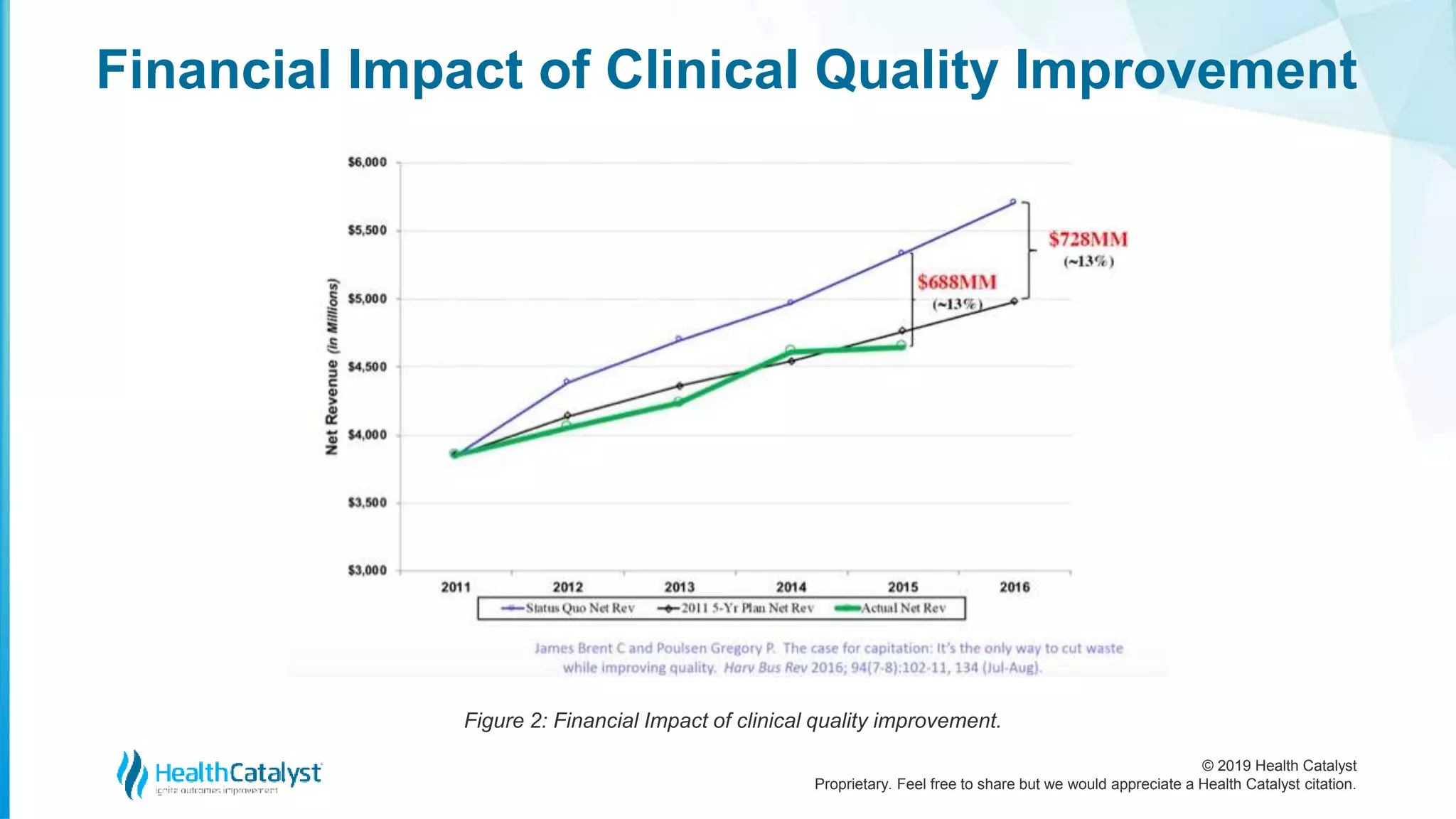
The document discusses the importance of healthcare quality improvement as a core business strategy, emphasizing that high-quality clinical care can significantly enhance financial performance by reducing waste and improving outcomes. Key challenges in healthcare include variation in clinical practices, inappropriate care, preventable patient injuries, and waste, which collectively represent substantial opportunities for improvement. Implementing team-based care approaches can lead to reduced costs and better patient outcomes, supporting the transition towards a pay-for-value model in healthcare.














![© 2019 Health Catalyst
Proprietary. Feel free to share but we would appreciate a Health Catalyst citation.
