111318, 10(24 PMThe Civil War and Industrialization Scoring .docx
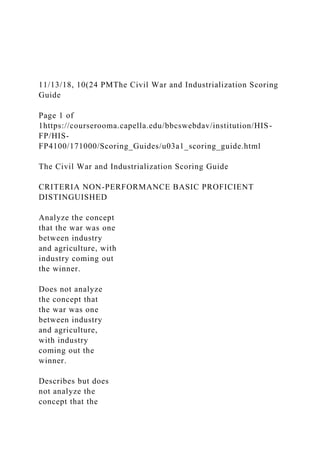
- 1. 11/13/18, 10(24 PMThe Civil War and Industrialization Scoring Guide Page 1 of 1https://courserooma.capella.edu/bbcswebdav/institution/HIS- FP/HIS- FP4100/171000/Scoring_Guides/u03a1_scoring_guide.html The Civil War and Industrialization Scoring Guide CRITERIA NON-PERFORMANCE BASIC PROFICIENT DISTINGUISHED Analyze the concept that the war was one between industry and agriculture, with industry coming out the winner. Does not analyze the concept that the war was one between industry and agriculture, with industry coming out the winner. Describes but does not analyze the concept that the
- 2. war was one between industry and agriculture, with industry coming out the winner. Analyzes the concept that the war was one between industry and agriculture, with industry coming out the winner. Analyzes the concept that the war was one between industry and agriculture, with industry coming out the winner using examples and citations from peer-reviewed sources. Examine ways in which the Civil War was a catalyst for economic change. Does not examine ways in which the Civil War was a catalyst for economic change. Lists ways in which
- 3. the Civil War was a catalyst for economic change. Examines ways in which the Civil War was a catalyst for economic change. Examines ways in which the Civil War was a catalyst for economic change using examples and citations from peer-reviewed sources. Analyze how the cultural shift after the Civil War was not easily embraced. Does not analyze how the cultural shift after the Civil War was not easily embraced. Describes how the cultural shift after the Civil War was not easily embraced. Analyzes how the cultural shift after the Civil
- 4. War was not easily embraced. Analyzes how the cultural shift after the Civil War was not easily embraced using examples and citations from peer-reviewed sources. Explain how the Civil War still has an emotional impact on people living today. Does not explain how the Civil War still has an emotional impact on people living today. List ways in which the Civil War still has an emotional impact on people living today. Explains how the Civil War still has an emotional impact on people living today.
- 5. Analyzes how the Civil War still has an emotional impact on people living today. Analyze the economics of slavery. Does not analyze the economics of slavery. Discusses the economics of slavery. Analyzes the economics of slavery. Analyzes the economics of slavery using real-world examples and citations from peer-reviewed sources. Communicate effectively in a variety of formats. Does not communicate effectively in a variety of formats. Communicates in a manner that is
- 6. effective but sometimes lacks clarity, conciseness, organization, or proper grammar. Communicates effectively in a variety of formats. Communicates in a professional manner using scholarly resources that support the analysis by connecting concepts through clear, concise, well-organized, and grammatically correct writing that incorporates appropriate APA style conventions. Research Original Investigation Preventing 30-D ay Hospital Readmissions A Systematic Review and Meta-analysis of Randomized Trials Aaron L. Leppin. MD; Michael R. Gionfriddo, PharmD; Maya Kessler, MD; Juan Pablo Brito, MBBS; Frances S. Mair, MD; Katie Gallacher, MBChB; Zhen Wang, PhD; Patricia J. Erwin. MLS; Tanya Sylvester, BS; Kasey Boehmer, BA; Henry H. Ting, MD, MBA; M. Hassan Murad, MD; Nathan D. Shippee, PhD; V ictor M. Montori, MD
- 7. IMPORTANCE Reducing early (<30 days) hospital readmissions is a policy priority aimed at improving health care quality. The cumulative complexity model conceptualizes patient context. It predicts that highly supportive discharge interventions will enhance patient capacity to enact burdensome self-care and avoid readmissions. OBJECTIVE To synthesize the evidence o f the efficacy o f interventions to reduce early hospital readmissions and identify intervention features- including their impact on treatment burden and on patients' capacity to enact postdischarge self- care-that might explain their varying effects. DATA SOURCES We searched PubMed, Ovid MEDLINE, Ovid EMBASE, EBSCO CINAHL, and Scopus (1990 until April 1,2013), contacted experts, and reviewed bibliographies. s t u d y SELECTION Randomized trials that assessed the effect o f interventions on all-cause or unplanned readmissions within 30 days o f discharge in adult patients hospitalized for a medical or surgical cause for more than 24 hours and discharged to home. DATA EXTRACTION a n d SYNTHESIS Reviewer pairs extracted trial characteristics and used an activity-based coding strategy to characterize the interventions; fidelity was confirmed with authors. Blinded to trial outcomes, reviewers noted the extent to which interventions placed additional work on patients after discharge or supported their
- 8. capacity for self-care in accordance w ith the cumulative complexity model. m a in outcomes a n d measures Relative risk o f all-cause or unplanned readmission w ith or w ithout out-of-hospital deaths at 30 days postdischarge. RESULTS In 42 trials, the tested interventions prevented early readmissions (pooled random-effects relative risk, 0.82 [95% Cl, 0.73-0.91]; P < .001; I2 = 31%), a finding that was consistent across patient subgroups. Trials published before 20 0 2 reported interventions that were 1.6 times more effective than those tested later (interaction P = .01). In exploratory subgroup analyses, interventions with many components (interaction P = .001), involving more individuals in care delivery (interaction P = .05), and supporting patient capacity for self-care (interaction P = .04) were 1.4,1.3, and 1.3 times more effective than other interventions, respectively. A post hoc regression model showed incremental value in providing comprehensive, postdischarge support to patients and caregivers. CONCLUSIONS AND relevance Tested interventions are effective at reducing readmissions, but more effective interventions are complex and support patient capacity for self-care. Interventions tested more recently are less effective. JAMA Intern Med. 2014:174(7):1095-1107. doLlO.lOOl/jamainternmed.2014.1608 Published online May 12,2014.
- 9. Author Affiliations: Author affiliations are listed at the end of this article. Corresponding Author: Victor M. Montori, MD, Knowledge and Evaluation Research Unit, Department of Medicine, Mayo Clinic, 200 First StSW, Plummer Bldg, Rochester. MN 55905 (montori.victor @mayo.edu). [J Supplemental con tent at jamainternalmedicine.com 1095 R e s e a rc h O r ig in a l In v e s tig a t io n P r e v e n tin g 3 0 - D a y H o s p ita l R e a d m is s io n s E arly hospital readm issions have been recognized as a com m on and costly occurrence, particularly am ong el- derly and high-risk patients. One in 5 Medicare benefi- ciaries is readm itted w ithin 30 days, for example, at a cost of m ore th an $26 billion per year.1 To encourage im provem ent in th e quality o f care and a reduction in unnecessary health ex- pense, policymakers, reim bursem ent strategists, and the US governm ent have m ade reducing 30-day hospital read m is- sions a national priority.2"4 Achieving th is goal, however, re- quires a more complete understanding of the underlying causes o f readm ission.
- 10. The cum ulative com plexity m odel (CuCoM)5 is a fram e- work developed by our research group th at conceptualizes p a- tie n t co n tex t as a balance b etw e en w orkload an d capacity (Figure 1). Workload consists o f all th e work of being a patient and includes efforts to u n d erstan d and plan for care, to enroll th e s u p p o rt o f o th e rs , an d to access an d u se h e a lth care services.6,7 Capacity is determ ined by th e quality and avail- ability o f resources th a t patients can mobilize to carry out this work (physical an d m ental health, social capital, financial re- sources, and environm ental assets). The CuCoM is novel in its consideration of th e effects o f treatm ent burden on patient con- text, and it illustrates how infeasible, u n su p p o rted , and con- text-irreverent care can lead to poor health outcom es and re- du ced h ea lth care effectiveness. Because p atien ts recently discharged from th e hospital are in a state o f extrem e physi- ologic and psychological vulnerability,8 their capacity for en - acting self-care is low. The CuCoM predicts th at, unless suffi- cient support is given to enhance patient and caregiver capacity to carry o u t th e work o f patienthood, placing highly b u rd en - some discharge dem ands on these patients will lead to poor outcom es and hospital readm ission. To evaluate th e validity o f th e CuCoM and provide hy- pothesis-generating work in th e understanding of patient con- text, we chose to synthesize th e evidence on the efficacy of interventions to reduce early hospital readm issions. In p ar- ticular, we sought to determ ine th e degree to w hich a n u m - ber o f intervention ch aracteristics-in clu d in g their im pact
- 11. on p a tie n t cap acity an d w o rk lo a d -m ig h t acco u n t for d iffer- ences in their effectiveness. F ig u r e 1. T h e C u m u l a t i v e C o m p l e x i t y M o d e l P a tie n t c o n t e x t is r e p r e s e n te d as a b a la n c e b e t w e e n w o r k lo a d a n d c a p a c ity . T h is b a la n c e m u s t b e o p t im iz e d t o e n s u r e c a re e ffe c tiv e n e s s a n d im p r o v e o u t c o m e s . In t u r n , t h e o u t c o m e s a c h ie v e d fe e d b a c k t o a f f e c t t h e w o r k lo a d - c a p a c ity b a la n c e . Methods A registered protocol (PROSPERO CRD42013004773) guided the conduct o f this review,9 w hich we report in adherence to th e Preferred Reporting Item s for Systematic Reviews and M eta- analyses (PRISMA) S tatem ent.10 Eligibility Criteria Eligible studies were random ized trials reported in English or Spanish, since 1990, th a t assessed th e effectiveness o f peri- discharge interventions vs any com parator on th e risk of early (ie, w ithin 30 days o f discharge) all-cause or u n p lan n ed read- m issions w ith or w ith o u t out-of-hospital deaths. The in te r- vention had to focus its efforts on th e hospital-to-hom e tra n - sition, perm it patients across arm s to have otherw ise similar
- 12. in p atien t experiences, and be generalizable to contexts b e - yond a single p atien t diagnosis. Adult patients had to be a d - m itted from th e com m unity to an inpatient ward for at least 24 hours w ith a medical or surgical cause. Studies including o b ste tric or p sy ch iatric ad m issio n s or only in clu d in g d is- charges to skilled n u rsin g or reh a b ilita tio n facilities w ere excluded. Info rm ation Sources In co lla b o ra tio n w ith an e x p e rie n c e d re s e a rc h lib ra ria n (P.J.E.), w e se a rc h e d in April o f 2013 th e follow ing d a ta - b a s e s : P u bM ed, Ovid MEDLINE, Ovid EMBASE, EBSCO CINAHL, a n d S co p u s. T h e c o m p le te s e a rc h s tr a te g y is re p o rte d in eA ppendix 1 (in S u p plem ent). Two review ers (T.S. a n d A .L.L.) h a n d - s e a r c h e d th e b ib lio g ra p h ie s o f in c lu d ed stu d ie s an d rec en t review s. E xperts in th e field w ere asked to identify additional references. Study Selection F our rev ie w ers (A.L.L., M.R.G., J.P.B., a n d T.S.) w o rk ed in d e p en d e n tly an d co n sid ered th e eligibility o f c an d id ate articles by exam ining th eir titles and abstracts, and th en th e full version o f articles identified as potentially eligible by at least 1 reviewer. Conflicts about th e eligibility of full articles w ere resolved by discussion an d consensus. Eligibility was delayed for studies reporting outcom es incompletely, p e n d - ing au th o r contact.
