Puk
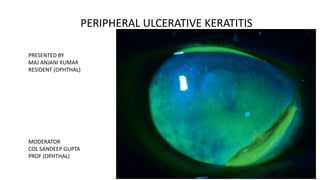
- 1. PERIPHERAL ULCERATIVE KERATITIS PRESENTED BY MAJ ANJANI KUMAR RESIDENT (OPHTHAL) MODERATOR COL SANDEEP GUPTA PROF (OPHTHAL)
- 2. REFERANCES
- 3. Introduction - • Peripheral ulcerative keratitis (PUK) is used to describe a group of destructive inflammatory diseases involving the peripheral cornea whose final common pathway is characterized by sloughing of corneal epithelium and keratolysis (corneal “melting”).
- 4. • Majority mediated by local and systemic immunological processes, although some of infectious etiology need proper evaluation. • One half of PUK of non infectious etiology are associated with CVD- RA, GPA, PAN. • If not properly treated, PUK can progress to perforation resulting in significant ocular morbidity, and when associated with a systemic autoimmune condition, may be potentially life-threatening.
- 6. Characteristics of the peripheral cornea • thickness (up to 0.7 mm) with tight collagen bundle packing; • vascular arcade originating from anterior ciliary arteries and extends approximately 0.5 mm into clear cornea (providing the nutritional supply but also access to the efferent arm of the immune response) • Presence of more Langerhans’ cells, higher concentrations of immunoglobulin M8 and first component of complement (C1), collagenase and proteoglycanase.
- 7. Pathogenesis Locally produced or circulating immune complexes lodged in limbal or peripheral corneal blood vessels Activation of the classic complement pathway in the presence of C1 Immune vasculitis resulting in damage to the vessel wall Chemotaxis of various inflammatory cells, proteins, and proinflammatory cytokines and the production of metalloproteinases Accelerate and propagate the peripheral corneal destructive process. Trigger factors- Trauma/infections Prior corneal surgery
- 8. Etiologies of PUK Ocular Noninfectious • Idiopathic • Acne rosacea (ocular) • Mooren’s ulcer • Traumatic, postoperative (may be a presenting feature of a systemic autoimmune disorder) • Exposure/neuroparalytic keratopathy Ocular Infectious • Bacterial (Staphylococcus, Streptococcus, Gonococcus [rare]) • Viral (herpes simplex and herpes zoster) • Amebic (Acanthamoeba) • Fungal
- 9. Systemic Noninfectious Collagen Vascular Diseases/Vasculitis • Rheumatoid arthritis (common) • Antineutrophil cytoplasmic antibody (ANCA)–associated vasculitides • Granulomatosis with polyangiitis (previously Wegener’s granulomatosis) (relatively common) • Polyarteritis nodosa (less common) • Microscopic polyangiitis (MPA) (less common) • Churg–Strauss syndrome (less common) • Relapsing polychondritis (uncommon) • Systemic lupus erythematosus (less common) • Progressive systemic sclerosis/scleroderma (rare) • Giant cell arteritis (very rare)
- 10. Other Systemic Autoimmune • Cicatricial pemphigoid (especially with trichiasis) (rare) • Inflammatory bowel disease (very rare) • Sarcoidosis (very rare) • Sjögren’s syndrome • Leukemia/malignancy (very rare) • Inflammatory bowel disease (usually associated with a nonulcerative peripheral keratitis) • Giant cell arteritis (rare)
- 11. Systemic Infectious • Gonorrhea • Bacillary dysentery • Tuberculosis • Borreliosis (Lyme disease—very rare) • Varicella zoster • Helminthiasis
- 12. OCULAR MANIFESTATIONS Foreign body sensation, pain, and photophobia -epithelial erosion and ulceration. Vision affected –if peripheral inflammatory process proceeds centrally or from induced astigmatism. Anterior uveitis may contribute to photophobia with reduction of visual acuity. Pain may be severe if associated scleritis occurs.
