaled insulin is a rapid-acting breathable insulin powder that starts working within 15 minutes of use. It peaks 30 minutes after taking it and lasts about 3 hours. It is used just before meals. One or more types of insulin may be used together to help control blood sugar. Dosing schedule may depend on: Body weight Type of insulin take How much and what eat Level of physical activity Blood sugar level Other health conditions Insulin cannot be taken by mouth because stomach acid destroys insulin. It is most often injected under the skin into fatty tissue. There are different insulin delivery methods available: Insulin syringe -- insulin is drawn from a vial into a syringe. Using the needle, you inject the insulin under the skin. Insulin pen -- disposable insulin pens have prefilled insulin delivered under the skin using a replaceable needle. Insulin pump -- a small machine worn on the body pumps insulin under the skin throughout the day. A small tube connects the pump to a small needle inserted into the skin. Inhaler -- a small device you use to inhale insulin powder through your mouth. It is used at the start of meals. Injection port -- a short tube is inserted into the tissue under the skin. The port containing tube is adhered to skin using adhesive tape. Fast-acting insulin is injected into the tube using a syringe or pen. This allows you to use the same injection site for 3 days before rotating to a new site.
- 46. Insulin is injected into these sites on the body: Abdomen Upper arm Thighs Hips Provider will teach how to give an insulin injection or use an insulin pump or other device. It is important not to always use the same site as this can decrease how effective the insulin is for you. Points to Remember: You need to know how to adjust the amount of insulin you are taking: When you exercise When you are sick When you will be eating more or less food When you are traveling Before and after surgery When to Call the Doctor: If you are taking insulin, contact your provider if: You think you may need to change your insulin routine You have any problems taking insulin Your blood sugar is too high or too low and you don't understand why LATEST INVENTIONS IN DIABETES MANAGEMENT In addition to the aforementioned innovations in the management of diabetes, several drugs are still at different stages of clinical trial for eventual use. Others are ready and have been recently introduced into the market. Drugs Recently Introduced Tirzepatide: The drug was recently approved by the FDA under the trade name mounjaro for the treatment of T2DM. Tirzepatide is an injectable given under the skin once in a week which targets the receptors of hormones which play central role in the metabolism of glucose. These hormones are glucagon-like peptide-1 (GLP-1) and glucose-dependent insulinotropic polypeptide (GIP). While the GLP-1 reduces blood glucose by several mechanisms, including stimulating insulin secretion and suppressing glucagon release during hyperglycemia, GIP stimulates insulin release during hyperglycemia, but it also stimulates glucagon release during hypoglycemia.
- 47. Tirzepatide acts as agonist to their receptors, hence elongating their functions which results in blood glucose control. The efficacy of tirzepatide was established against a placebo, a GLP-1 receptor agonist (semaglutide) and two long-acting insulin analogs either as monotherapy or in combination with other antidiabetic agents. In comparison to the placebo, it lowered the HbA1c by 11.6% and 1.5% as monotherapy and combination therapy, respectively. In comparison to other antidiabetic drugs, at the highest dose of 15 mg, it lowered the HbA1c 0.5% more than semaglutide, 0.9% more than insulin degludec and 1.0% more than insulin glargine. Because of the efficacy therein and the once in a week dosing, tirzepatide provides a desirable paradigm shift in the management of T2DM. Drugs in the Pipeline Several drug candidates are at different phases of development for the management of DM. These are listed below. LY3502970: LY3502970 is a partial agonist, biased toward G-protein activation over β-arrestin recruitment at the (GLP-1 receptor (GLP-1R). The molecule is highly potent and selective against other class B G- protein-coupled receptors (GPCRs) with a pharmacokinetic profile favorable for oral administration. It is a product that is currently being developed by Eli lilly. SCO-094: SCO-094 is a drug candidate identified by SCOHIA company which has a dual target of the receptors of GIP and GLP-1 Ladarixin (LDX): Ladarixin is an inhibitor of the interleukin-8 receptors CXCR1 and CXCR2, in new-onset T1DM. It is a drug candidate developed by Dompe Farmaceutici. Short term LDX treatment of newly diagnosed patients with T1DM had no appreciable effect on preserving residual beta cell function. In the current scenario, digital health management plays a significant role in T1D care and self-management. Recent technological advances including continuous glucose monitoring (CGM) and insulin pumps, have sought to ease the burden of diabetes self-management. However, insulin pumps provide automated insulin delivery but cost barriers, variable insurance coverage, and authorization hurdles prevent the wide usage of insulin pumps. Nowadays, smart insulin pens and artificial pancreas are gaining attention for T1D self-management.