- 13. Data Collection After creating and piloting a standardized form, the review - ers (A.L.L., M.R.G., and J.P.B.), working independently and in duplicate an d using a w eb-based program (DistillerSR), ab - stracted details about th e p atien t population, th e in te rv en - tions com pared, and th e outcom es reported. We abstracted details o f th e interventions tested verba- tim from either th e trial report or a cited protocol, lim iting our focus to th e period o f hospitalization until 30 days after dis- charge, and identifying th e “n et intervention” by selecting out activities th a t occurred in th e intervention arm b u t n o t in th e control arm . These activities w ere coded using a taxonom y adapted from H ansen e t al11 (Table 1). We also noted th e n u m - ber o f m eaningfully involved individuals participating in th e 1 0 9 6 J A M A I n t e r n a l M e d ic in e J u ly 2 0 1 4 V o lu m e 174, N u m b e r 7 ja m a in t e r n a lm e d ic in e .c o m Preventing 30-Day Hospital Readmissions Original Investigation Research intervention’s delivery and the number of meaningful inter actions these individuals had with patients. Meaningfully in- volved individuals played a structured and requisite function in the delivery of central aspects of the intervention (eg, a phy- sician who might be contacted only as needed would not be considered meaningfully involved). Similarly, meaningful pa- tient interactions were defined as those that were the pro-
- 14. posed sources of the intervention’s effectiveness (eg, a nurse visiting a patient only to deliver educational materials but not to actually engage in educational activity would not be con- sidered a meaningful interaction). Two team members (A.L.L. and M.R.G.) created summary descriptions of the interven- tions in a standardized format; these were shared with each author to confirm their fidelity to what happened in the trial. After calibrating judgments on a pilot sample, 2 raters fa- miliar with the CuCoM (F.S.M. and K.G.), not involved in data collection and blinded to trial results, evaluated each stan- dardized intervention description on a scale of l (substan- tially decrease) to 4 (no effect) to 7 (substantially increase) to reflect the degree to which the intervention was likely to affect patient workload and patient capacity for self-care. The im- pact on patient capacity was rated with perfect agreement 50% of the time and within l point of difference in 42% of cases (8% differed by 2 points). Because no interventions were rated to decrease patient capacity and all mean ratings fell within the range of 4.0 to 5.5, we elected to dichotomize the variable (threshold of >5 for increasing capacity) for analysis. Work- load was more difficult to assess reliably: perfect agreement and minor disagreement (±1 point) were seen in 29% and 44% of cases, respectively, with 27% of cases differing by 2 or more points. This variable was divided into 3 categories (increase, decrease, no change). For each included trial, we extracted or computed the risk of early readmission for each arm, analyzing patients as ran- domized (intention to treat analysis). We used the number ran- domized as the denominator except when the number of pa- tients discharged was reported and differed from the number randomized. We selected the outcome to extract on the basis of an ad hoc hierarchy of outcomes of interest, with priority given to unplanned readmissions, then to all-cause readmis- sions, and finally to the composite end points of unplanned
- 15. and all-cause readmissions plus out-of-hospital deaths, re- spectively. Outcomes were extracted and analyzed at the lon- gest period of follow-up, up to 30 days from discharge. Exami- nation of trials reporting the effect of interventions on more than 1 of these outcomes revealed that treatment effects were consistent across them (data not shown). Risk o f Bias Two raters (A.L.L. and M.K.) worked independently and in du- plicate to determine the extent to which each trial was at risk of bias using a standardized form based on the Cochrane Col- laboration’s tool.12 The assessment considered the quality of the randomization sequence generation, allocation conceal- ment, blinding of outcome assessors, the potential for miss- ing outcomes (ie, likelihood of missing readmissions to other hospitals), and the proportion of patients lost to follow-up. For missing outcomes, “high risk of bias” was assigned when the Table 1. A c tiv ity -B a s e d C odin g F ra m e w o rk f o r D ischarge In te rv e n tio n s Label A ctivity Observed Discharge planning Simply thinking about and formalizing an approach to prepare for discharge when this did not occur in any way in the control arm Case management Logistical coordination of care and/or resources not specifically focused on self-management and either not occurring in control arm or occurring to lesser degree
- 16. Telephone follow-up Use of a telephone or videophone for provider-initiated communication after discharge that does not occur in the control arm Telemonitoring Use o f remote technology designed fo r the patient to transm it objective measures of health status w ith or w ithout connected subjective assessment Patient education Patient-directed education related to diagnosis or treatm ent rationale but not focused on encouraging self- management and not occurring in control arm Self-management Patient-directed education or coaching directly focused on improving patient's ability to self-manage care needs that does not happen in control arm Medication intervention Medication reconciliation or special education aimed at improving medication understanding or adherence; often conducted by a pharmacist but need not be Home visits Physical visitation by intervention provider to patient's place of residence when this does not happen in control arm
- 17. Follow-up scheduled Scheduling of a follow -up visit prior to discharge when this is not done in the control arm or is done less reliably Patient-centered discharge instructions Some difference in the form at or usability of discharge materials to make them more accessible or relevant compared w ith control Clinician continuity Increased provider presence on both sides o f the hospital- to-hom e transition compared w ith control; may include involvement o f PCP in inpatient care or strategic follow -up w ith inpatient clinician after discharge or "bridging" clinician Timely follow-up Postdischarge follow -up visit or communication with patient when this either does not occur or occurs at a later date in the control arm Timely PCP communication Engagement with PCP in communication about patient status when this either does not occur or occurs at a later date in the control arm Patient hotline Presence of an open line fo r patient-initiated
- 18. communication when this either does not exist in the control arm or is more restricted in availability or usefulness Rehabilitation intervention Patient-directed rehabilitation efforts that are not entirely diagnosis specific but aimed at improving functional status and do not exist in the control arm Streamlining A general streamlining o f services provided, often with dedicated assignment of responsibility, when this does not occur in the control arm Making requisite Increasing the use or quality of services currently available but underutilized compared w ith the situation in the control arm Other Special situations unique to the intervention (eg, caregiver education, peer mentoring) Abbreviation: PCP, prim ary care provider. readmissions data came from internal health system records only. To assess for publication bias, we examined a funnel plot for asymmetry and conducted asymmetry regression accord- ing to Sterne and Egger13 and determined the associated P value. Data Synthesis We used random-effects meta-analyses to estimate pooled risk ratios and 95% confidence intervals for early readmission.14,15
- 19. We tested for heterogeneity of effect on this outcome using the Cochran Q x2 te st16 and estim ated between-trial inconsis- tency not due to chance using the P statistic.17 jamainternalmedicine.com JAM A In te rn a l M edicine July 2014 Volume 174, Number 7 1097 R e s e a rc h O r ig in a l I n v e s t ig a t io n P r e v e n tin g 3 0 - D a y H o s p ita l R e a d m is s io n s To explore th e effects o f p atien t, intervention, and o u t- come characteristics on th e im pact o f m easured intervention effectiveness, we conducted planned subgroup analyses, te st- ing variables 1 at a tim e. Patient characteristics tested were age (m ean >65 years or not), diagnosis (h eart failure or o th er), an d h o sp ital w ard (general medical or other). Intervention characteristics tested included th e num ber o f u n iq u e activities involved in th e in - tervention, th e n um ber o f unique individuals or roles m ean- ingfully involved in its delivery, the minimum num ber of m ean- in g fu l p a tie n t in te ra c tio n s o ccu rrin g w ith in 30 days, th e location o f th e intervention activity (ie, w h eth er it occurred entirely during th e inpatient stay, after discharge, or as a com - bination th a t “bridged” th e transition), w h eth er th e interven- tion was rated to increase or decrease p atien t w orkload, and w h eth er th e intervention w as rated to increase p atien t capac- ity (no intervention was found th a t decreased patient capac-