- 13. Progressive Circumferential Peripheral Corneal Ulceration. (A) A 60-year-old female with idiopathic peripheral ulcerative keratitis. Slit-lamp microscopy demonstrates depth of stromal necrolysis. There is inflammatory infiltrate at both the peripheral and central edges. (B) Fluorescein staining
- 14. The specific clinical findings at presentation will depend on the severity and rate of progression of the disease, as well as the timing between the onset and clinical evaluation. Corneal melting, once initiated, may progress very rapidly. The amount of stromal loss apparent after corneal scrapings are performed to evaluate for infectious causes. Limbal, conjunctival, and episcleral injections occur frequently. Concurrent scleritis denotes a higher likelihood of active vasculitis. The finding of PUK with scleritis portends a worse ocular and systemic outcome than when scleritis occurs alone. Cataract and glaucoma may occur as a result of the inflammatory processor the use of corticosteroids.
- 15. RA WITH PUK Nearly 50% of patients with PUK have an associated systemic disease, with the large majority of these being the collagen vascular diseases (CVDs). Rheumatoid arthritis (RA) is the most common CVD associated with PUK, likely due to its high prevalence in the population (affecting 2.5%–3% of adults). Pathogenesis immune complex deposition in the limbal vessels immune-mediated vasculitis leakage of inflammatory cells and proteins. activation of complement system and increases cytokine production, recruiting neutrophils and macrophages that release collagenases and other proteases that in turn cause corneal tissue destruction. Studies have shown that increased cytokines may also stimulate an increase in matrix metalloproteinase production by keratocytes themselves
- 16. Slit lamp photograph of the right eye of a 50-year-old patient with RA and acute marginal stromal infiltrates Slit lamp photograph of diffuse anterior and posterior scleritis in a 67-year-old patient with RA
- 17. Keratolysis may occur associated with necrotizing scleritis in inflamed or noninflamed eyes. Loss of stroma occurs in regions of clear cornea and may progress to descemetocele formation. Corneal and scleral stromal lysis with wound dehiscence has also been described after cataract, strabismus, and other intraocular surgeries in patients with RA, often in patients with preoperative KCS. Postoperative scleral or corneal necrosis may, in fact, be the first manifestation of a systemic vasculitic process, and such patients should receive an appropriate autoimmune work-up with a consulting rheumatologist to rule out RA or other autoimmune disorders. Slit lamp photograph of necrotizing scleritis 1 week after phacoemulsification with intraocular lens implantation. Note eroded running suture and prolapsed uveal tissue
- 18. PUK WITH GPA Non specific disease causing conjunctival and scleral inflammation leading to corneal thinning if systemic therapy delayed. PUK may manifest at the onset. Ocular involvement in 50-60% Dx- ANCA Focal necrotizing scleritis with peripheral keratitis (box) in Wegener's granulomatosis Peripheral anterior stromal and subepithelial infiltrates (1) in Wegener's granulomatosis
- 19. PAN Ocular findings occur in a minority of patients (10–20%),[ most commonly involving the retinal vessels. This may occur secondary to the hypertension or there may be vasculitis involving retinal vessels. Conjunctival nodules caused by edema and necrosis of conjunctival vessels as well as uveitis have also been reported. Anterior segment findings are infrequent but include scleritis, sclerokeratitis, and peripheral ulcerative keratitis. The scleritis may be diffuse and associated with peripheral keratitis and ulceration, or more focal with peripheral corneal Mooren's-like ulceration. Bilateral peripheral ulceration with perforation in a patient with microscopic polyarteritis has also been reported. Treatment focuses on the systemic disease and involves the use of corticosteroids and, more importantly, cytotoxic agents, which have markedly improved the outcome.