- 48. Smart insulin: The introduction of "smart" insulin is promising to revolutionize diabetes treatment by allowing for more efficient and personalized glucose control. Smart insulin is a new class of insulin analogs that are intended to mimic the body's natural insulin secretion in response to glucose levels. These novel formulations are designed to self-regulate insulin release based on an individual's blood glucose level. Smart insulin combines a set of core components: digital dose capture, real-time wireless connectivity, real-time connectivity with glucose-sensing devices, and integration with insulin-dosing decision support. Remarkably, the US Food and Drug Administration (FDA) approved the usage of the first smart insulin pen in 2017. The glucose-responsive insulin (GRI) is one of the most promising smart insulin candidates. GRI formulations contain glucose-sensing elements that cause insulin release in response to hyperglycaemia. This closed-loop system provides several benefits, including better glycaemic control, a lower risk of hypoglycaemia, and increased patient convenience. Furthermore, smart insulin therapies seek to eradicate the need for multiple daily injections by developing long-acting formulations that can adjust insulin release based on glucose levels over time. These developments may reduce the burden of frequent injections, improving patient adherence and quality of life. ARTIFICIAL PANCREAS: An artificial pancreas, also termed as closed- loop insulin system, is a medical device that integrates a continuous glucose monitor, an insulin pump, and a control algorithm to regulate insulin delivery based on real-time glucose measurements. Recently, in the United States, a single closed-loop. system (MiniMed 670 G, Medtronic) was approved for 6–13 years aged T1D patients Remarkably, Food and Drug Administration (FDA), USA approved another system (t: slim X2 insulin pump with Control-IQ Technology, Tandem Diabetes Care) for the treatment of T1D patients (up to 14 years or older) However, the efficacy of artificial pancreas systems in managing T1D and minimizing the risk of hypoglycaemia is a matter of concern and thus, being investigated extensively. In 2005, a pioneer and pilot study conducted by Steil and colleagues reported improved glycaemic control and reduced occurrence of hypoglycaemia in children with T1D after using an artificial pancreas system . Furthermore, a randomized clinical trial of 16 weeks revealed that the use of an artificial pancreas system helps to improve glycaemic control in T1D children. In a long-term clinical trial, the use of an artificial pancreas system improved glycaemic control and reduced the risk of hypoglycaemia in adults with T1D over six months. Apparently, these findings suggest that an artificial pancreas system may offer significant benefits for individuals with T1D and warrant further investigation.
- 49. Complications related to T1D: In T1D, the pancreas’s insulin-producing β-cells are unintentionally attacked and destroyed by the body’s immune system and thus leading to the shortage of insulin, which controls blood sugar levels and cause a variety of complications The complications of T1D can affect various organs and systems in the body as shown in Fig Fig. 4. Potential complications of T1D. T1D is an autoimmune disease that affects pancreatic β-cells, eyes, skeletal muscle, kidney, gastrointestinal tract, circulatory system, and liver, and makes them non-functional. IMMUNOTHERAPY: Immunotherapy refers to the administration of drugs or other interventions to regulate the immune system, thereby averting the destruction of insulin-producing β-cells in the pancreas. Such interventions may involve immune modulators or biologics that selectively target specific immune cells or pathways. As a potential treatment option for T1D, immunotherapy seeks to manipulate the immune system to forestall or reverse the destruction of β-cells. In a pioneer study, Herald and colleagues studied the effect of anti-CD-3 antibody which target and deactivate the T cells that attack β-cells, on the progression of T1D, and results showed that anti-CD-3 antibody preserved the β-cell functionality in newly diagnosed T1D patients. In a randomized, double-blind, placebo-controlled clinical trial, newly-diagnosed T1D patients were inoculated with autologous T cells that were genetically engineered to express a proinsulin peptide. The T-cell vaccine was found to preserve β-cell function and reduce the deterioration in insulin secretion over a two-year period. Furthermore, low-dose interleukin-2 (IL-2) therapy has been shown to increase the number of regulatory T cells (Tregs), which can suppress the autoimmune response that results in β-cell destruction and thus, enhance the β-cell functionality in patients with new-onset T1D. In addition, transplantation of engineered islet cells capable of evading immune attack has been suggested as potential cell based-immunotherapy for T1D. Notably, modification of the islet/β-cell surface by immobilizing the anticoagulant enzymes including urokinase (UK) and thrombomodulin (TM) or biotinylating the islet membrane to conjugate streptavidin-Fas-ligand (SA-
- 50. FasL) proteins have been reported to escape the immune attack post- transplantation in T1D hosts In continuation, surface labelling of islet cells with immunomodulatory proteins including A20 and programmed death-ligand 1 (PD- L1)/cytotoxic T-lymphocyte-associated protein 4 (CTLA4) provide protection from post-transplantation immunological attack in T1D host. Overexpression of A20 protected the islets from TNFα, interleukin 1 β (IL-1β), and IFNγ-induced apoptosis. In addition, Wang and colleagues reported that PD-L1/CTLA4-Ig– expressing engineered MSCs immunologically protect the co-transplanted islets and thus could be used as accessory cells in islet transplantation to improve the graft function and to minimize the systemic immunosuppression . Reported studies clearly indicate that local immunomodulation also plays a crucial role in the immunotherapy of T1D. CELL-BASED THERAPY: Cell therapy for diabetes involves the transplantation of pancreatic