- 20. ity for self-care). Ad hoc variables tested were year o f publi- c a tio n a n d ty p e o f o u tc o m e r e p o r te d (ie , u n p la n n e d readm issions vs other). In form ed by th e findings o f th e ex p lo rato ry subgroup analyses and our initial hypotheses, we constructed a post hoc m etaregression m odel to te st a variable th a t reflected th e d e- gree to w hich discharge interventions provided com prehen- sive p atien t and caregiver support. This “com prehensive su p p o rt” variable could re tu rn values w ith in a range o f 0 to 4 “p oints” on th e basis o f w h eth er th e intervention (1) was rated to increase p atien t capacity, (2) had at least 5 (75th percentile o f distribution) unique intervention activities, (3) had at least 5 (75th percen tile o f d istrib u tio n ) m eaningful p atien t co n - tacts, and (4) h ad at least 2 (75th percentile o f distribution) in - dividuals involved in its delivery. We created 3 categories for this variable: interventions w ith zero points (category 1), in - terventions w ith 1 or 2 points (category 2), and interventions w ith 3 or 4 points (category 3). To control for changes in s ta n - dard care delivery over tim e, we adjusted on th e basis o f the year o f publication variable. Results Study Selection Our initial database search generated 1128 reports (eFigure 1 in Supplement). Through abstract and title screening, 256 re- p o rts w ere id e n tified for fu ll-tex t review. D uring fu ll-tex t screening (agreement, 89%), 24 were selected for inclusion and
- 21. 39 were set aside for au th o r contact prior to making a d eci- sion. Of 7 potentially eligible studies identified from bibliog- raphies and expert consultation, 2 were included and 1 was set aside for au th o r contact. Of th e 40 trials requiring au th o r con- ta ct for a final eligibility decision, 21 were deem ed eligible. Of th e 48 apparently eligible trials, 1 was found ineligible after the au th o r confirm ed th a t readm ission data were collected only for readm issions related to th e index diagnosis.18 The final sam ple therefore com prised 47 trials from 46 reports.19"64 Of th e 47 eligible trials, 42 con trib u ted data for th e pri- m ary meta-analysis, and 5 (those th a t reported num bers o f re- adm issions rath er th a n th e n um ber o f p atien ts readm itted) w ere analyzed separately.31,45,50,55,61 A com plete list o f ex- cluded full-text studies w ith rationale for exclusion is avail- able in eAppendix 2 (in Supplement). Study Characteristics Table 2 d es crib es th e in c lu d e d tria ls . M any w ere sin g le - center trials taking place in academ ic m edical centers, enroll- ing few patients (eg, 22 trials enrolled <200 patients), and re- porting 30-day readm issions. Most interventions tested took place in b oth the inpatient and o u tp atien t settings. The coded activity analysis is reported in eTable 1 (in Supplement). In gen- eral, interventions included anyw here from 1 to 7 unique ac- tivities. Case m anagement, patient education, hom e visits, and self-m anagem ent support were com m only present in n et ac-
- 22. tivity descriptions (eTable 1 in Supplement). Trial authors re- sponded to confirm ation requests for 34 of th e 47 n et in ter- v e n tio n d e s c r ip tio n s . T h re e a u th o r s r e q u e s te d m in o r modifications and 1 au th o r m ade major modifications to these descriptions. Most studies were at low risk o f bias (eTable 2 and eFig- ure 2 in Supplement). The m ost com m on methodological limi- tation of these trials was th e lack o f a reliable m ethod for deal- ing w ith missing data. Meta-analysis In th e 42 trials reporting readm ission rates, th e overall pooled relative risk (RR) o f readm ission w ithin 30 days w as O.82 (95% Cl, 0.73-0.91; P < .001) (Figure 2). Inconsistency across trials was low (P = 31%). Funnel plot exam ination show ed asym - m etry suggestive o f publication bias in th e context o f smaller studies (eFigure 3 in Supplem ent), and the Egger test was sig- nificant (P = .02). The 5 trials reporting n u m ber o f readm is- sions (rather th an num ber o f patients w ith readm issions) had a pooled relative risk o f readm ission o f 0.93 (95% Cl, 0.72- 1.20; P = 23% ; P = .59). Although this result was consistent with th e risk found in trials reporting readm ission rates (interac- tio n P = .38), we opted n o t to include th ese trials in subgroup analyses. Subgroup analyses failed to find an interaction betw een trial results and p atien t characteristics or outcom e m easured
- 23. (Table 3). A num ber o f intervention characteristics, however, d id in te ra c t w ith m e a su re d effec tiv e n ess. T h ese in c lu d e w hether th e intervention was rated to augm ent patient capac- ity for self-care (RR, 0.68 [95% Cl, 0.53-0.86] w hen it was and RR, 0.88 [95% Cl, O.8O-O.97] w h en it w as n o t; in te ractio n P = .04), w h eth er th e intervention had at least 5 unique, com - p o n en t activities (RR, 0.63 [95% Cl, 0.53-0.76] w h en it did and RR, 0.91 [95% Cl, 0.81-1.01] w h e n it d id n o t; in te ra c tio n P = .001), an d w h eth er th e in terv en tio n had at least 2 in d i- viduals involved in delivery (RR, 0.69 [95% Cl, O.57-O.84] w hen it did and RR, 0.87 [95% Cl, 0.77-0.98] w hen it did not; in ter- action P = .05). Studies testin g in terventions m ore recently were associated w ith reduced effectiveness (RR, 0.89 [95% Cl, O.81-O.97] w hen published in 2002 or later and RR, 0.56 [95% Cl, 0.40-0.79] w h en p u b lis h e d p rio r to 2002; in te ra c tio n P = .01). Other characteristics of th e interventions, such as their rated effect on patient w orkload and th e site o f delivery, had no significant interaction w ith th e intervention effect. 1098 JAMA Internal Medicine J u ly 2 0 1 4 V o lu m e 174, N u m b e r 7 ja m a in t e r n a lm e d ic in e .c o m Preventing 30-Day Hospital Readmissions Original Investigation Research
- 24. Table 2. Study Characteristics3 Source Setting Population Added Intervention Program Baseline Control Activity Outcome Time Reported Patients Discharged, No. Activities6/ People'/ Interactions8 Included in Intervention, No. Capacity' Workload' Location9 Melton e ta l,19 2012 48 US states Commercially insured for 3 acute DRGs
- 25. Risk-prioritized telephone follow-up Nonprioritized telephone follow-up UR, 1 mo 3988 1/1/1 4.0 3.5 OP Marusicetal,20 2013 Academic hospital in Croatia Elderly patients receiving >2 medications for chronic disease Specialized pharmacotherapeutic counseling Standard discharge planning and usual information about drugs from physician UR, 1 mo 160 2/1/1 4.0 3.5 IP
- 26. Altfeldetal,21 2012 US Elderly patients receiving >7 medications with psychosocial need Targeted telephone follow-up program Standard discharge planning without any follow-up contact ACR, 1 mo 906 2/1/1 5.0 2.0 OP Davis eta l,22 2012 Academic center, US Patients with HF with mild cognitive impairment Self-management focused education program
- 27. Standard discharge HF teaching and booklet ACR, 1 mo 125 5/1/2 5.0 3.5 Both Bowles et al,23 2011 Urban community, US Mostly black patients with HF under specific home care agency Telehomecare substitution of traditional home care Clinical pathway for HF and home care ACR, 1 mo 218 1/2/5 4.0 5.5 OP Finn etal,24 201 l h Academic center, US
- 28. General medical patients of academic center; approximately 25% discharged toSNF Embedded nurse practitioner into academic team to improve discharge process Standard discharge planning with follow-up scheduled by resident ACR, 1 mo 646 2/1/1 4.0 2.5 IP Wong e ta l,25 2011 Large general hospital, Hong Kong Elderly general medical population Use of nurse case managers and trained
- 29. volunteers to improve transition through health-social partnership Usual discharge planning for follow-up and support ACR, 1 mo 686 4/3/5 4.5 3.5 Both Leventhal e ta l,26 2011 University hospital, Switzerland Elderly patients with HF Outpatient, interdisciplinary education and support program Standard care with HF consultation, education booklet ACR, 1 mo 34 5/1/4 4.5 4.0 OP Rytter et al,27
- 30. 2010 Single center, Denmark Elderly patients from medical or geriatric ward Use of mandatory home visits to improve follow-up from PCP and district nurses Standard discharge procedures and letters ACR, 1 mo 331 4/2/2 4.0 2.5 OP Koehler etal,28 2009 Academic center, US Elderly general medical patients expected to return to home or assisted living Supplemental care
- 31. bundle that shifted responsibilities from nurses to care coordinators and added follow-up Nursing staff do medication reconciliation, discharge medication teaching, and education; pharmacist review UR, 1 mo 41 6/2/5 4.5 4.0 Both Braun,29 2009 Medical center, Israel General medical patients Use of tight telephone Standard follow-up, especially discharge to improve adherence planning and summary ACR, 1 mo 400 1/1/2 4.5 3.0 OP Courtney eta l,30 2009
- 32. Tertiary center, Australia Elderly general medical patients at high risk Individualized, exercise-based care plan for elderly Routine discharge and rehabilitation advice, planning UR, 1 mo 128 6/2/5 5.0 5.0 Both Jack e ta l,31 2009 Academic, urban, safety net center, US General medical patients; 51% black Standardized discharge package to minimize failures using discharge planners and
- 33. pharmacists Similar to intervention but uncoordinated ACRE, 1 mo 738 6/2/3 5.0 2.5 Both (continued) jamainternalmedidne.com JAMA Internal Medicine July 2014 Volume 174, Number 7 1099 Research Original Investigation Preventing 30-Day Hospital Readmissions Table 2. Study Characteristics3 (continued) Activities3/ People1/ Interactions3 Source Setting Population Added Intervention Program Baseline Control Activity Outcome Time Reported
- 34. Patients Discharged, No. Included in Intervention, No. Capacity' Workloadf Location9 Wakefield e ta l,32 2008 VA medical center, Iowa, US Men w ith HF; mean age, 69 y Telehealth-facilitated Usual discharge postdischarge support teaching and program follow -up ACR, 1 mo 148 2 /1 /5 5.0 5.0 OP Balaban e ta l,33 2008 Small Culturally and community linguistically teaching diverse general hospital, US medical or surgical patients