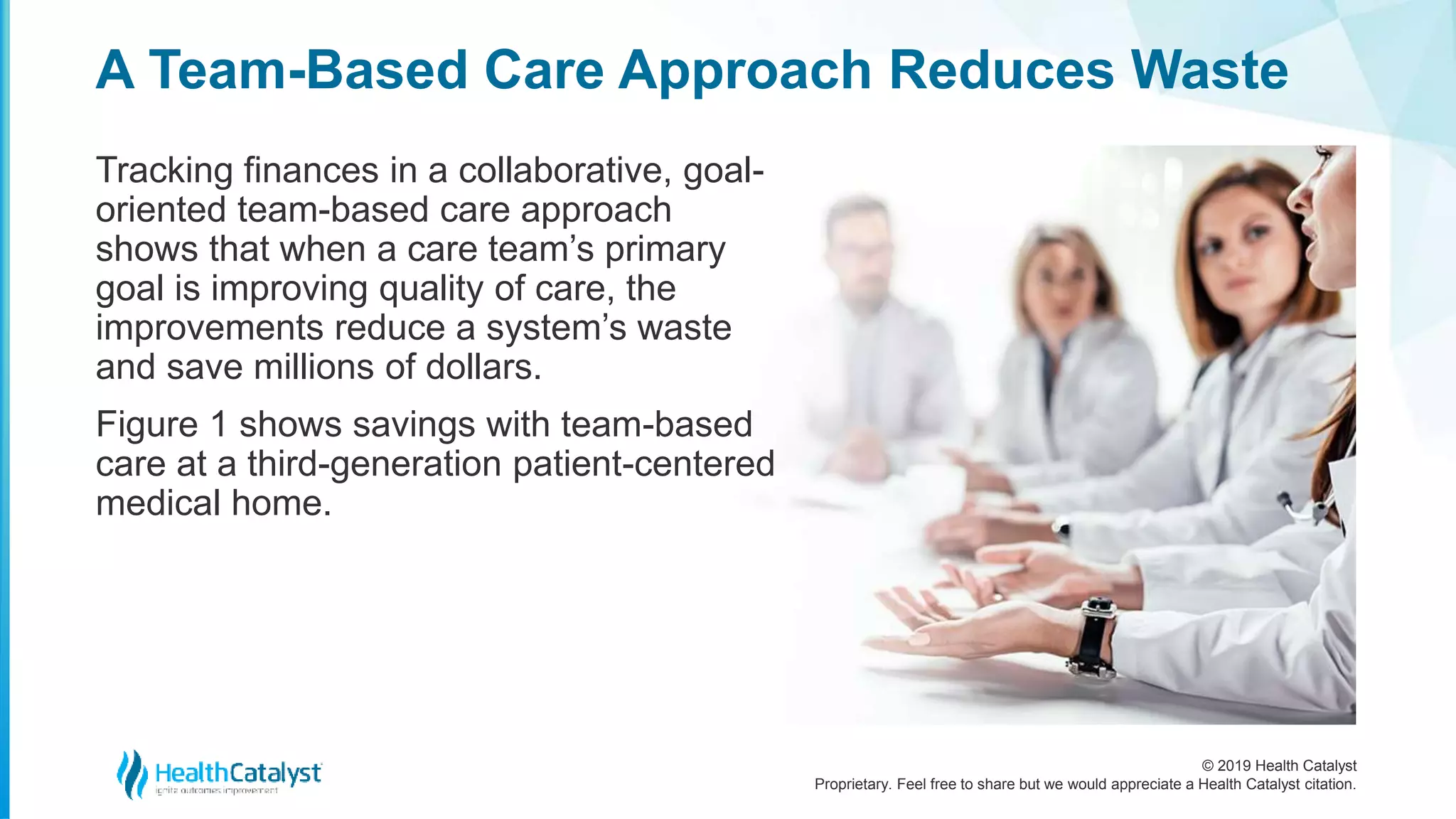
Overall, the investment in a team-based approach produced
better care at reduced expense (specifically, a conservative
investment of $22 per-member-per year [PMPY]).
For every dollar spent, the team-based approach earned $5
back for a total savings of $115 PMPY, mostly by reducing
hospital admits, other avoidable specialties,
and outpatient procedure care.
A Team-Based Care Approach Reduces Waste](https://image.slidesharecdn.com/healthcarequalityimprovement-afoundationalbusinessstrategy-200114195949/75/Healthcare-Quality-Improvement-A-Foundational-Business-Strategy-21-2048.jpg)