islet cells or β-cells. Islet transplantation entails the transplant of islet cells from a healthy donor’s pancreas into a patient suffering from T1D. This method has been shown to enhance glucose control and lower the risk of severe hypoglycaemia in individuals with T1D. However, islet cell transplantation is associated with disadvantages like the requirement of a large number of cells for transplantation and the lack of donors. Notably, combinational cell therapy has been suggested as a potential tool for diabetes therapeutics. Various combinational diabetes therapies including gene therapy, cell encapsulation etc. are gaining attention of the researchers worldwide and are being explored for diabetes therapeutics. GENE THERAPY: Gene therapy refers to the insertion of genes into cells to correct genetic abnormalities or enhance cellular function. For individuals with T1D, gene therapy utilizes viral vectors to deliver genes that boost the growth and survival of β-cells or to silence genes that contribute to β-cell destruction. A preclinical investigation showed that the introduction of the pancreatic transcription factor Pdx-1 gene into pancreatic cells of diabetic mice reinstated glucose homeostasis and insulin production. Gene therapy utilizing glucokinase has been suggested as a potential treatment for T1D, as glucokinase is a crucial enzyme in glucose metabolism. Thus, a preclinical study demonstrated that gene therapy with glucokinase improved glucose homeostasis and prevented the development of diabetes in diabetic mice. Inflammation is known to play a key role in the pathogenesis of T1D. Gene therapy with anti-inflammatory cytokines like interleukin-10 (IL-10) has been proposed as a treatment for T1D. In a preclinical study, gene therapy with IL-10 prevented the onset of diabetes in diabetic mice. Furthermore, regulatory T cells (Tregs) are important in suppressing the autoimmune response that results in the destruction of β-cells in T1D. In a preclinical study, gene therapy with Tregs prevented the onset of diabetes and improved glucose homeostasis in diabetic
- 51. mice. Gene therapy with insulin-producing cells has also been proposed as a potential treatment for T1D. In a preclinical study, gene therapy utilizing insulin- producing cells obtained from human embryonic stem cells prevented the onset of diabetes in diabetic mice and improved glucose homeostasis. CELL ENCAPSULATION: Cell encapsulation has emerged as a promising approach for the transplantation of insulin-producing cells, such as inlet cells, without immunosuppressive drugs in patients with T1D. This technique involves using semi-permeable membranes to protect transplanted cells from the immune system while allowing nutrients and oxygen to pass through. In a clinical trial study, the implantation of alginate-encapsulated islet cells improved glycaemic control in patients without causing any major adverse events. In another attempt, the implantation of polyethylene glycol (PEG)-encapsulated islet cells improved glycaemic control and prevented immune system attack in mice. Similarly, another study revealed that the implantation of PEG-encapsulated islet cells improved glycaemic control and prevented immune system attacks in non-human primates with T1D. In a pilot clinical trial, the implantation of stem cell-derived insulin-secreting cells encapsulated in a hydrogel improved glycaemic control in patients with T1D without causing any major adverse events, while the same stem cells were utilized in a preclinical study to improve the glycaemic control and prevent immune system attack in T1D mice. STEM CELL THERAPY: Stem cell therapy is presently an area of intense exploration in the context of T1D cell-based therapeutics. The objective is to revitalize β-cells within the pancreas using stem cells that possess the ability to differentiate into a diverse range of cell types. Researchers are investigating various types of stem cells, such as induced pluripotent stem cells, adult stem cells, and embryonic stem cells, for this purpose. Although early-stage clinical trials have yielded encouraging results, further investigations are necessary to ascertain the safety and effectiveness of stem cell therapy. Stem cells: Stem cells are undifferentiated cells that possess the unique ability to differentiate into specialized cell types and self-renew. There are several types of stem cells, including embryonic stem cells (ESCs), induced pluripotent stem cells (iPSCs), and adult stem cells. Stem cells hold significant potential for medical applications, particularly in regenerative medicine and cell-based therapies for different diseases. ESCs are derived from the inner cell mass of early-stage embryos known as blastocysts. They can differentiate into any type of body cell, making them useful for studying disease modelling. However, the use of ESCs is controversial due to ethical concerns surrounding the use of embryos. Meanwhile, induced pluripotent stem cells (iPSCs) are adult cells that have been reprogrammed to a pluripotent state like ESCs. Typically, this reprogramming process is accomplished by introducing particular genes into the cells via viral
- 52. vectors or other methods. They are an important tool for modelling diseases and discovering new drugs due to their capacity to differentiate into any type of cell. On the other hand, adult stem cells are capable of differentiating into specific cell types within the tissue where they are found in the body. For example, hematopoietic stem cells in bone marrow can transform into various blood cell types. They have been utilized in numerous cell-based therapies, such as bone marrow transplants for leukaemia and other blood disorders. Further, totipotent stem cells have the ability to differentiate into any type of cell, including both embryonic & extra-embryonic tissues. In humans, totipotent stem cells are present only in the zygote (fertilized egg) and the earliest stages of embryonic development. Unipotent stem cells, in contrast, can transform into only one cell type but have the ability to self-renew. Muscle satellite cells, which can develop into