- 35. Program to promptly reconnect patients to medical home through discharge form Standard discharge planning and instruction ACR, 1 mo 96 3 /2 /2 5.0 2.5 Both Wong e ta l,34 2 0 08 3 Regional hospitals, Hong Kong Elderly patients readmitted to department of medicine Preventive, postdischarge home visits fo r high-risk patients Standard discharge planning and instruction UR, 1 mo 354 2 /1 /2 4.0 4.0 Both
- 36. Coleman e ta l,35 2006 Single center, US Elderly medical patients who were in capitated delivery system; approximately 20% discharged to SNF Use o f transition coaches and personal health record to equip patients and caregivers to be more active in care Not well reported UR, 1 mo 750 5 /1 /5 4.5 5.0 Both Linne et al,3e 2006 Multiple community hospitals, Sweden
- 37. Patients w ith HF; discharge disposition not reported Use computer-based education session in discharge process Standard HF education and materials ACR, 1 mo 230 2 /0 /0 4.0 4.5 Both Casas et al,37 2006 2 Tertiary centers, 1 in Spain and l i n Belgium Elderly patients w ith COPD Integrated care plan Standard to generate synergy discharge and avoid redundancy protocol w ithout between inpatient and support o f nurse outpatient care teams or call center fo r patients with COPD ACR, 1 mo 155 7 /3 /5 5.0 4.5 Both
- 38. Riegel et al,38 2006 2 Mexican Community Americans with hospitals, HF who were southern old, ill, and California, poorly US acculturated Telephone case management program to improve discharge transition in Mexican Americans Nonstandardized, ACR, 1 mo HF education often in English 135 5 /1 /1 5.5 3.0 OP Koelling e ta l,39 2 005 University Selected hospital, US patients w ith HF; mean age, 65 y Single predischarge education session Standard discharge
- 39. information and education, booklet ACR, 1 mo 223 2 /1 /1 4.5 4.5 IP Mejhert e ta l,40 2 0 04 University hospital, Sweden Elderly patients w ith HF Nurse-driven, protocol-based outpatient management program Standard discharge care; usual follow -up ACR+D, 1 mo 196 3 /2 /1 5.0 4.5 OP Kwok et al,41 2004 2 Acute hospitals, Hong Kong
- 40. Elderly patients w ith chronic lung disease at high risk Community nurse-supported program based on weekly home visits Standard follow -up with home visits as needed UR, lm o 157 4 /1 /5 5.5 4.5 Both Doughty et a l 42 2002" Single Patients w ith HF; center, New dispositions not Zealand reported Outpatient, integrated management program for HF Usual care under PCP ACR, 1 mo 197 6 /3 /1 4.5 5.0 OP
- 41. Jaarsma e ta l,43 1999 University Elderly patients Hospital, w ith HF; mean Netherlands age, 73 y Nurse-led education and support program w ith follow -up home visit Usual care; no structured education, follow -up call, or home visit ACR, 1 mo 179 3 /1 /3 4.0 3.5 Both Naylor et al,44 1999 2 Urban academic hospitals, US Elderly medical and surgical patients; 45% black Advanced practice nurse-directed program that stressed
- 42. continuity, home and telephone follow -up Routine discharge planning and home care ACR, 1 mo 363 5 /1 /4 5.5 2.5 Both Stewart et al,45 1998 Tertiary referral center, Australia General medical and surgical patients; 83% considered high Risk-targeted, home- based intervention by nurse and pharmacist Discharge planning with follow -up w ithin 2 wk UR+DE, 1 mo
- 43. 762 5 /2 /3 5.0 2.5 Both risk (continued) 1100 JAMA Internal Medicine July 2014 Volume 174, Number 7 jamainternalmedicine.com Preventing 30-Day Hospital Readmissions Original Investigation Research Table 2. Study Characteristics3 (continued) Activities11/ People11/ Interactions11 Outcome Patients Included in Added Intervention Baseline Control Time Discharged, Intervention, Source Setting Population Program Activity Reported No. No. Capacity' Workload1 Location9 Dunn et al,46 1995 Geriatric hospital, England Geriatric ward patients; mean age, 83 y
- 44. Single home visit from Usual discharge public health nurse process ACR, 1 mo 204 2 /1 /1 4.5 3.0 OP Rich et al,47 1995 Single academic center, US High-risk, elderly patients w ith HF Nurse-directed, m ultidisciplinary intervention w ith home visit follow -up Conventional care by PCP ACR, 1 mo 274 6 /4 /5 5.5 2.0 Both Naylor et al,48 1994 Single university hospital, US Elderly patients w ith or w ithout
- 45. caregiver for medical cardiac diagnosis Individualized, comprehensive program directed by clinical nurse specialists, including home follow -up Robust but not individualized routine discharge plan ACR, 2 wk 142 5 /1 /4 4.5 2.0 Both Naylor et at,48 1994 Single university hospital, US Elderly patients w ith or w ithout caregiver for surgical cardiac diagnosis Individualized, comprehensive program directed by clinical nurse specialists, including
- 46. home follow -up Robust but not individualized routine discharge plan ACR, 2 wk 134 5 /1 /4 4.5 2.0 Both Naylor et al,49 1990 Urban medical center, US Elderly general medical or surgical patients Comprehensive, individualized discharge planning protocol w ith home follow -up directed by nurse specialists Nurse-directed routine discharge planning ACR, 2 wk 40 4 /1 /4 4.0 3.0 Both Kulshreshtha e ta l,50 2010
- 47. Urban Patients w ith HF; teaching could enter hospital, US study up to 2 weeks after discharge Remote monitoring Not well follow -up program fo r described ambulatory patients ACRE, 1 mo 150 2 /1 /5 5.5 5.5 OP Graumlich e ta l,512009h Tertiary General medical teaching patients at high hospital, US risk of readmission Discharge software to improve communication and address deficiencies Usual care with handwritten discharge forms ACR, 1 mo 631 3 /1 /0 4.0 3.0 IP Atienza et al,52 2004
- 48. 3 Tertiary university hospitals, Spain Patients w ith HF; mean age, 68 y Hospital discharge and outpatient disease management program Variable and nonstructured; PCP follow -up ACR, 1 mo 338 5 /2 /2 4.5 4.0 Both R ie g e le ta l,53 2004 2 Hospitals in suburban Southwest, US Patients w ith HF in integrated health system; mean age, 73 y Use of peer mentors to improve self-care in recently discharged
- 49. patients Inpatient HF education; support groups available ACR, 1 mo 88 1 /1 /2 4.5 3.0 OP Stowasser e ta l,54 2 0 02 2 Large hospitals, Australia General medical and surgical patients Medication liaison service to improve communication of medication-related issues through discharge process Routine care and pharmacist medication review, discharge planning UR, 1 mo 240 3 /1 /0 4.0 3.0 IP
- 50. Li e ta l,55 2012 Academic Elderly patients center, New and their fam ily York, US caregivers Training of fam ily caregivers to prepare fo r anticipated postdischarge role Routine care w ith practical information given to caregivers ACRE, 2 wk 407 1 /0 /0 4.5 3.5 IP Shyu e ta l,56 2005 Large, single center, Taiwan Elderly patients w ith hip fracture Interdisciplinary program of geriatric consultation, rehab, and discharge planning service Routine care and inpatient
- 51. physical therapy w ithout home visits ACR, 1 mo 137 4 /3 /5 5.5 3.5 Both Angermann e ta l,57 2012 9 Centers, Germany Patients w ith HF; mean age, 69 y Nurse-coordinated disease management program that emphasized a "call and care center" Standard discharge planning and follow -up ACR, 1 mo 715 4 /1 /5 4.5 4.5 Both Naylor e ta l,58 2004 5 Academic and Elderly patients with HF; 36%
- 52. Advanced practice nurse-directed care Standard, site- specific HF ACR+D, 1 mo 239 6 /1 /5 5.0 3.0 Both community black program with discharge hospitals, emphasis on comorbid planning and US and chronic condition follow -up management; included home follow -up (continued) jamainternalmedicine.com JAMA Internal Medicine July 2014 Volume 174, Number 7 1101 R e s e a rc h O r ig in a l I n v e s t ig a t io n P r e v e n tin g 3 0 - D a y H o s p ita l R e a d m is s io n s T a b le 2 . S t u d y C h a r a c t e r i s t i c s 3 ( c o n t i n u e d ) S o u rce S e ttin g P o p u la tio n A d d e d I n te r v e n tio n P ro g ra m
- 53. B a s e lin e C o n tr o l A c t i v i t y O u tc o m e T im e R e p o rte d P a tie n ts D is c h a rg e d , N o. A c t iv it ie s 6/ P e o p le 1/ In te r a c tio n s 6 In c lu d e d in I n te r v e n tio n , N o. C a p a c ity " W o r k lo a d ' L o c a tio n 9 S tro m b e rg e t a l , 59 2 0 0 3 1 U n iv e r s ity E ld e rly p a tie n ts a n d 2 w it h HF c o u n ty h o s p ita ls , S w e d e n R e q u is ite f o l lo w - u p in s p e c ia liz e d , p r o t o c o l- d r iv e n , n u r s e -le d HF c lin ic
- 54. C o n v e n tio n a l p r im a r y ca re f o llo w - u p ACR+D, 1 m o 1 0 6 5 / 1 / 1 5 .0 3 .5 OP H ansen e t a l , 60 1 9 9 5 U n iv e r s ity H ig h ly s e le c te d H o m e v is it f o llo w - u p h o s p ita l, p a tie n ts f r o m p ro g ra m f o r h ig h ly D e n m a rk s u b a c u te g e r ia tr ic ta r g e te d e ld e r ly w a rd n e e d in g p o p u la tio n h o m e r e h a b ilita tio n and m e d ic a l a nd s o c ia l s u p p o r t D is c h a rg e s u m m a ry s e n t a n d s ta n d a rd s u p p o r t a rra n g e d ACR, 1 m o 1 9 3 4 / 2 / 2 5 .0 3 .5 OP M a slo ve e t a t,61 2 0 0 9 h S in g le G e n e ra l m e d ic a l a c a d e m ic p a tie n ts ;
- 55. c e n te r, a p p r o x im a te ly Canada 8 0 % d is c h a rg e d h o m e D e v e lo p m e n t o f m o re u s e fu l a nd s ta n d a rd iz e d d is c h a rg e s u m m a ry S ta n d a rd , a tte n d in g p h y s ic ia n - g e n e ra te d d is c h a rg e s u m m a rie s a nd p la n n in g ACRE, 1 m o 2 0 9 2 / 1 / 0 4 .0 3 .5 IP F o rs te r e t a l , 62 2 0 0 5 2 C am p u se s G e n e ra l m e d ic a l o f a p a tie n ts ; m e an te a c h in g a g e , 6 6 y h o s p ita l, Canada In te g r a tio n o f d e d ic a te d c lin ic a l n u rs e s p e c ia lis t in to c a re te a m t o f a c ilit a t e d is c h a rg e p la n n in g p roce ss
