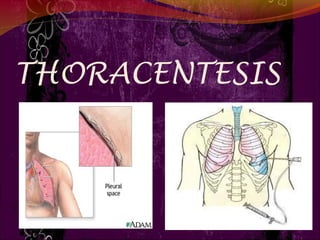
Thoracentesis
- 1. 1
- 2. DEFINITION Thoracentesis is a procedure to remove fluid from the space between the lungs and the chest wall called the pleural space. Thoracentesis is a procedure that removes an abnormal accumulation of fluid or air from the chest through a needle or tube.
- 3. PURPOSE To determine the cause of abnormal accumulation of fluid in the pleural space. Relieve shortness of breath and pain As a diagnostic or treatment procedure To drain large amounts of pleural fluid To equalize pressure on both sides of the thoracic cavity
- 4. INDICATION Traumatic pneumothorax Hemopneumothorax Spontaneous pneumothorax Bronchopleural fistula Pleural effusion
- 5. CONTRAINDICATION An uncooperative patient Coagulation disorder Atelectasis Only one functioning lung Emphysema(pulmonary enlargement) Severe cough or hiccups
- 6. COMPLICATION Pulmonary edema Bleeding Respiratory distress Infection Air embolism Dyspnea and cough Cardiac tamponade(fluid build up in the space Atelectasis(lung between myocardium and collapes) pericardium)
- 7. 7
- 8. BEFORE THE PROCEDURE Explain the purpose, risks/benefits, and steps of the procedure and obtain consent from the patient or appropriate legal design. R: An explanation helps orient the patient to the procedure assist in coping and provide an opportunity to ask question and verbalise anxiety
- 9. CON’T… Take Medical History such as Trouble in breathing, coughing, and hiccups Had heart disease Smoked Travelled to places where may have been exposed to tuberculosis R: to detect any abnormalities regarding the procedure 9
- 10. • Prepare Equipment Dressing set Povidone / Alcohol Abraham’s needle Local anaesthetic, e.g. lignocaine (lidocaine) 1% Connecting tubing or 2% Syringe 50ml and 5ml Formalin bottle Scapel blade and blade 11 Urine bottle x2 Needles (18 and 23 C+S bottle gauge) 3-way stopcock Sterile Glove Fenestrated towel Mask Jug
- 11. BEFORE THE PROCEDURE Check platelet count and/or presence of coagulopathy. If platelet count is < 20,000, or there is known coagulopathy as to whether platelet transfusion or other intervention is needed R: To prevent complication such as bleeding while during procedure.
- 12. Place patient upright / cardiac position and help patient maintain position during procedure. R: the upright position ensures that the diaphragm is more dependent and facilitates the removal of fluid that usually localizes at the base of the chest. Explain that he/she will receive a local anesthetic R: to minimize pain during the procedure. Clean patient skin with antiseptic soap R: To prevent infection and maintain aseptic technique.
- 14. DURING PROCEDURE Observe patient respiration rate and breathing pattern. R: to provide base line data to estimate patient tolerance of procedure Assess patient vital sign such as B/P, pulse R: To prevent any complication such as hypovolemic shock during procedure. Observe patient level of consciousness and give emotional support R: To reduce patient anxiety
- 15. DURING PROCEDURE Monitor saturation R: To prevent hypoxia Inform doctor if any changes of the patient R: To make sure whether need to continue the procedure or stop immediately.
- 16. AFTER PROCEDURE Obtain a chest x-ray to evaluate the fluid level. R: To compare the conditions of the lungs before and after the procedure. For specimen handling, fill the tubes with the required amount of pleural fluid R : To prevent over intake of the fluid to the specimen bottle. Check that each bottle is correctly labelled by checking patient identifiers- full name, date of birth and/or medical record number then send to the lab tests R: To prevent from incorrect results to the patient.
- 17. AFTER PROCEDURE Document the procedure, patient’s response, characteristics of fluid and amount, and patient response to follow-up. R: To develop further treatment to the patient. Provide post-procedural analgesics as needed. R: To prevent patient from pain related to the incision site.
- 18. AFTER PROCEDURE Rest in bed for about 2 hours after the procedure R: To minimize patient activity due to complication such as dyspnea. Blood pressure and breathing will be checked for up to a few hours R: to make sure don't have complications
- 19. AFTER PROCEDURE May remove dressing/bandage another day, or replace it if it becomes soiled or wet R: To prevent from getting infection. Resume patient regular diet. R: To promote wound healing.
- 20. THANK YOU !!!