muscle cells, and spermatogonial stem cells, which can differentiate into sperm cells, are some examples of unipotent stem cells. GENERATION OF INSULIN-PRODUCING CELLS (IPCS) FROM IPSCS iPSCs are used to differentiate into IPCs by employing the differentiation protocols that mimic the natural development of pancreatic β-cells. Based on the in vivo pancreas development, various multistep differentiation protocols of iPSCs-derived insulin-producing β-cells involving the differentiation of iPSCs towards endoderm cells, followed by pancreatic progenitor cells, and ultimately IPCs have been reported. The differentiation protocols may vary depending on the cell source and culture conditions; however, they commonly employ growth factors, signalling molecules, and small molecules to guide differentiation. However, differentiation efficiency is the major limitation of the iPSCs-derived IPCs and thus, research on iPSCs-derived IPCs is progressing rapidly to improve the differentiation efficiency of iPSCs into IPCs. In one such attempt, Amer and colleagues generated the insulin-producing β-cells by modulating the TGF-β signalling at the later stage of the differentiation and results showed that time- specific inhibition and induction of TGF-β signalling are required during β-cell differentiation to achieve dynamic insulin release against glucose exposure. Moreover, a recent study by Kroon et al. developed a small molecule-based IPCs differentiation protocol and they achieved a high yield of functional IPCs that secreted insulin in response to glucose stimulation. Generation of IPCs from MSCs: MSCs are multipotent stem cells that can differentiate into several cell types, including adipocytes, osteocytes, and chondrocytes. Recent studies have demonstrated that MSCs are also differentiated into IPCs using various differentiation protocols involving stepwise induction of endoderm, pancreatic progenitor cells, and IPCs, similar to the protocols utilized for iPSCs and ESCs. Developed a novel approach to improving the functional stability of MSC-derived IPCs. They differentiated human MSCs into IPCs using a protocol that included nicotinamide, BMP-7, and exendin-4. They then encapsulated the IPCs in a hydrogel made from extracellular
- 53. matrix (ECM) proteins, which provided a supportive microenvironment for the cells. The researchers found that the IPCs in the hydrogel maintained their function and survival for up to 21 days in vitro, compared to only 7 days for IPCs without the hydrogel. They also transplanted the IPCs into diabetic mice and found that the hydrogel-encapsulated IPCs improved glucose tolerance and reduced hyperglycemia. Furthermore, in a recent study, human adipose-derived MSCs were exposed to a combination of cytokines and small molecules, including Activin A, BMP-4, retinoic acid, and the GSK-3β inhibitor CHIR99021. After 12 days of differentiation, the cells displayed morphological changes consistent with IPCs and expressed key beta cell markers, including insulin, PDX1, and NKX6.1. The resulting IPCs also exhibited glucose-stimulated insulin secretion, suggesting functional beta-cell activity. Current Status of Stem Cell Therapy for T1D Stem cells have the potential to differentiate into pancreatic β-cells, making them a promising source for cell-based therapies for T1D. Stem cells (ESCs, iPSCs, and adult stem cells) are among those being widely explored for T1D therapeutics In preclinical studies, ESCs-derived β-cells have demonstrated favorable results by secreting insulin in response to glucose stimulation and restoring normoglycemia in diabetic mouse models. However, the clinical translation of ESC-derived β-cells have been limited by ethical concerns and the risk of immune rejection. Thus, iPSCs offer a viable alternative to ESCs since they can be derived from adult somatic cells, thereby eliminating ethical concerns. iPSC-derived β- cells have also demonstrated the ability to secrete insulin and restore normoglycemia in diabetic mouse models. Yet, their clinical translation is still in its early stages, and further research is needed to establish their safety and efficacy. In addition to iPSCs, adult stem cells, including MSCs and hematopoietic stem cells (HSCs), have also been investigated for T1D therapy. Preclinical studies have shown that MSCs have the potential for β-cell regeneration and immune modulation, while HSCs can promote β-cell survival and function. Despite these exciting findings, the clinical translation of adult stem cells for T1D therapy is still in its infancy and requires further investigation to determine their safety and efficacy. In recent years, there have been several successful clinical trials of stem cell therapy for T1D have been carried out. One notable trial was conducted by Viacyte, Inc., involving the transplantation of pancreatic progenitor cells derived from stem cells into T1D patients. The implanted cells successfully differentiated into insulin-producing β-cells and effectively regulated the blood glucose levels in most patients without exerting serious adverse events. Another clinical trial involved the transplantation of autologous bone marrow-derived stem cells in patients with T1D, promoting the regeneration of pancreatic β-cells and improving glycaemic control in the majority of patients. In another effort, the use
- 54. of stem cell educator therapy in T1D involved exposing the blood of 15 patients to allogeneic umbilical cord blood-derived stem cells using a blood filtration device. Following treatment, the patients experienced improved blood glucose control, increased C-peptide levels, and reduced insulin requirements (Zhao et al., 2022). Another clinical trial involved 63 newly diagnosed T1D patients who received allogeneic MSC transplantation. Following the transplantation, the patients experienced improved blood glucose control, increased C-peptide levels, and reduced insulin requirements. In the current scenario, the diabetes epidemic has been a serious global health issue and the lack of an efficient and substantial therapy plays a significant role in the continuously increasing prevalence of diabetes. Recent advances in biomedical research led to the development of various diabetes management and therapeutic approaches (as summarized in Fig. 6) including immunotherapy, artificial pancreas, cell-based therapy, etc. which hold great promise for diabetes treatment through uniquely powerful modes of action. Immunotherapy relies on the modulation of the immune system which in turn, prevents the destruction of β-cells and preserves insulin production. However, early clinical studies have shown promising results but there are several unanswered questions about the optimal timing, dosing, and duration of