- 56. R e g u la r d is c h a rg e c a re p la n n in g ACR+D, 1 m o 3 6 1 3 / 1 / 1 4 .0 3 .0 B o th D udas e t a l,63 2 0 0 1 S in g le G e n e ra l m e d ic a l a c a d e m ic s e rv ic e p a tie n ts c e n te r, US P h a rm a c y s e rv ic e f o l lo w - u p c a ll R e g u la r p h a rm a c y - f a c ilita te d d is c h a rg e p roce ss ACR, 1 m o 2 2 1 2 / 1 / 1 4 .0 3 .0 OP P a rry e t a l , 64 2 0 0 9 2 F e e - fo r - s e r v ic e Use o f t r a n s it io n C o m m u n ity M e d ic a re p a tie n ts co a c h e s a nd p e rs o n a l h o s p ita ls , in s in g le h e a lth h e a lth r e c o rd t o e q u ip US s y s te m ; in c lu s io n p a tie n ts and
- 57. c r ite r ia d e s ire d t o c a re g iv e rs t o a s s e rt c a tc h p a tie n ts m o re a c tiv e r o le in d is c h a r g in g t o c a re tr a n s it io n S N F - d id n o t r e p o r t d is p o s itio n s N o t w e ll re p o r te d UR, 1 m o 9 8 5 / 1 / 5 5 .0 2 .5 B o th A b b r e v ia tio n s : AC R , a ll-c a u s e r e a d m is s io n r a te ; A C R +D , a ll-c a u s e r e a d m is s io n c N u m b e r o f in d iv id u a ls m e a n in g f u lly in v o lv e d in d e liv e r y o f t h e in t e r v e n tio n , a n d o u t - o f- h o s p ita l d e a t h ra te ; A C R E , a ll-c a u s e r e a d m is s io n e v e n t c o u n t; B o th , a |y|jn j m u m n u m b e r o f m e a n in g f u l h u m a n in t e r a c t io n s in i n t e r v e n t io n d e liv e ry . a c t i v it y o c c u r r e d in b o t h in p a t ie n t a n d o u t p a t ie n t e n v ir o n m e n ts ; C O P D , c h r o n ic „ . , ,, . . , ,. ,. . . . . . . . . e R a te d lik e lih o o d o f i n t e r v e n t io n t o a f f e c t p a t ie n t c a p a c ity f o r s e lf- c a r e o n a o b s t r u c t iv e p u lm o n a r y d is e a s e ; DRG , d ia g n o s is - r e la te d g r o u p ; HF, h e a r t f a ilu r e ; , , , , . „ . , . ,, .. .. . . . . . . . . „ .. .. ,. s c a l e o f l ( s u b s t a n t i a l ly d e c r e a s e ) t o 4 ( n o e f f e c t ) t o 7 ( s u b s t a n t i a l l y in c r e a s e ) . IP, a ll a c t i v it y o c c u r r e d in i n p a t ie n t e n v ir o n
- 58. m e n t ; OP, a ll a c t iv it y o c c u r r e d in o u t p a t ie n t e n v ir o n m e n t ; SNF, s k ille d n u r s in g f a c ility ; U R, u n p la n n e d f R a te d lik e lih o o d o f in t e r v e n t io n t o im p o s e w o r k o r b u r d e n o n p a t ie n t o n a r e a d m is s io n ra te ; U R + D E , u n p la n n e d r e a d m is s io n a n d o u t - o f- h o s p ita l d e a th s s c a le o f 1 ( s u b s t a n t ia lly d e c re a s e ) t o 4 ( n o e f f e c t ) t o 7 ( s u b s t a n t ia lly in c re a s e ), e v e n t c o u n t ; US, U n ite d S ta te s ; V A . V e te r a n s A ffa ir s . s S e ttin g ( in p a tie n t , o u t p a t ie n t , o r b o t h ) w h e r e in t e r v e n t io n a c t i v it y o c c u r r e d . 3 I n t e r v e n t io n a n d b a s e lin e /c o n tr o l a c tiv it ie s w e r e s y s te m a tic a lly c o d e d in h C lu s te r - r a n d o m iz e d s tu d y . g r e a t e r d e ta il th a n c a n b e e x p r e s s e d in t h is t a b le (s e e e T a b le 1 in S u p p le m e n t) . b N u m b e r o f a c t iv it ie s in t h e i n t e r v e n t io n as e v a lu a te d b y c o d in g s tr a te g y f r o m T a b l e ! P o s t H o c M e t a r e g r e s s io n A n a ly s is D e sp ite p o te n tia l c o lin e a rity o f th e c o n tr ib u tin g v a ria b le s , m e ta re g re ssio n sh o w e d a sig n ifican t a n d in c re m e n ta l effect o f “c o m p r e h e n s i v e s u p p o r t ” o n r e d u c i n g r e a d m is s io n s (Table 4). C ategory 3 com prised 7 in terv en tio n
- 59. s.28,3037'47'56,58,64 C om pared w ith cate g o ry 1 in te rv e n tio n s, th e s e w ere a sso c i- a te d w ith a relativ e risk o f re a d m iss io n o f 0.63 (95% Cl, 0.43- 0 .91; P = .02). C ategory 3 in te rv e n tio n s u s e d a c o n siste n t an d c o m p le x s tra te g y th a t e m p h a s iz e d th e a s s e s s m e n t a n d a d - d re ssin g o f facto rs re la te d to p a tie n t c o n te x t a n d ca p a c ity for self-care (including th e im p act o f com orbidities, fu nctional s ta - tu s , caregiver capabilities, socioeconom ic factors, p o te n tia l for self-m a n a g e m e n t, a n d p a tie n t a n d caregiver goals for care). T h ese in te rv e n tio n s co o rd in a te d care across th e in p a tie n t-to - o u tp a tie n t tr a n s itio n a n d in v o lv ed m u ltip le p a tie n t in te ra c - tio n s; all b u t l 28 inv o lv ed p a tie n t h o m e visits. Discussion O u r F in d in g s T he b o d y o f ra n d o m iz e d trial ev id en c e show s a c o n siste n t and b en eficial effect o f te s te d in te rv e n tio n s o n th e risk o f 30-day read m issio n s. E x p lo rato ry su b g ro u p a n aly ses su g g est th a t ef- 1 1 0 2 J A M A I n t e r n a l M e d ic in e J u ly 2 0 1 4 V
- 60. o lu m e 174, N u m b e r 7 ja m a in t e r n a lm e d ic in e .c o m P r e v e n t in g 3 0 - D a y H o s p ita l R e a d m is s io n s O r ig in a l I n v e s t ig a t io n Research Figure 2. Results o f Prim ary Meta-analysis Study RR (95% Cl) Naylor e ta l,49 1990 0.33 (0 .0 4 -2 .9 4 ) Naylor e ta l,48 1994 0 .2 7 (0 .0 8 -0 .9 1 ) Naylor et a l 48 1994 0.69 (0 .2 3 -2 .0 8 ) Dunn et al,46 1995 1.13 (0 .6 1 -2 .08 ) Rich et a l,47 1995 0.69 (0 .4 2 -1 .1 3 ) Hansen e ta l,60 1995 0 .3 0 (0 .1 6 -0 .5 7 ) Jaarsma e ta l,43 1999 0.89 (0 .4 3 -1 .8 5 ) Naylor e ta l,44 1999 0 .3 5 (0 .1 9 -0 .6 5 ) Dudas e ta l,63 2 001 0.61 (0 .3 6 -1 .0 5 ) Doughty et al,42 2002 1 .1 4 (0 .6 4 -2 .0 4 ) Stowasser et al,54 2002 0 .8 4 (0 .3 7 -1 .9 3 ) Stromberg et a l,59 2003 0 .6 1 (0 .3 5 -1 .0 9 ) M ejhert et al,40 2004 0.91 (0 .4 5 -1 .8 3 ) Kwok et al,41 2004 1 .1 8 (0 .8 0 -1 .7 4 ) Atienza et a l,52 2 0 04 0.57 (0 .3 1 -1 .06 ) Riegel and Carlson,53 2004 1.53 (0 .5 4 -4 .31 ) Naylor et a l,58 2004 0.51 (0 .3 0 -0 .88 ) Koelling et a l,39 2 0 05 0 .7 0 (0 .4 3 -1 .1 5 ) Shyu e ta l,56 2005 0 .6 1 (0 .1 5 -2 .4 5 ) Forster e ta l,62 2 0 05 1.35 (0 .8 4 -2 .16 )
- 61. Coleman e ta l,35 2006 0.70 (0 .4 5 -1 .07 ) Linne and Liedholm ,36 2006 1.05 (0 .6 3 -1 .77 ) Casas et a l,37 2006 0 .5 9 (0 .2 4 -1 .4 6 ) Riegel et a l,38 2 0 06 0 .7 9 (0 .3 8 -1 .6 3 ) Balaban e t a l, 33 2008 1 .0 4 (0 .2 8 -3 .9 3 ) Wong et a l,34 2008 0 .9 8 (0 .7 3 -1 .3 1 ) Wakefield e ta l,32 2008 0.66 (0 .3 0 -1 .4 6 ) Koehler et a l,28 2009 0.42 (0 .0 9 -1 .9 2 ) Braun et a l,29 2009 0.92 (0 .4 1 -2 .0 3 ) Courtney e t a l, 30 2009 0 .3 0 (0 .0 9 -1 .0 4 ) Graumlich e ta l,51 2009 0.97 (0 .6 6 -1 .45 ) Parry et a l,64 2 0 09 0.44 (0 .1 5 -1 .3 5 ) R y tte r e ta l,27 2010 0 .7 1 (0 .4 5 -1 .1 3 ) Bowles et a l,23 2011 0.83 (0 .4 6 -1 .49 ) Finn e ta l,24 2011 1 .1 6 (0 .8 5 -1 .6 0 ) Wong e ta l,25 2011 0.78 (0 .5 3 -1 .16 ) Leventhal e ta l,26 2011 0 .5 6 (0 .0 6 -5 .6 3 ) Melton e ta l,19 2012 0 .7 8 (0 .6 2 -0 .9 9 ) A ltfeld et a l,212012 1.05 (0 .7 7 -1 .43 ) Davis et a l,22 2012 1.15 (0 .5 8 -2 .28 ) Angermann et al,57 2012 1.09 (0 .7 1 -1 .66 ) Marusic e ta l,20 2013 1 .2 0 (0 .3 8 -3 .7 7 ) Overall effect (P<.001) 0.82 (0 .7 3 -0 .9 1 ) Heterogeneity: l 2 = 31%; P = .03 Favors Intervention Favors Control j
- 62. 0.1 1.0 RR (95% Cl) Weight, % 0.24 0.71 0.88 2.30 3.08 2.14 1.75 2.28 2.77 2.49 1.44 2.57 1.88 4.17 2.31 0.97
- 64. 5.06 4.16 0.22 6.30 5.18 1.95 3.77 0.81 100.00 T T 1 10 S ize o f t h e d a ta m a r k e r c o r r e s p o n d s t o t h e r e la tiv e w e ig h t a s s ig n e d in t h e p o o le d a n a ly s is u s in g r a n d o m - e ffe c ts m o d e ls . RR in d ic a te s r e la tiv e ris k . fective interventions are more complex and seek to enhance patient capacity to reliably access and enact postdischarge care. In addition, interventions tested more recently are, in gen- eral, less efficacious when compared with controls. Our findings are consistent with the CuCoM in their sug- gestion that providing comprehensive and context-sensitive
- 65. support to patients reduces the risk of early hospital readmis- sion; however, we could not identify an effect of rated inter- vention workload on this risk. Limitations and Strengths of This Review Many studies in this review were conducted in single, aca- demic centers; this raises questions about applicability. Also, the scales that we used to evaluate intervention effects on pa- tient workload and capacity relied on global judgments (rather than criterion-based judgments) and are original to this work. To our knowledge, no validated scale exists to assess the po- tential of an intervention to impose patient workload or treat- ment burden and/or affect a patient’s capacity for self-care. Al- though our raters were consistent in their assessm ents of interventions’ effect on patient capacity, their judgment of im pact on patient workload was less reliable. Particularly, raters believed that some burdensome interventions could be ben- eficial if the patient had the capacity and resources to access and enact the care. Because the experience of treatment bur- den is not constant between patients, an ideal analysis of its ja m a in t e r n a lm e d ic in e .c o m JAMA Internal Medicine J u ly 2 0 1 4 V o lu m e 174, N u m b e r 7 1103 R e s e a rc h O r ig in a l I n v e s t ig a t io n P r e v e n tin g 3 0 - D a y H o s p ita l R e a d m is s io n s T a b le 3 . S u b g r o u p A n a ly s e s S tu d y S u b g ro u p C h a r a c te r is tic (N o . o f S tu d ie s in S u b g r o u p ) 3
