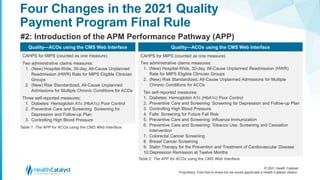
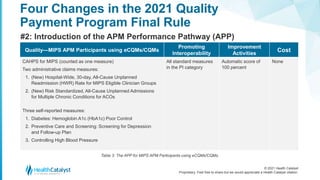
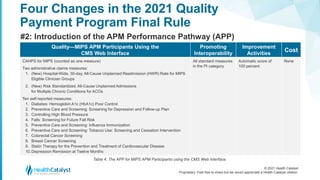
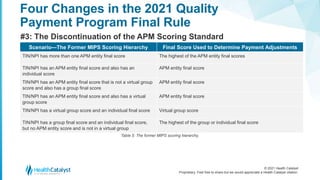
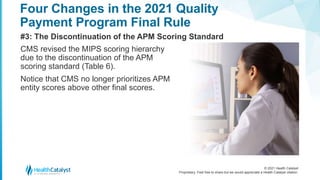
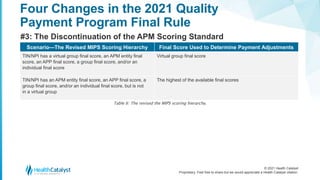
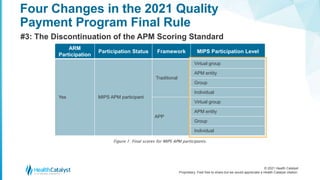
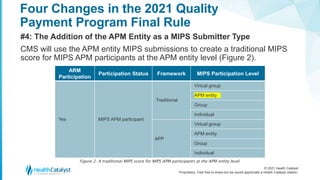
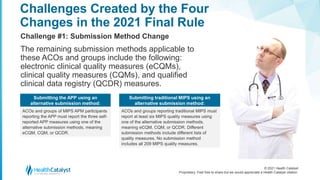
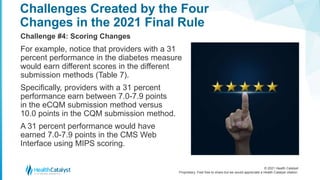
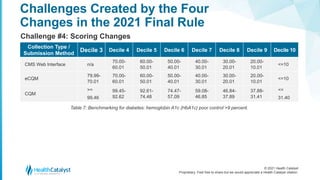
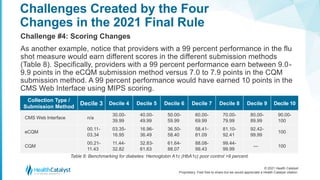
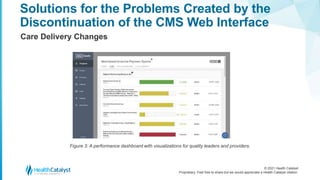
The document outlines four significant changes to the Quality Payment Program for 2021, specifically affecting Accountable Care Organizations (ACOs) and MIPS APM participants. Key changes include the discontinuation of the CMS web interface for reporting quality data, the introduction of the APM performance pathway, and updates to the MIPS scoring hierarchy. These changes introduce new challenges in quality measurement and compliance for ACOs and MIPS participants, necessitating adapted strategies to meet the new guidelines.