- 55. immunotherapy and long-term side effects still exist. The artificial pancreas can automatically regulate insulin delivery based on real-time glucose measurements. However, more accurate glucose sensors and the optimization of the control algorithms could make the artificial pancreas a better tool for diabetes treatment. Cell-based therapy including gene therapy, cell encapsulation, and stem cell therapy is gaining attention in diabetes therapeutics. In continuation, gene therapy is able to restore normal insulin production by delivering the genes that promote the growth and survival of β-cells or silencing the genes that contribute to β-cell destruction. However, the safety and efficiency of viral vectors, and the potential for off-target effects are the associated disadvantages of gene therapy. Stem cell therapy is one of the most promising approaches for the treatment of T1D, with several studies showing that it can improve glucose control and reduce the need for exogenous insulin. However, combination therapies that target different aspects of the disease pathogenesis may be necessary for optimal outcomes. Despite the challenges, the rapid pace of technological advancements and scientific discoveries in cellular therapies make them a promising area of research for the treatment of T1D. In a few short decades, type 2 diabetes research and technological breakthroughs have brought about significant advancements in how the condition is treated and managed. Here are some of the top innovations that are helping people with type 2 diabetes better manage the condition today. 1. Insulin Pumps The first insulin pump came on the market in 1974. Previously, insulin pumps were only approved for use in those with type 1 diabetes. But if you have type 2 diabetes and have to inject insulin multiple times a day, a pump is an alternative to self-injection. “An insulin pump is a medical device that delivers insulin into the tissue just underneath the skin,” says Megan Porter, RD, CDCES, a certified diabetes educator in Portland, Oregon. This computerized device, which is about the size of a deck of cards, can be worn around your waist, put in a pocket, secured with an armband, or attached to a belt or bra. “Some pumps deliver the insulin continuously, and others only deliver the insulin at meals or large snacks,” adds Porter. An insulin pump can also be more convenient if you’re out or at work, because all you may need to do is push a button to deliver the insulin instead of giving yourself a shot. 2. Continuous Glucose Monitors (CGMs) These devices have a tiny sensor that is placed below the surface of the skin to measure the amount of glucose in the fluid between cells every few minutes and transmit the data wirelessly to a device or your smartphone. CGMs are a game-changer: Unlike glucose meters that require a drop of blood to check what your blood glucose levels are at that moment, CGMs monitor your levels at set times throughout the day, such as every five minutes. This can help you and your doctor identify patterns and trends that may be helpful in fine-tuning
- 56. your type 2 diabetes treatment plan to optimize management, according to the American Diabetes Association (ADA). These devices can also alert you when your glucose level is too low or too high. The first CGM, which involved wearing a device provided by the doctor for two weeks or less and then returning it to the clinic or hospital, was approved by the U.S. Food and Drug Administration (FDA) in 1999. Since then, CGMs have become increasingly accurate and much more widely available for home use. In the past five years, there have been even more advances in CGM therapy. In 2018, the FDA approved the first implantable CGM device, which can be worn up to three months without changing the sensor, for people with type 1 or 2 diabetes. “The benefit of using a CGM is that it can be worn for seven or more days, which means one poke to insert the monitor [during that time frame] replaces checking blood sugars via a finger poke three or more times per day,” Porter notes. CGMs make it easier to check your blood sugar before and after meals, and they can help you understand how your diet, activity, and lifestyle affect your blood sugar levels. 3. Connected CGM-Insulin Pumps Another option available is a combination CGM-insulin pump, which enables the pump to use the data from the CGM to suggest changes in medication dosing or make necessary adjustments on its own. In 2020, the FDA approved an integrated CGM, which allows it to be connected to other diabetes management devices, such as insulin pumps and blood glucose monitors. Should You Try Cryotherapy to Help Rheumatoid Arthritis Symptoms? Read More This integration of devices can help improve type 2 diabetes management by quickly reducing blood sugar and minimizing the amount of time you experience unsafe and unhealthy blood sugar levels. 4. Diabetes Medications Although insulin has been used in the United States since the 1920s, according to the FDA, today’s medications can be far more targeted for specific diabetes issues. Metformin, which belongs to a class of medications called biguanides, is often the first medication prescribed for type 2 diabetes. “Metformin decreases glucose absorption from food and decreases liver production of insulin,” says Porter. Other options, including oral medications and noninsulin injectables: Sodium-glucose cotransporter-2 (SGLT2) inhibitors are oral medications that lower blood sugar levels by preventing the kidneys from absorbing glucose.