- 66. R e a d m is s io n , R e la tiv e R isk ( 9 5 % C l) P V a lu e f o r In te r a c tio nS u b g ro u p C o m p a ris o n G ro u p P a tie n t c h a r a c te r is tic s HF ( 1 6 ) 0 .8 2 ( 0 . 7 0 - 0 . 9 5 ) 0 . 8 0 ( 0 . 6 9 - 0 . 9 3 ) .8 3 A g e > 6 5 y ( 3 6 ) 0 .7 9 ( 0 . 6 9 - 0 . 9 0 ) 0 .9 1 ( 0 . 7 4 - 1 . 1 0 ) .2 4 F ro m g e n e r a l m e d ic a l w a r d ( 1 8 ) 0 . 8 0 ( 0 . 6 7 - 0 . 9 5 ) 0 . 8 3 ( 0 . 7 2 - 0 . 9 5 ) .7 9 I n te r v e n tio n c h a r a c te r is tic s R a te d t o in c re a s e p a t ie n t c a p a c ity ( 1 6 ) 0 . 6 8 ( 0 . 5 3 - 0 . 8 6 ) 0 . 8 8 ( 0 . 8 0 - 0 . 9 7 ) .0 4 R a te d t o in c re a s e p a t ie n t w o r k lo a d ( 5 ) b 0 .7 7 ( 0 . 5 7 - 1 . 0 3 ) 0 .8 2 ( 0 . 7 1 - 0 . 9 6 ) .6 8 R a te d t o d e c re a s e p a t ie n t w o r k lo a d ( 1 9 ) b 0 .8 1 ( 0 . 6 7 - 0 . 9 8 ) 0 .8 2 ( 0 . 7 1 - 0 . 9 6 ) .9 0 A b b r e v ia tio n : HF, h e a r t fa ilu r e . D e liv e re d b y 2 o r m o re in d iv id u a ls ( 1 3 ) c 0 . 6 9 ( 0 . 5 7 - 0 . 8 4 ) 0 .8 7 ( 0 . 7 7 - 0 . 9 8 ) .0 5 a C o m p a r e d w it h t h e r e m a in d e r o f a n a ly z e d s tu d ie s ( ie , 4 2 - N ) u n le s s o th e r w is e n o te d . in v o lv e d > 5 m e a n in g f u l p a t ie n t in t e r a c t io n s ( 1 3 ) c
- 67. 0 . 7 7 ( 0 . 6 4 - 0 . 9 2 ) 0 . 8 4 ( 0 . 7 3 - 0 . 9 6 ) .4 3 C o m p ris e d > 5 u n iq u e a c t iv it ie s ( 1 6 ) c 0 .6 3 ( 0 . 5 3 - 0 . 7 6 ) 0 .9 1 ( 0 . 8 1 - 1 . 0 1 ) .0 0 1 b C o m p a r e d w it h " n o c h a n g e ” ( n = 1 8). c C u t o f fs c h o s e n b e c a u s e t h e y H ad b o th a n in p a t ie n t a n d o u t p a t ie n t c o m p o n e n t ( 2 2 ) 0 .7 8 ( 0 . 6 5 - 0 . 9 2 ) 0 . 8 4 ( 0 . 7 4 - 0 . 9 7 ) .4 6 S tu d y p u b lis h e d 2 0 0 2 o r la t e r ( 3 3 ) d 0 .8 9 ( 0 . 8 1 - 0 . 9 7 ) 0 . 5 6 ( 0 . 4 0 - 0 . 7 9 ) .0 1 r e p r e s e n te d t h e 7 5 t h p e r c e n tile o f O u tc o m e c h a r a c te r is tic s O u tc o m e m e a s u re d w a s u n p la n n e d r e a d m is s io n s ( 9 ) 0 . 8 4 ( 0 . 6 9 - 1 . 0 2 ) 0 . 8 0 ( 0 . 7 0 - 0 . 9 1 ) .7 0 r e p r e s e n te d t h e m i d - p o in t o f s tu d y e lig ib ilit y f o r t h is r e v ie w . T a b le 4 . E f f e c t s o f C o m p r e h e n s i v e S u p p o r t in M e t a r e g r e s s i o n A n a ly s i s S tu d y C h a r a c te r is tic S tu d ie s , N o. R e a d m is s io n , R e la tiv e R isk ( 9 5 % C l)a P V a lu e C o m p re h e n s iv e s u p p o r t c a te g o r y 5
- 68. 1 ( 0 p o in ts ) 1 5 1 [R e fe r e n c e ] 2 (1 o r 2 p o in ts ) 2 0 0 .8 2 ( 0 . 6 6 - 1 . 0 2 ) .0 7 3 (3 o r 4 p o in ts ) 7 0 .6 3 ( 0 . 4 3 - 0 . 9 1 ) .0 2 P u b lic a tio n in 2 0 0 2 o r a fte r 3 3 1 .4 7 ( 1 . 1 0 - 1 . 9 6 ) .0 1 a T h is r e p r e s e n ts t h e a d ju s te d e f f e c t o f e a c h c h a r a c te r is tic o n e a r ly r e a d m is s io n t h a t (1) w e r e r a te d t o in c re a s e p a t ie n t c a p a c ity , ( 2 ) h a d > 5 u n iq u e in t e r v e n t io n in m e ta r e g r e s s io n . a c tiv it ie s , (3 ) h a d s 5 m e a n in g fu l p a t ie n t in t e r a c t io n s , a n d ( 4 ) h a d > 2 b T h e c o m p r e h e n s iv e s u p p o r t v a r ia b le r e tu r n e d 1 p o in t e a c h f o r in t e r v e n tio n s in d iv id u a ls in v o lv e d in its d e liv e ry . effects would be based on patient-reported assessm ents o f in - te rv e n tio n w o rk lo ad . In d e e d , m an y eligible p a tie n ts d e - clined en ro llm en t in to som e s tu d ie s , 2 3 , 2 8 ,4 4 , 5 0 ,5 3 o ften b e - cause th ey did not w ish to take on th e perceived burden o f the intervention; evaluating th e effect o f intervention-im posed w orkload in such sam ples is o f lim ited applicability. In gen- eral, th e se assessm en ts should be regarded as h y p o th e sis- generating and th e inferences m ade on th e basis o f subgroup analyses m u st be view ed as tentative (given th e potential for chance findings from testing multiple hypotheses and the pos- sibility th a t some variables are correlated). Finally, despite ro
- 69. - b u st efforts to obtain unpublished data, there was evidence o f publication bias. The overall effect o f this on our findings is n o t known. This review also has m any strengths. First, it provides, to our knowledge, th e largest a n d m ost com prehensive assess- m ent o f discharge interventions and their effect on 30-day re- adm issions, including 47 random ized trials at low risk o f bias. This is a stronger and less heterogeneous body o f evidence than previously assem bled , 11,65 and it includes u npublished data from 18 trials. Our study used an activity-based coding m ethod designed to en su re appropriate characterization o f each in - te rv en tio n and th e n et difference in activity betw een in te r- v en tio n and control arm s. This m e th o d co n trib u tes to th e field an d can be applied to fu tu re assessm en ts o f com plex interventions. To our knowledge, this is also th e first use of th e CuCoM5 to analyze th e im pact o f health care delivery in - terv en tio n s on p atien ts as an explanation for th e ir relative efficacy. C o m p a r is o n W i t h O t h e r S t u d ie s We identified 31 more random ized clinical trials th a n were accu m u lated in th e m o st recen t review o f discharge in te r- ven tio n effects on 30-day readm ission ra te s , 11 an d w e p ro - vide th e first m eta-analysis on th is topic. Although previous stu d ies an d review s have suggested th a t “b u n d le d ” in te r- v en tio n s are o f g rea ter v a lu e , 11,65 th is m e ta-an a ly
- 70. sis p ro - vides objective support for this claim. In addition, our study ad d s to an d en h an ces th e body o f evidence rela ted to th e im portance o f p atien t contextual factors in affecting health outcom es. 6 5 Im p lic a t io n s f o r P o lic y a n d P r a c t ic e In this analysis, interventions th a t used a com plex and su p - portive strategy to assess and address contextual issues and lim itations in patient capacity w ere m ost effective at reduc- 1 1 0 4 J A M A I n t e r n a l M e d ic in e J u ly 2 0 1 4 V o lu m e 174, N u m b e r 7 ja m a in t e r n a lm e d ic in e .c o m Preventing 30-Day Hospital Readmissions Original Investigation Research ing early hospital readm issions. Many o f these contacted th e p atien t frequently, used hom e visits, and reported cost sav- ings. This inform ation can be used to guide the design and te st- ing o f fu tu re interventions. The CuCoM may also have value in helping to conceptualize th e effects o f health care in terv en - tions across diverse patient contexts, b u t we w ere unable to characterize a co n sisten t effect o f rated in terv en tio n w ork- load on outcom es. Finally, we found th a t more recently tested interventions were less effective. We hypothesize th at this may rep rese n t (l) a general im provem ent over tim e in th e s ta n -
- 71. dard o f care th a t was no t fully appreciated in control descrip- tions, (2) an increased effort over tim e to test sim pler and less comprehensive interventions, (3) a higher likelihood over tim e o f more diverse interventions to m easure and report 30-day readm ission rates (eg, including th o se less focused on red u c- ing early readm issions), and/or (4) a general shift away from interventions stressing hum an interaction tow ard those more high tech in nature. Additional stu d y is need ed to d eterm ine th e im plications o f this finding. Conclusions Our results suggest th a t m ost interventions tested are effec- tiv e in red u cin g th e risk o f early read m issio n s. Some fe a - tures, however, m ay enhance th e effect o f these programs. In particular, we found value in interventions th a t supported p a- tie n ts’ capacity for self-care in their transition from hospital to hom e. F uture work in ten d ed to improve th e effectiveness o f health care delivery may benefit from consideration o f the dem ands th a t h ealth care interventions place on recently dis- charged patients and th eir caregivers and th e extent to w hich these dem ands are offset by comprehensive support for im ple- m entation. ARTICLE INFORMATION Accepted for Publication: March 8,2014. Published Online: May 12,2014. doi:10.1001/jamainternmed.2014.1608. Author Affiliations: Knowledge and Evaluation Research Unit, Mayo Clinic, Rochester, Minnesota
- 72. (Leppin, Gionfriddo, Kessler, Brito, Wang, Boehmer, Ting, Murad, M ontori); Mayo Graduate School. Mayo Clinic, Rochester, Minnesota (Gionfriddo); Departm ent o f Medicine, Mayo Clinic, Rochester, Minnesota (Kessler, Brito, M ontori); Mayo Clinic Center fo r the Science o f Healthcare Delivery, Mayo Clinic, Rochester, Minnesota (Brito, Wang, Murad, M ontori); General Practice and Primary Care, Institute o f Health and Wellbeing, University o f Glasgow, Glasgow, Scotland, United Kingdom (Mair, Gallacher); Mayo Clinic Libraries, Mayo Clinic, Rochester, Minnesota (Erwin); medical student at St Louis University School o f Medicine, St Louis, Missouri (Sylvester); graduate student at University o f Minnesota School o f Public Health, Minneapolis (Boehmer); Division o f Health Policy and Management, School o f Public Health, University o f Minnesota. Minneapolis (Shippee). Author Contributions: Drs Leppin and M ontori had full access to all o f th e data in the study and take responsibility fo r th e integrity o f the data and the accuracy o f th e data analysis. Study concept and design: Leppin, Gionfriddo, Mair, Gallacher, Erwin, Murad, Shippee, M ontori. Acquisition, analysis, o r interpretation o f data: Leppin, Gionfriddo, Kessler, Brito, Mair, Gallacher, Wang, Sylvester, Boehmer, Ting, Murad, M ontori. Drafting o f the manuscript: Leppin, Mair, Gallacher, Boehmer, Murad, Montori. Critical revision o f the manuscript fo r im portant intellectual content: All authors. Statistical analysis: Wang, Murad, Montori. Administrative, technical, or m aterial support: Leppin, Kessler, Brito, Mair, Gallacher, Erwin, Sylvester, Boehmer, M ontori.
