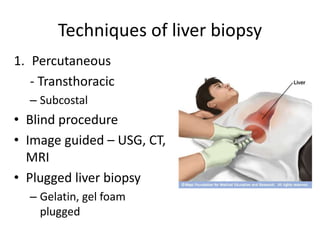
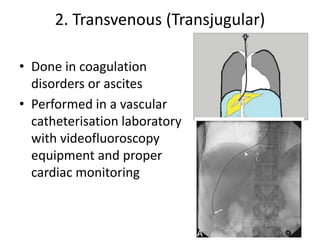
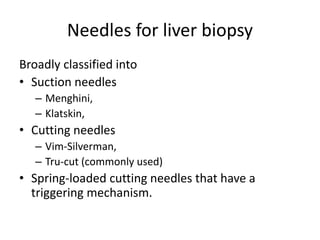
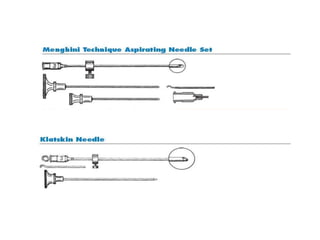
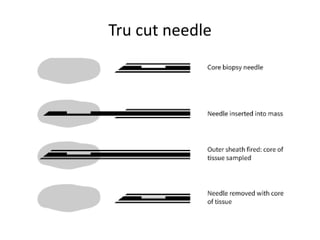
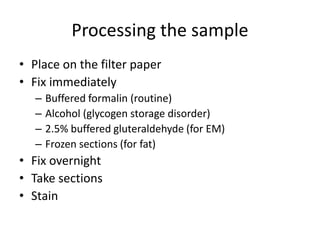
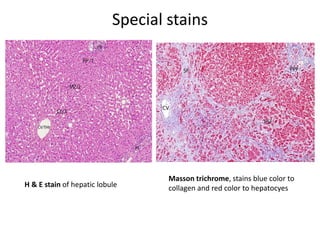
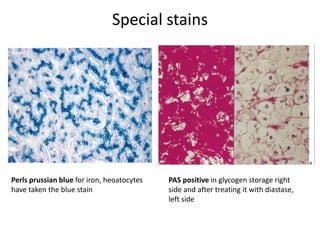
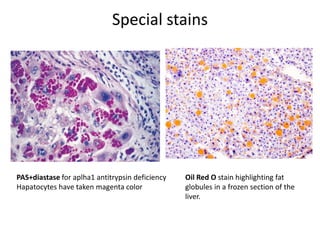
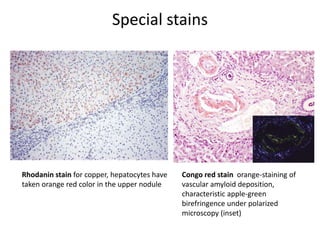
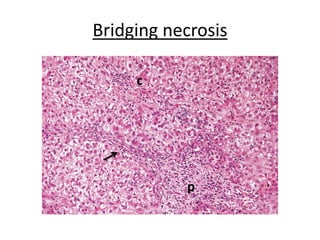
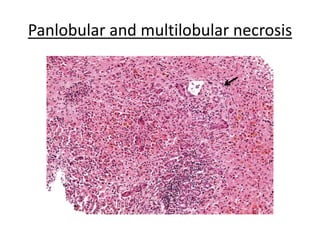
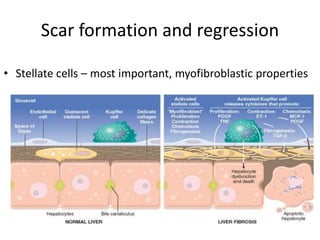
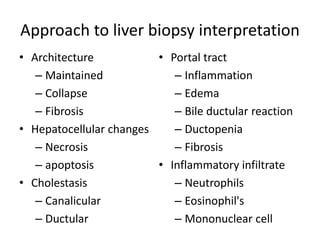
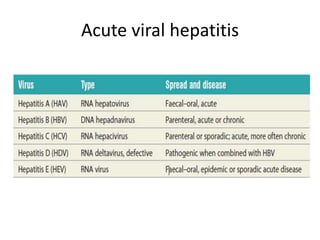
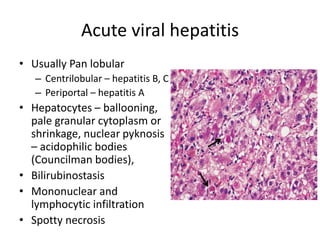
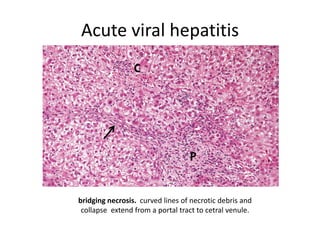
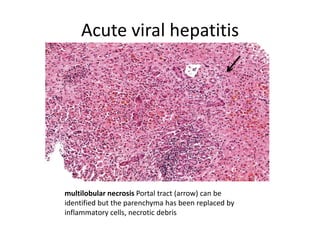
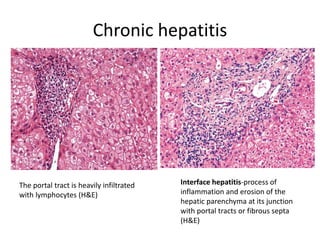