- 57. Glucagon-like peptide-1 receptor agonists (GLP-1 RAs) are injectable medications that help you control appetite and blood sugar levels. DPP-4 inhibitors, also called gliptins, are oral medications that help manage diabetes in several ways, such as by enhancing insulin secretion, slowing down digestion, and decreasing appetite, which can help with weight loss. Thiazolidinediones, also called glitazones, are oral medications that help make your body’s tissues more sensitive to insulin. Sulfonylureas are oral medications that increase the release of insulin from your pancreas. Meglitinides are oral medications that help your body make more insulin around mealtimes. Alpha-glucosidase inhibitors are oral medications that help your body digest sugar more slowly. Combination therapies join multiple drug classes in a single medication. They may be injected or taken orally. “And, of course, insulin is still used as a replacement when a person’s body does not create enough insulin on its own,” Porter adds. 5. Insulin Innovations Insulin has come a long way since it was first discovered. It now comes in a variety of forms, including rapid-acting, long-lasting, and premixed formulas, and can be delivered via a number of methods, such as syringes, pumps, and pens. And innovations are still coming. For instance, there are now insulin pen devices that can remember the last dose and the time that it was given, which is especially helpful if you’re busy or tend to forget to take it. Smart insulin pens have many of the features of insulin pumps but cost less and don’t have to be attached to your body. According to the ADA, smart insulin pens can connect to your smartphone or watch and link to diabetes data-tracking platforms to help you accurately calculate each dose based on factors such as your blood sugar level, carb amounts, meal size, and other parameters prescribed by your doctor. These devices can also remind you to take your dose, keep track of the amount of each dose, and tell you when your insulin has expired. 6. Easier-to-Use Glucagon Glucagon is used in emergencies to treat very low blood sugar, or hypoglycemia, a dangerous condition that can lead to confusion, loss of consciousness, seizures, and even death, according to the National Institute of Diabetes and Digestive and Kidney Diseases. Glucagon injections have been available for more than 20 years, but in the past few years, devices such as injectable pens and glucagon that can be inhaled have made it much easier for you — or your family or friends — to administer glucagon in the event of an emergency.
- 58. 7. Better Support for People With Diabetes In the past, many people with type 2 diabetes were treated by their primary care physician — rather than an endocrinologist, who is trained to treat diabetes — who may not have had any special training in the complexities of type 2 diabetes management. Today, there are many specialists who can help. Since the 1980s, certified diabetes educators have transformed diabetes management, according to the ADA. These professionals, who are now called certified diabetes care and education specialists (CDCES), take a comprehensive approach to teaching diabetes management and specialize in educating and supporting those with diabetes to optimize their health. Diabetes educators can also connect you to dietitians, physical therapists, and mental health experts trained to help with the condition. “Hopefully, over time, more people with chronic conditions, such as diabetes, will be referred out to other healthcare professionals who can help them manage their condition physically and mentally,” Porter says. 8. Diabetes Smartphone Apps Yes, there’s an app for that — many of them, in fact. Nowadays, diabetes apps can track your blood sugar levels and show trends; monitor your diet and suggest recipes; log your exercise; and provide support from other people with diabetes. “Coaching apps can also give you access to highly trained diabetes educators and fitness coaches,” Porter says. But it’s important to check with your doctor, CDCES, or other trusted diabetes health professional before you choose an app. An article in the journal Diabetes Care noted that there isn’t sufficient evidence to back up the effectiveness, accuracy, and safety of many apps, and many are plagued by technical problems. The authors noted that regulatory agencies and app companies urgently need to work with diabetes health professionals and researchers to ensure the safety and effectiveness of diabetes apps. 9. Meal Delivery Services While they weren’t developed specifically for diabetes, meal delivery companies that offer healthy foods and recipes have become very popular over the past several years. Now, many companies provide diabetes-friendly meal kits if you want to eat healthy but don’t want to do a lot of food shopping and planning.
- 60. The Department of Health & Family Welfare, Government of India provides technical and financial support to the States/UTs under the National Programme for Prevention and Control of Non Communicable Diseases (NP-NCD), as part of National Health Mission (NHM), based on the proposals received from the States/UTs and subject to the resource envelope. Diabetes is an integral part of the programme. The programme focusses on strengthening infrastructure, human resource development, health promotion & awareness generation for prevention, early diagnosis, management and referral to an appropriate level of healthcare facility for treatment of the Non-Communicable Diseases (NCDs). Under NP- NCD, 724 District NCD Clinics, 210 District Cardiac Care Units, 326 District Day Care Centres and 6110 Community Health Centre NCD Clinics have been set up.
- 61. A population-based initiative for prevention, control and screening for common Non-Communicable Diseases (NCDs) i.e., diabetes, hypertension and common cancers has been rolled out in the country under NHM and also as a part of Comprehensive Primary Health Care. Under the initiative, persons more than 30 years of age are targeted for their screening for common NCDs. Screening of these common NCDs is an integral part of service delivery under Ayushman Bharat – Health and Wellness Centres which generates awareness on risk factors of NCDs including diabetes. Preventive aspect of diabetes is strengthened under Comprehensive Primary Health Care through Ayushman Bharat Health Wellness Centre scheme, by promotion of wellness activities and targeted communication at the community level. In addition, NP-NCD gives financial support under NHM for awareness generation (IEC) activities for Diabetes to be undertaken by the States/UTs as per their Programme Implementation Plans (PIPs). Other initiatives for increasing public awareness about Diabetes and for promotion of healthy lifestyle include observation of World Diabetes Day and use of print, electronic and social media for continued community awareness. Furthermore, healthy eating is promoted through FSSAI. Eat Right Initiative, Safe and Nutritious Food at Home and ‘Aaj se thoda kum’ awareness activities are also initiated. This initiative aims to promote both the demand for and the supply of safe and healthy food in a sustainable way. Fit India and Khleo India movements are implemented by Ministry of Youth Affairs and Sports, and various Yoga related activities are carried out by Ministry of AYUSH. Diabetes patients are getting treatment at various health facilities in the health care delivery system including District Hospitals, Medical Colleges, Central Institutes like AIIMS, Central Government hospitals, and private sector hospitals. The treatment in Government Hospitals is either free or highly subsidized for the poor and needy. Under NP-NCD, glucometer and drugs for diabetes are provided as per the proposals received from the states. Under Free Drugs Service Initiative of NHM, financial support is provided to States/UTs for provision of free essential medicines including insulin for poor and needy people. Furthermore, quality generic medicines including insulin are made available at affordable prices to all, under ‘Pradhan Mantri Bhartiya Janaushadhi Pariyojana (PMBJP), in collaboration with the State Governments.