- 73. Study supervision: Leppin, M ontori. Conflict o f Interest Disclosures: None reported. Funding/Support: This publication was made possible by Clinical and Translational Science Award grant UL1TR000135 from th e National Center for Advancing Translational Sciences, a com ponent o f th e National Institutes o f Health. Role o f the Sponsors: The funding source had no role in the design and conduct o f th e study; collection, management, analysis, and interpretation o f the data; preparation, review, or approval o f the manuscript; and decision to submit the manuscript fo r publication. Disclaimer: The contents are solely the responsibility o f the authors and do n ot necessarily represent the official view o f the National Institutes o f Health. Additional Contributions: The follow ing individuals provided unpublished data, conducted secondary analyses, assisted w ith study identification, and/or provided guidance and support: Agneta Bjorck Linne, MS, PhD, and Hans Liedholm, MD, PhD (Malmo University Hospital, Sweden); Marcia E. Leventhal, RN, MSN, Sabina De Geest, PhD. RN. and Kris Denhaerynck, PhD, RN (Institute o f Nursing Science, University o f Basel, Switzerland); Lars Rytter, MD (Glostrup University Hospital, Denmark); Gillian A. Whalley, PhD (University o f Auckland, New Zealand); David Maslove, MD, FRCPC (University o f Toronto, Canada); Judith Garcia-Aymerich, MD, PhD
- 74. (Universitat Pomeu Fabra-Barcelona, Spain); Bonnie J. Wakefield, PhD, RN (Iowa City Veterans Affairs Healthcare System); Kathleen Finn, MD (D epartm ent o f Medicine, Massachusetts General Hospital, Boston); Jon C. Tilburt, MD, MPH (Mayo Clinic); Christiane E. Angermann, MD (Universitatsklinikum Wurzburg, Denmark); Felipe Atienza, MD, PhD (Hospital General Universitario Gregorio Maranon-Madrid, Spain); Dan Gronseth, BS (Mayo Clinic); Michael W. Rich, MD (Washington University, St Louis); A ndrew Masica, MD, MSCI (Baylor Health Care System); Karen B. Hirschman, PhD, and Mary D. Naylor, PhD (University o f Pennsylvania School o f Nursing); James F. Graumlich, MD (University o f Illinois College o f Medicine at Peoria); Anna Stromberg, RN, PhD (Linkoping University Hospital, Sweden). These contributors were not compensated fo r th e ir contributions. REFERENCES 1. Jencks SF, Williams MV, Coleman EA. Rehospitalizations among patients in th e Medicare fee-for-service program. N Engl J Med. 2 0 0 9 :3 6 0 (14):1418-1428. 2. Committee on Redesigning Health Insurance Performance Measures, Payment, and Performance Im provem ent Programs. Rewarding Provider Performance: Aligning Incentives in Medicare. Washington, DC: National Academies Press; 2 0 0 6 . 3. Medicare Payment Advisory Commission. Report to the Congress: Promoting Greater Efficiency in Medicare. Washington, DC: Medicare Payment
- 75. Advisory Commission; 2007. 4 . Joynt KE, Jha AK. A path forw ard on Medicare readmissions. N Engl J Med. 2013;368(13):1175-1177. 5. Shippee ND, Shah ND, May CR, Mair FS, M ontori VM. Cumulative complexity: a functional, patient-centered model o f patient com plexity can improve research and practice. J Clin Epidemiol. 2012;65(10):1041-1051. 6. Gallacher K, May CR, M ontori VM, Mair FS. Understanding patients' experiences o f treatm ent burden in chronic heart failure using normalization process theory. Ann Earn Med. 2011;9(3):235-243. 7. Sav A, Kendall E, McMillan SS, et al. 'You say treatm ent, I say hard w ork': treatm ent burden among people w ith chronic illness and th e ir carers in Australia. Health Soc Care Community. 2013;21 (6):665-674. 8. Krumholz HM. Post-hospital syndrom e-an acquired, transient condition o f generalized risk. N Engl J Med. 2013;368(2):100-102. 9. Leppin AL, Ting HH, Gionfriddo MR, et al. Describing the usefulness and efficacy o f discharge interventions: predicting 30 day readmissions through application o f the cumulative com plexity model (protocol). 2013. http://kerunit.fMes .wordpress.com/2011/07/ccm-readmissions -protocolll.docx. Accessed September 1,2013. 10. Moher D, Liberati A, Tetzlaff J, Altman DG; PRISMA Group. Preferred reporting items for
- 76. systematic reviews and meta-analyses: th e PRISMA statement. PLoSMed. 2 0 0 9 ;6 (7 ):e 1 00 0 09 7 . It. Hansen LO, Young RS, Hinami K, Leung A, Williams MV. Interventions to reduce 30-day rehospitalization: a systematic review. Ann Intern Med. 2011:155(8):520-528. 12. Higgins JP. Altman DG, Gatzsche PC, e t al; Cochrane Bias Methods Group; Cochrane Statistical Methods Group. The Cochrane Collaboration's tool jamainternalmedicine.com JAMA Internal Medicine July 2014 Volume 174, Number 7 1105 Research Original Investigation Preventing 30-Day Hospital Readmissions fo r assessing risk o f bias in randomised trials. BMJ. 2011;343:d5928. 13. Sterne JA, Egger M. Funnel plots fo r detecting bias in meta-analysis: guidelines on choice o f axis. J Clin Epidemiol. 2001;54(10):1046-105S. 14. DerSimonian R, Kacker R. Random-effects model fo r meta-analysis o f clinical trials: an update. Contemp Clin Trials. 2007;28(2):105-114. 15. Mantel N, Haenszel W. Statistical aspects o f the analysis o f data from retrospective studies o f disease. J Natl Cancer Inst. 1959:22(4):719-748. 16. Cochran WG. Some m ethods fo r strengthening
- 77. th e common x 2 tests. Biometrics. 1954;10:417-451. 17. Higgins JP, Thompson SG, Deeks JJ, Altman DG. Measuring inconsistency in meta-analyses. BMJ. 2003;327(7414):557-560. 18. Herrera-Espineira C, Rodriguez del Aguila MdelM, Navarro Espigares JL, et al. Effect o f a telephone care program after hospital discharge from a trauma surgery unit [in Spanish], GacSanit. 2011;25(2):133-138. 19. M elton LD, Foreman C, Scott E, McGinnis M, Cousins M. Prioritized post-discharge telephonic outreach reduces hospital readmissions fo r select high-risk patients. Am J Manag Care. 2012:18(12): 838-844. 20. Marusic S, Gojo-Tomic N, Erdeljic V, e t al. The effect o f pharmacotherapeutic counseling on readmissions and emergency departm ent visits. Int J Ciin Pharm. 2013;35(1):37-44. 21. Altfeld SJ, Shier GE, Rooney M, e t al. Effects o f an enhanced discharge planning intervention for hospitalized older adults: a randomized trial. Gerontologist. 2013;53(3):430-440. 22. Davis KK, Mintzer M, Dennison Him melfarb CR, Hayat MJ, Rotman S, Allen J. Targeted intervention improves knowledge b ut not self-care or readmissions in heart failure patients w ith mild cognitive im pairm ent. EurJ Heart Fail. 2012;14(9): 1041-1049. 23. Bowles KH, Hanlon AL, Glick HA, et al. Clinical
- 78. effectiveness, access to, and satisfaction w ith care using a telehomecare substitution intervention: a randomized controlled trial. In tJ Telemed Appl. 2011:2011:540138. 24. Finn KM, Heffner R, Chang Y, et al. Improving the discharge process by embedding a discharge facilitator in a resident team. J Hasp Med. 2011:6(9): 4 9 4 -5 0 0 . 25. Wong FK, Ho MM, Yeung S, Tam SK, Chow SK. Effects o f a health-social partnership transitional program on hospital readmission: a randomized controlled trial. SocSci Med. 2011;73(7):960-969. 26. Leventhal ME, Denhaerynck K, Brunner-La Rocca HP, e t al. Swiss Interdisciplinary Management Programme fo r Heart Failure (SWIM-HF): a randomised controlled trial study o f an outpatient inter-professional management programme for heart failure patients in Switzerland. Swiss Med Wkly. 2011;141:W13171. 27. Rytter L, Jakobsen HN, Ronholt F, e t al. Comprehensive discharge follow -up in patients' homes by GPs and district nurses o f elderly patients: a randomized controlled tria l. Scand J Prim Health Care. 2010;28(3):146-153. 28. Koehler BE, Richter KM, Youngblood L, e t al. Reduction o f 30-day postdischarge hospital readmission or emergency departm ent (ED) visit rates in high-risk elderly medical patients through delivery o f a targeted care bundle. JHosp Med. 2009;4(4):211-218.
- 79. 29. Braun E, Baidusi A, Alroy G. Azzam ZS. Telephone follow -up improves patients satisfaction follow ing hospital discharge. EurJ Intern Med. 2009;20(2):221-225. 3 0. Courtney M, Edwards H, Chang A, Parker A, Finlayson K, Hamilton K. Fewer emergency readmissions and better quality o f life fo r older adults at risk o f hospital readmission: a randomized controlled trial to determine the effectiveness o f a 24-week exercise and telephone follow -up program. JA m GeriatrSoc. 2009;57(3):395-402. 31. Jack BW, Chetty VK, Anthony D, et al. A reengineered hospital discharge program to decrease rehospitalization: a randomized trial. Ann Intern Med. 2009;150(3):178-187. 32. Wakefield BJ, Ward MM, Holman JE .etal. Evaluation o f home telehealth follow ing hospitalization fo r heart failure: a randomized trial. Telemed JE Health. 2008;14(8):753-761. 33. Balaban RB, Weissman JS, Samuel PA, Woolhandler S. Redefining and redesigning hospital discharge to enhance patient care: a randomized controlled study. J Gen Intern Med. 2 00 8 :2 3 (8): 1228-1233. 34. Wong FK, Chow S, Chung L, e t al. Can home visits help reduce hospital readmissions? randomized controlled trial. JAdvNurs. 2 0 0 8 :6 2 (5):585-595. 35. Coleman EA, Parry C, Chalmers S, Min SJ. The
- 80. care transitions intervention: results o f a randomized controlled trial. Arch Intern Med. 2 0 0 6 ; 166(17):1822-1828. 36. Linne AB, Liedholm H. Effects o f an interactive CD-program on 6 m onths readmission rate in patients w ith heart fa ilu re -a randomised, controlled trial [NCT00311194], BMC Cardiovasc Disord. 2 0 0 6 :6 :3 0 . 37. Casas A, Troosters T, Garcia-Aymerich J, et al; members o f the CHRONIC Project. Integrated care prevents hospitalisations fo r exacerbations in COPD patients. EurRespirJ. 2006;28(1):123-130. 38. Riegel B, Carlson B, Glaser D. Romero T. Randomized controlled trial o f telephone case management in Hispanics o f Mexican origin w ith heart failure. J Card Fail. 2006:12(3):211-219. 39. Koelling TM, Johnson ML, Cody RJ, Aaronson KD. Discharge education improves clinical outcomes in patients w ith chronic heart failure. Circulation. 2005;111(2):179-185. 40. M ejhert M, Kahan T, Persson H, Edner M. Lim ited long term effects o f a management programme fo r heart failure. Heart. 2 0 0 4 :9 0 (9 ): 1010-1015. 41. Kwok T, Lum CM, Chan HS, Ma HM, Lee D, Woo J. A randomized, controlled trial o f an intensive com m unity nurse-supported discharge program in preventing hospital readmissions o f older patients w ith chronic lung disease. JAm GeriatrSoc. 2004;52(8):1240-1246.