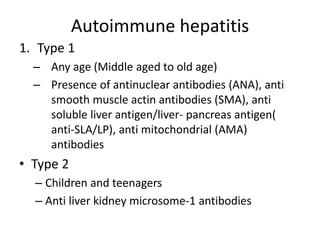
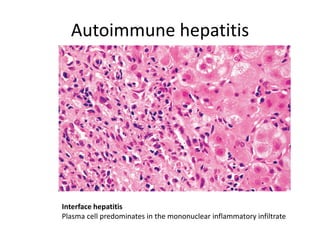
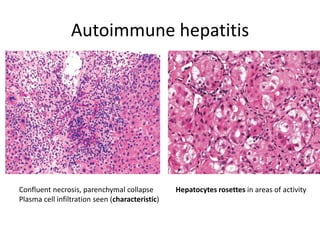
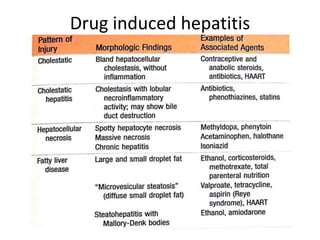
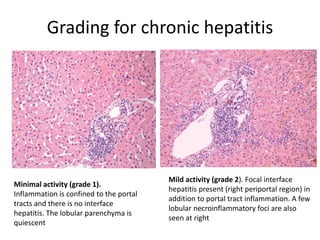
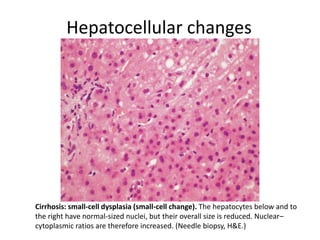
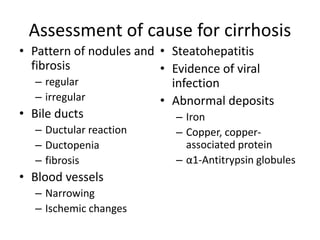
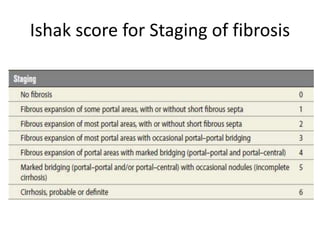
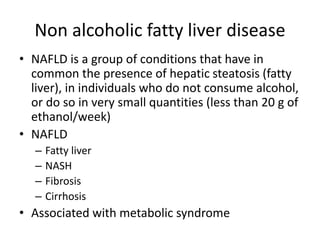
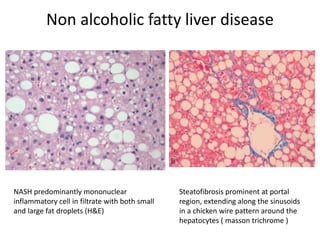
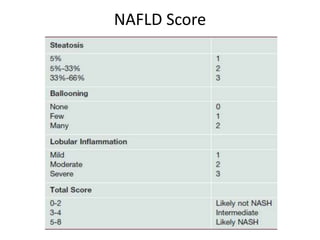
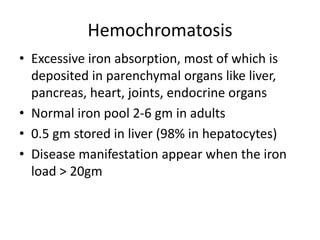
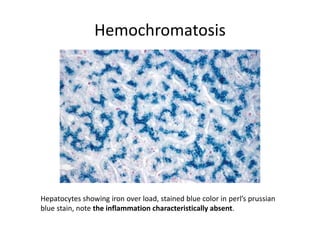
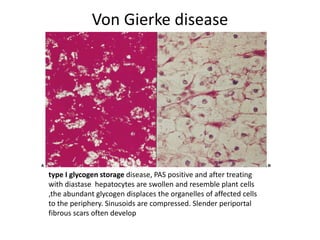
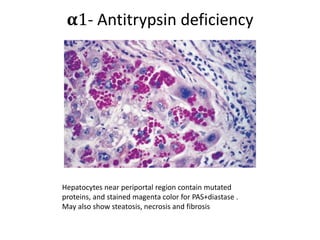
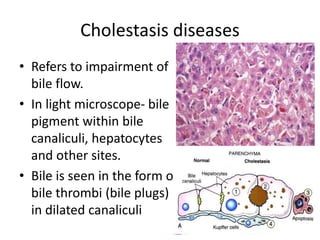
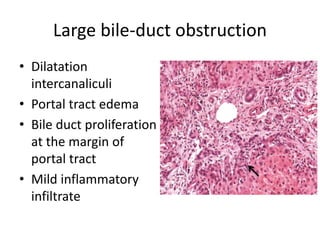
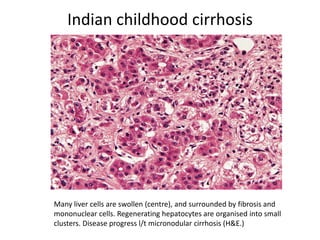
