Xantogranuloma Juvenil Congênito Gigante
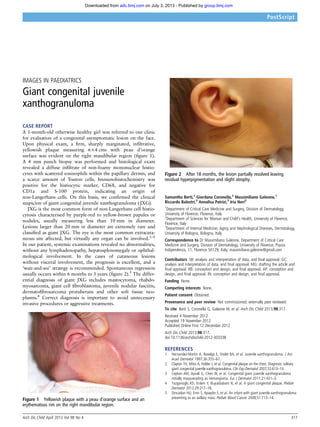
- 1. IMAGES IN PAEDIATRICS Giant congenital juvenile xanthogranuloma CASE REPORT A 1-month-old otherwise healthy girl was referred to our clinic for evaluation of a congenital asymptomatic lesion on the face. Upon physical exam, a firm, sharply marginated, infiltrative, yellowish plaque measuring 6×4 cms with peau d’orange surface was evident on the right mandibular region (figure 1). A 4 mm punch biopsy was performed and histological exam revealed a diffuse infiltrate of non-foamy mononuclear histio- cytes with scattered eosinophils within the papillary dermis, and a scarce amount of Touton cells. Immunohistochemistry was positive for the histiocytic marker, CD68, and negative for CD1a and S-100 protein, indicating an origin of non-Langerhans cells. On this basis, we confirmed the clinical suspicion of giant congenital juvenile xanthogranuloma ( JXG). JXG is the most common form of non-Langerhans cell histio- cytosis characterised by purple-red to yellow-brown papules or nodules, usually measuring less than 10 mm in diameter. Lesions larger than 20 mm in diameter are extremely rare and classified as giant JXG. The eye is the most common extracuta- neous site affected, but virtually any organ can be involved.1–4 In our patient, systemic examinations revealed no abnormalities, without any lymphadenopathy, hepatosplenomegaly or ophthal- mological involvement. In the cases of cutaneous lesions without visceral involvement, the prognosis is excellent, and a ‘wait-and-see’ strategy is recommended. Spontaneous regression usually occurs within 6 months to 3 years (figure 2).5 The differ- ential diagnosis of giant JXG includes mastocytoma, rhabdo- myosarcoma, giant cell fibroblastoma, juvenile nodular fasciitis, dermatofibrosarcoma protuberans and other soft tissue neo- plasms.4 Correct diagnosis is important to avoid unnecessary invasive procedures or aggressive treatments. Samantha Berti,1 Giordana Coronella,2 Massimiliano Galeone,1 Riccardo Balestri,3 Annalisa Patrizi,3 Iria Neri3 1 Department of Critical Care Medicine and Surgery, Division of Dermatology, University of Florence, Florence, Italy 2 Department of Sciences for Woman and Child’s Health, University of Florence, Florence, Italy 3 Department of Internal Medicine, Aging and Nephrological Diseases, Dermatology, University of Bologna, Bologna, Italy Correspondence to Dr Massimiliano Galeone, Department of Critical Care Medicine and Surgery, Division of Dermatology, University of Florence, Piazza Indipendenza, 11, Florence 50129, Italy; massimiliano.galeone@gmail.com Contributors SB: analysis and interpretation of data, and final approval. GC: analysis and interpretation of data, and final approval. MG: drafting the article and final approval. RB: conception and design, and final approval. AP: conception and design, and final approval. IN: conception and design, and final approval. Funding None. Competing interests None. Patient consent Obtained. Provenance and peer review Not commissioned; externally peer reviewed. To cite Berti S, Coronella G, Galeone M, et al. Arch Dis Child 2013;98:317. Received 4 November 2012 Accepted 19 November 2012 Published Online First 12 December 2012 Arch Dis Child 2013;98:317. doi:10.1136/archdischild-2012-303338 REFERENCES 1 Hernandez-Martin A, Baselga E, Drolet BA, et al. Juvenile xanthogranuloma. J Am Acad Dermatol 1997;36:355–67. 2 Clayton TH, Mitra A, Holder J, et al. Congenital plaque on the chest. Diagnosis: solitary giant congenital juvenile xanthogranuloma. Clin Exp Dermatol 2007;32:613–14. 3 Ceyhan AM, Aynali G, Chen W, et al. Congenital giant juvenile xanthogranuloma initially masquerading as hemangioma. Eur J Dermatol 2011;21:431–3. 4 Yazganoglu KD, Erdem Y, Buyukbabani N, et al. A giant congenital plaque. Pediatr Dermatol 2012;29:217–18. 5 Dincaslan HU, Emir S, Apaydin S, et al. An infant with giant juvenile xanthogranuloma presenting as an axillary mass. Pediatr Blood Cancer 2008;51:713–14.Figure 1 Yellowish plaque with a peau d’orange surface and an erythematous rim on the right mandibular region. Figure 2 After 18 months, the lesion partially resolved leaving residual hyperpigmentation and slight atrophy. Arch Dis Child April 2013 Vol 98 No 4 317 PostScript group.bmj.comon July 3, 2013 - Published byadc.bmj.comDownloaded from
- 2. doi: 10.1136/archdischild-2012-303338 2012 2013 98: 317 originally published online December 12,Arch Dis Child Samantha Berti, Giordana Coronella, Massimiliano Galeone, et al. Giant congenital juvenile xanthogranuloma http://adc.bmj.com/content/98/4/317.full.html Updated information and services can be found at: These include: References http://adc.bmj.com/content/98/4/317.full.html#ref-list-1 This article cites 5 articles service Email alerting the box at the top right corner of the online article. Receive free email alerts when new articles cite this article. Sign up in Collections Topic (159 articles)Surgical diagnostic tests (167 articles)Surgery (502 articles)Radiology (120 articles)Journalology (1226 articles)Immunology (including allergy) (586 articles)Clinical diagnostic tests (81 articles)Competing interests (ethics) (132 articles)Pathology (2179 articles)Child health (225 articles)Dermatology (467 articles)Oncology Articles on similar topics can be found in the following collections Notes http://group.bmj.com/group/rights-licensing/permissions To request permissions go to: http://journals.bmj.com/cgi/reprintform To order reprints go to: http://group.bmj.com/subscribe/ To subscribe to BMJ go to: group.bmj.comon July 3, 2013 - Published byadc.bmj.comDownloaded from