- 81. 42. Doughty RN, W right SP, Pearl A, e t al. Randomized, controlled trial o f integrated heart failure management: the Auckland Heart Failure Management Study. Eur Heart J. 2002;23(2):139-146. 43. JaarsmaT, HalfensR, Huijer Abu-Saad H .e ta l. Effects o f education and support on self-care and resource utilization in patients w ith heart failure. Eur Heart J. 1999;20(9):673-682. 44. Naylor MD, Brooten D, Campbell R, e t al. Comprehensive discharge planning and home follow -up o f hospitalized elders: a randomized clinical trial. JAMA. 1999;281(7):613-620. 45. Stewart S, Pearson S, Luke CG, H orow itz JD. Effects o f home-based intervention on unplanned readmissions and out-of-hospital deaths. JAm GeriatrSoc. 1998;46(2):174-180. 46. Dunn RB, Guy PM, Hardman CS, Lewis PA, V etter NJ. Can a house call by a public health nurse improve th e quality o f th e discharge process for geriatric patients? Clin Perform Qual Health Care. 1995;3(3):151-155. 47. Rich MW, Beckham V, W ittenberg C, Leven CL, Freed land KE, Carney RM. A m ultidisciplinary intervention to prevent th e readmission o f elderly patients w ith congestive heart failure. N Engl J Med. 1995;333(18):1190-1195. 48. Naylor M, Brooten D, Jones R, Lavizzo-Mourey R, MezeyM, Pauly M. Comprehensive discharge
- 82. planning fo r the hospitalized elderly: a randomized clinical trial. Ann Intern Med. 1994;120(12):999-1006. 4 9. Naylor MD. Comprehensive discharge planning fo r hospitalized elderly: a pilot study. Nurs Res. 1990;39(3):156-161. 50. Kulshreshtha A, Kvedar JC, Goyal A, Halpern EF, Watson AJ. Use o f remote m onitoring to improve outcomes in patients w ith heart failure: a p ilo t trial. In tJ Telemed Appl. 2010:2010:870959. 51. Graumlich JF, Novotny NL, Nace GS, e t al. Patient readmissions, emergency visits, and adverse events after software-assisted discharge from hospital: cluster randomized trial. J Hasp Med. 2009;4(7):11-19. 52. Atienza F, Anguita M, Martinez-Alzamora N, e t al; PRICE Study Group. M ulticenter randomized trial o f a comprehensive hospital discharge and outpatient heart failure management program. Eur J Heart Fail. 2004;6 (5 ):6 4 3-6 5 2. 53. Riegel B, Carlson B. Is individual peer support a promising intervention fo r persons w ith heart failure? J Cardiovasc Nurs. 2004;19(3):174-183. 54. Stowasser DA, Collins DM, Stowasser M. A randomised controlled trial o f medication liaison service s-p a tien t outcomes. J Pharm Pract Res. 2002;32(2):133-140. 55. Li H, Powers BA, Melnyk BM, et al. Randomized controlled trial o f CARE: an intervention to improve outcomes o f hospitalized elders and family
- 83. caregivers. Res Nurs Health. 2012;35(5):533-549. 56. Shyu Yl, Liang J, Wu CC, e t al. A pilot investigation o f th e short-term effects o f an interdisciplinary intervention program on elderly patients w ith hip fracture in Taiwan. JAm GeriatrSoc. 2005;53(5):811-818. 57. Angermann CE, Stork S, Gelbrich G, e t al; Competence Network Heart Failure. Mode o f action and effects o f standardized collaborative disease management on m ortality and m orbidity in patients w ith systolic heart failure: the Interdisciplinary Network fo r Heart Failure (INH) study. Circ Heart Fail. 2012;5(1):25-35. 58. Naylor MD, Brooten DA, Campbell RL, Maislin G, McCauley KM, Schwartz JS. Transitional care of older adults hospitalized w ith heart failure: a randomized, controlled trial [published correction 1106 JAMA Internal Medicine July 2014 Volume 174, Number 7 jamainternalmedicine.com Preventing 30-Day Hospital Readmissions Original Investigation Research appears in JA m GeriatrSoc. 2004;52(7):1228]. JA m GeriatrSoc. 2 004;52(5):675-684. 59. Stromberg A, Martensson J, Fridlund B. Levin LA, Karlsson JE, Dahlstrom U. Nurse-led heart failure clinics improve survival and self-care behaviour in patients w ith heart failure: results
- 84. from a prospective, randomised trial, Eur Heart J. 2003;24(11):1014-1023. 6 0 . Hansen FR, Poulsen H, Sorensen KH. A model o f regular geriatric follow -up by home visits to selected patients discharged from a geriatric ward: a randomized controlled trial. Aging (Milano). 1995; 7(3):202-206. 61. Maslove DM, Leiter RE, Griesman J, et al. Electronic versus dictated hospital discharge summaries: a randomized controlled trial. J Gen Intern Med. 2009;24(9):995-1001. 62. Forster AJ. Clark HD, Menard A, e ta l. Effect o f a nurse team coordinator on outcomes for hospitalized medicine patients. Am J Med. 2005;118 (10):1148-1153. 63. Dudas V, Bookwalter T, Kerr KM, Pantilat SZ. The im pact o f follow -up telephone calls to patients after hospitalization. Am J Med. 2001;111(9B): 26S-30S. 6 4. Parry C, Min SJ, Chugh A, Chalmers S, Coleman EA. Further application o f the care transitions intervention: results o f a randomized controlled trial conducted in a fee-for-service setting. Home Health CareServQ. 200 9;28(2-3):84-99. 65. Hesselink G, Schoonhoven L, Barach P, et al. Improving patient handovers from hospital to prim ary care: a systematic review. Ann intern Med. 2012;l57(6):417-428.
- 85. 6 6. Payne RA. Abel GA, Guthrie B, Mercer SW. The effect o f physical m ultim orbidity, mental health conditions and socioeconomic deprivation on unplanned admissions to hospital: a retrospective cohort study. CMAJ. 2013;185(5):221-228. jam ainternalmedicine.com JAMA Internal Medicine July 2014 Volume 174, Number 7 1107 Copyright 2014 American Medical Association. All Rights Reserved. Applicable FARS/DFARS Restrictions Apply to Government Use. This is a discussion post. PLEASE USE the textbook below for reference and at least one SCHOLARLY PEER-Review American Nurses Association. (2015). Nursing: Scope and standards of practice (3rd ed.). Silver Spring, MD: Author. Your capstone change project begins this week when you identify a practice issue that you believe needs to change. The practice issue must pertain to a systematic review that you must choose from a List of Approved Systematic Reviews for the capstone project, whose link may be found in the guidelines for the Week 3 Capstone Project: Milestone 1 assignment page. · 1st part Choose a systematic review from the list of approved reviews based on your interests or your practice situation. · Formulate a significant clinical question related to the topic of the systematic review that will be the basis for your capstone change project. · Relate how you developed the question. · Describe the importance of this question to your clinical practice previously, currently, or in the future.
- 86. · Describe what a research-practice gap is. 2nd part Now that you have identified your capstone change project, it is time to look at its feasibility. · What tangible and intangible resources will be needed to implement your project? · What improved outcomes do you anticipate will occur that could indicate the project produced a successful return on investment (ROI) of these resources? · How will you communicate your plan for change with key decision makers so that they will support the allocation of the resources you are seeking? Overview Write a five-page analysis of the American Civil War. This assessment allows you to demonstrate your understanding of a critical event in American history. SHOW LESS By successfully completing this assessment, you will demonstrate your proficiency in the following course competencies and assessment criteria: · Competency 3: Examine how the Civil War was a catalyst for economic change. . Analyze the conflict between industry and agriculture in America. . Examine the economic shifts after the Civil War. . Analyze the cultural shift after the Civil War. . Investigate the emotional impact of the Civil War. . Analyze whether slavery might have been profitable for the South in 1860. · Competency 6: Communicate effectively in a variety of formats. Context America's Bloodiest War
- 87. America's bloodiest war was not fought overseas. The Civil War had the highest number of American casualties. Almost three quarters of a million men and women died. Many more than that were wounded and disfigured. The war was fought and won by more populous and fully developed states against those who were less developed, much more agrarian, and prone to using human beings as little more than animals. Slavery was an abomination, but the upper classes in these states could not or would not abolish it. The South aspired to be the major cotton supplier to the world. In order to do so, the plantation owners there clung to the notion that slavery remained necessary, all the more so, if the plantation economy were to be introduced into new territories destined for statehood lying further west. Questions to consider To deepen your understanding, you are encouraged to consider the questions below and discuss them with a fellow learner, a work associate, an interested friend, or a member of the business community.Suggested Resources The following optional resources are provided to support you in completing the assessment or to provide a helpful context. For additional resources, refer to the Research Resources and Supplemental Resources in the left navigation menu of your courseroom.Library Resources The following e-books or articles from the Capella University Library are linked directly in this course: · Coclanis, P. A., & Engerman, S. L. (2013). Would slavery have survived without the Civil War? Southern Cultures, 19(2), 66–90. · Post, C. (2011). Social-property relations, class-conflict and the origins of the U.S. Civil War: Towards a new social interpretation. Historical Materialism, 19(4), 129–168. · McCardell, J. M., Jr. (2014). Reflections on the Civil War. Sewanee Review, 122(2), 295–303. · Halpern, R., & Dal Lago, E. (Eds.). (2002). The growth of the cotton kingdom. In Slavery and Emancipation (pp. 123–145). Malden, MA: Blackwell Publishers.
- 88. SHOW LESSCourse Library Guide A Capella University library guide has been created specifically for your use in this course. You are encouraged to refer to the resources in the HIS-FP4100 – Critical Aspects of American History Library Guide to help direct your research.Bookstore Resources The resources listed below are relevant to the topics and assessments in this course and are not required. Unless noted otherwise, these materials are available for purchase from the Capella University Bookstore. When searching the bookstore, be sure to look for the Course ID with the specific – FP (FlexPath) course designation. · Keene, J. D., Cornell, S. T., & O'Donnell, E. T. (2016). Visions of America: A history of the United States (3rd ed.). Boston, MA: Pearson Education. . Chapter 12, "Slavery and Sectionalism: The Political Crisis of 1848–1861."‹ . Chapter 13, "A Nation Torn Apart: The Civil War 1861–1865." Assessment instructions Write a five-page examination of the American Civil War. Address the following in your examination: · Analyze the concept that the war was one between industry and agriculture, with industry coming out the winner. · Examine ways in which the Civil War was a catalyst for economic change. · Analyze how the cultural shift after the Civil War was not easily embraced. · Examine how the Civil War still has an emotional impact on people living today. · Examine whether technology such as the cotton gin could have affected the need for slavery in the South. Additional Requirements · Written communication: Written communication is free of errors that detract from the overall message.
- 89. · APA formatting: Resources and citations are formatted according to APA (6th edition) style and formatting. · Number of resources: Minimum of one peer reviewed resource. · Length of paper: Five typed, double-spaced pages. · Font and font size: Times New Roman, 12 point.