- 62. SESSION-4 COMPLICATIONS OF DIABETES [DIAGNOSIS AND MANAGEMENT]
- 63. HYPOGLYCEMIA (LOW BLOOD SUGAR) Hypoglycemia happens when the level of sugar (glucose) in blood drops below the range that’s healthy for you. It’s also called low blood sugar or low blood glucose. Hypoglycemia is common in people with diabetes, especially Type 1 diabetes. For most people with diabetes, hypoglycemia is when blood sugar level is below 70 milligrams per deciliter (mg/dL) or 3.9 millimoles per liter (mmol/L). For most people without diabetes, hypoglycemia is when blood sugar level is below 55 mg/dL or 3.1 mmol/L. Hypoglycemia requires immediate treatment by eating or drinking sugar/carbohydrates. Severe hypoglycemia can be life- threatening and requires treatment with emergency glucagon and/or medical intervention. Glucose (sugar) mainly comes from carbohydrates in the food and drinks we consume. It’s body’s main source of energy. Glucose is very important because it’s the primary source of energy for brain. If don’t have diabetes, several bodily processes naturally help keep blood glucose in a healthy range. Insulin, a hormone pancreas makes, is the most significant contributor to maintaining healthy blood sugar. Glucagon is another important hormone in this process. People who have diabetes must use medication, like oral diabetes medications or synthetic insulin, and/or lifestyle changes to help keep their blood sugar levels in range. Low blood sugar often happens due to excess insulin — whether body naturally makes too much or inject too much synthetic insulin. Other hormonal and metabolic issues can also lead to low blood sugar. If blood sugar drops below the healthy range, it causes certain symptoms like shakiness and a faster heartbeat and can be life-threatening if it goes too low. This is because your brain needs a continuous supply of glucose to function properly. Without enough glucose, your brain can’t function. Hypoglycemia is common in people with diabetes, especially people who take insulin to manage the condition. One study found that 4 in 5 people with Type 1 diabetes and nearly half of all people with Type 2 diabetes who take insulin reported a low blood sugar episode at least once over a four-week period. People with Type 2 diabetes who take meglitinide or sulfonylurea oral diabetes medications are also at an increased risk for low blood sugar.
- 64. Causes: Hypoglycemia happens when blood sugar drops below a healthy range. Several factors can contribute to this for people with diabetes. Hypoglycemia can develop if things like food, exercise and diabetes medications are out of balance. Common situations that can lead to hypoglycemia for people with diabetes include: Taking too much insulin, the wrong insulin or injecting it into your muscle instead of in your fat tissue. Not timing insulin and carb intake correctly (for example, waiting too long to eat a meal after taking insulin for the meal). Taking too much or too high of a dose of oral diabetes medications. Being more active than usual. Drinking alcohol without eating. Eating meals later than usual or skipping meals. Not balancing meals by including fat, protein and fiber. People who are pregnant and have Type 1 diabetes are also more likely to experience low blood sugar during the first trimester due to hormone changes. There are two main types of non-diabetes-related hypoglycemia: Reactive hypoglycemia and fasting hypoglycemia. Reactive hypoglycemia happens when experience low blood sugar after a meal. It typically occurs about two to four hours after a meal. Researchers don’t yet know the exact cause. But they think it happens due to a sudden spike and then fall in blood sugar after eating certain foods, especially simple carbohydrate foods like white rice, potatoes, white bread, cake and pastries. Bariatric surgery can also result in reactive hypoglycemia. After certain types of bariatric surgery, such as gastric bypass surgery, your body absorbs sugars very quickly, which stimulates excess insulin production. This can then cause hypoglycemia. Your body usually corrects reactive hypoglycemia on its own, but consuming carbohydrates may help your symptoms go away more quickly. Fasting hypoglycemia: For the majority of people without diabetes, not eating food for a long time (fasting) doesn’t lead to hypoglycemia. This is because your body uses hormones and stored glucose to manage your blood sugar. However, certain conditions and situations can lead to fasting hypoglycemia in people without diabetes, including: Excessive alcohol consumption: Alcohol prevents your body from forming new glucose cells (gluconeogenesis). If you drink excessive amounts of alcohol over
- 65. several days and don’t eat much, your body can run out of stored glucose (glycogen). This can lead to hypoglycemia because your body can’t properly regulate your blood sugar. Critical illness: You can experience hypoglycemia in critical illness states, such as end-stage liver disease, sepsis, starvation or kidney failure. This is because your body is using stored glucose for energy faster than your body can create new glucose cells from the food you eat. Adrenal insufficiency: Adrenal insufficiency causes lower-than-normal cortisol levels. As cortisol (a hormone) helps regulate your blood sugar by increasing it, having low levels of cortisol can lead to hypoglycemia episodes. Non-islet cell tumor hypoglycemia (NICTH): This is a rare but serious syndrome in which a tumor releases excess insulin-like growth factor 2 (IGF-2). This is a hormone that has similar effects as insulin. Excess IGF-2 causes hypoglycemia. A wide variety of benign (noncancerous) and malignant (cancerous) tumors can cause NICTH. Insulinoma: An insulinoma is a rare tumor in your pancreas that produces excess insulin. It leads to hypoglycemia episodes — most commonly in the early morning.In rare cases, non-diabetes-related medications can lead to hypoglycemia, such as beta-blockers and certain antibiotics. If you’re experiencing hypoglycemia and don’t have diabetes, talk to your healthcare provider. Common symptoms of hypoglycemia include shaking or trembling, faster heart rate, extreme hunger, sweating, dizziness and more. Symptoms of hypoglycemia (low blood sugar) can start quickly, and they can vary from person to person. The signs include: Shaking or trembling, Weakness, Sweating and chills, Extreme hunger (polyphagia), Faster heart rate, Dizziness or lightheadedness, Confusion or trouble concentrating, Anxiety or irritability., Color draining from your skin (pallor), Tingling or numbness in your lips, tongue or cheeks. Signs of severe hypoglycemia include: Blurred or double vision, Slurred speech, Clumsiness or difficulty with coordination, Being disoriented, Seizures, Loss of consciousness. Severe hypoglycemia is life-threatening. It needs immediate medical treatment. In rare cases, severe hypoglycemia that isn’t treated can result in a coma and/or death.