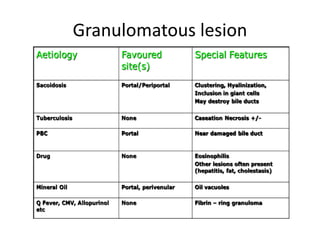
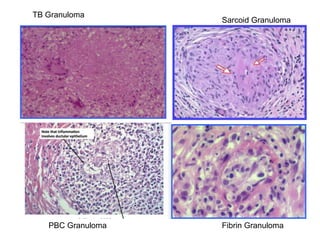
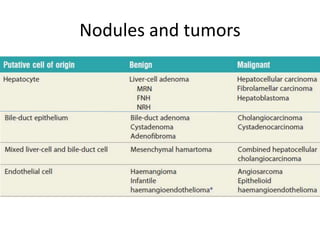
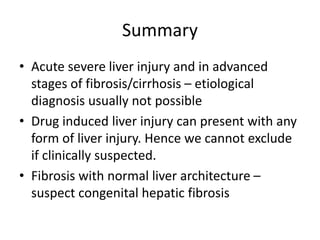
This document provides an overview of liver biopsy interpretation. It discusses the indications for liver biopsy, techniques used, histological examination and staining, and the approach to interpreting different pathological conditions of the liver seen on biopsy. Key points include the use of biopsy to diagnose and assess liver damage and prognosis, techniques including percutaneous and transjugular biopsies, examining features such as necrosis, inflammation, fibrosis and cirrhosis, and interpreting conditions like viral hepatitis, autoimmune hepatitis, non-alcoholic fatty liver disease, and hemochromatosis.