- 66. Can also experience low blood sugar while sleeping (nocturnal hypoglycemia). Symptoms may include: Restless sleep, Sweating through your pajamas or sheets, Crying out during sleep, having nightmares, Feeling tired, disoriented or confused after waking up. In general, symptoms often begin for people with diabetes when their blood glucose is around 70 mg/dL or lower. If blood sugar is falling rapidly, may experience symptoms before this point. If have hypoglycemia unawareness, it’s important to let friends and family know so that they know how to help if experience a severe low blood sugar episode. You may also benefit from the following: Using a continuous glucose monitoring (CGM) device that can alert you when you have hypoglycemia. More frequent manual blood sugar checks. A service dog called a diabetes alert dog that’s specially trained to alert you when you have low blood sugar. Prolonged severe hypoglycemia is life-threatening and can lead to the following complications: Multiple organ failure, Cardiac arrhythmias, Cardiac arrest, Permanent brain damage, Coma, Death. Operating heavy equipment, such as driving a vehicle, while having low blood sugar can also be dangerous. You may be more likely to get in an accident. If you have diabetes, always make sure your blood sugar is in range before operating heavy equipment. Diagnosis and Tests: The only way to know if you have hypoglycemia is to check blood sugar with a blood glucose meter (glucometer). Most of these devices use a tiny blood sample from a finger prick with a lancet (small needle). If you’re experiencing symptoms of hypoglycemia and are unable to check blood sugar, treat the hypoglycemia. If healthcare provider suspects have hypoglycemia, they may check blood sugar every few hours during a fast lasting several days. For reactive hypoglycemia, provider might recommend a test called a mixed-meal tolerance test (MMTT). For the MMTT, first have a special drink containing protein, fats and sugar. The drink raises blood glucose, causing body to make more insulin. Then a provider will check blood glucose multiple times over the next five hours. Management and Treatment: Treat mild to moderate hypoglycemia by eating or drinking sugar (carbohydrates). The American Diabetes Association recommends the “15-15 rule” to treat an episode of mild to moderate hypoglycemia:
- 67. Eat or drink 15 grams of fast-acting carbs to raise blood sugar. After 15 minutes, check blood sugar. If it’s still below 70 mg/dL, have another 15 grams of fast-acting carbs. Repeat until blood sugar is at least 70 mg/dL. To know how many carbs eating, read food nutrition labels. Some examples of foods that contain about 15 grams of fast-acting carbs include: 1 small piece of fruit, such as half a banana. 4 ounces (half-cup) of juice or regular soda (not diet). 1 tablespoon of sugar, honey or syrup. 1 tube of instant glucose gel (check the instructions). 3 to 4 glucose tablets (check the instructions). If have symptoms of hypoglycemia but can’t check blood sugar, use the 15-15 rule until feel better. Children may need fewer grams of carbs to treat hypoglycemia. Check with your child’s healthcare provider. Severe hypoglycemia requires different treatment than mild or moderate hypoglycemia. If someone you know is having a hypoglycemia episode and is slurring their speech, disoriented or unconscious, don’t give them food or liquid. They could choke. Severe hypoglycemia episodes require the use of emergency glucagon. This is a synthetic form of glucagon that you can administer as an injection or nasal powder (dry nasal spray), depending on the type. Synthetic glucagon triggers your liver to release stored glucose, which then raises blood sugar. If the glucagon is injectable, inject it into their butt, arm or thigh, following the instructions in the kit. If the glucagon is a nasal powder, follow the instructions on the package to administer it into their nostril. When the person regains consciousness (usually in 5 to 15 minutes), they may experience nausea and vomiting. If they’re laying down, roll them onto their side to prevent choking in case they vomit. Don’t hesitate to call 911 for help. If someone is unconscious and glucagon isn’t available or you don’t know how to use it, call 911 immediately. Prevention: It’s easiest to do this when healthcare provider understand what causes blood sugar to drop. Give healthcare provider as much information as