- 20. Peripheral ulcerative keratitis in a patient with polyarteritis nodosa Clinical characteristic similar to Mooren’s Ulcer. Hbs Ag + in 50% Development of PUK in a pt with already diagnosed PAN on therapy – indication for vigorous therapy
- 21. GCA Giant cell arteritis (GCA) or temporal arteritis is a systemic vasculitis of medium to large vessels. Ocular manifestations include ischemic optic neuropathy, amaurosis fugax, diplopia and ophthalmoplegia, and retinal vessel occlusion. Formed visual hallucinations have also been reported. Anterior segment findings are infrequent. Scleritis has been reported. Anterior segment ischemia with diffuse corneal edema, hypotony, and keratic precipitates has been reported, presumably secondary to inflammation involving the long posterior ciliary arteries. Bilateral peripheral corneal ulceration without infiltration has been reported in a single case of temporal arteritis. Peripheral ulcerative keratitis in a patient with giant cell arteritis
- 22. DIAGNOSTIC AND ANCILLARY TESTING • Workup of Peripheral Ulcerative Keratitis (Noninfectious) • CBC • RF • Anti-CCP • c-ANCA and p-ANCA • ESR and CRP, CIC • Urine analysis • Radiographs • Chest • Sinus
- 23. Medical treatment • Topical Corticosteroid- in milder PUK, not a/w CVDs • Systemic corticosteroids- oral prednisone 1 mg/kg/day- acute management of more severe cases of PUK. • If progression occurs, pulsed methylprednisolone (0.5–1.0 g) for three consecutive days may be effective
- 24. Indications for Systemic Immunomodulatory Therapy in Peripheral Ulcerative Keratitis (PUK) 1. PUK associated with a potentially lethal systemic disease, such as rheumatoid arthritis, Wegener’s granulomatosis, relapsing polychondritis, polyarteritis nodosa 2. PUK with associated scleritis 3. Bilateral Mooren’s ulcer 4. Disease progression despite local conjunctival resection and tectonic procedures (e.g., tissue adhesive)
- 26. Surgical treatment • Conjunctival resection • Tissue adhesives & Flaps/AMT • Lamellar graft/ PK
- 27. Mooren’s ulcer Rare, chronic, painful, peripheral ulcerative keratitis (PUK), was first described in detail as a clinical entity by Mooren in 1867. Unilateral, occurs in the fourth decade or later, responsive to local surgical and medical therapy. The disease is strictly a peripheral ulcerative keratitis (PUK), with no associated scleritis. Bilateral, more resistant to systemic immunosuppression, painful, relentless, progressive destruction of the cornea, usually in younger individuals (third decade), many of whom are of African descent Pathogenesis- autoimmune reaction against a specific target molecule in the corneal stroma, which may occur in genetically susceptible individuals. Both cellular and humoral mechanisms have been postulated. The conjunctival epithelium demonstrates increased levels of several inflammatory mediators. Mooren’s ulcer in patients with concurrent hepatitis C respond to IFN-α- common antigenic source.
- 28. Acute Mooren’s Ulcer. Peripheral thinning and an overlying epithelial defect are present in an inflamed eye. Mooren’s Ulcer. Peripheral thinning is present in a relatively quiet eye in this patient who had a history of Mooren’s ulcer, now in remission
- 29. An early Mooren's ulcer characterized by a crescent-shaped peripheral ulcer concentric to limbus; the leading edges are undermined and infiltrated. Clinical Features Symptoms redness, tearing, and photophobia, but pain is typically the outstanding feature. The pain often is incapacitating and may well be out of proportion to the inflamma decreased visual acuity, which may be secondary to associated iritis, central corneal involvement, or irregular astigmatism due to peripheral corneal thinning.
- 30. Signs Typically, Mooren's ulcer begins as a crescent-shaped gray-white infiltrate in the peripheral cornea. Epithelial breakdown and stromal melting follow this. Eventually it develops into a characteristic chronic crescent-shaped peripheral ulcer. The ulcer is concentric to limbus; the leading edges are undermined, infiltrated, and deepithelialized. The ulcer progresses circumferentially and centrally. As it progresses, it creates an overhanging edge at its central border. Though the ulcer may begin as a shallow furrow in the peripheral cornea, over time it may involve the limbus. The adjacent conjunctiva and sclera are usually inflamed and hyperemic.
- 31. As the disease progresses, the ulcer spreads in three directions: peripherally, centrally, and rarely into sclera. Behind the advancing edge of the ulcer, healing may take place. This healing is in the form of corneal epithelialization and vascularization. Associated with this is scarring and thinning. The healed area remains clouded. In an advanced case of Mooren's ulcer most of the cornea is lost, leaving behind a central island surrounded by area of grossly thinned, scarred, and vascularized tissue . Although the disease is characterized by progressive thinning, corneal perforation is uncommon and is more common in eyes with peripheral as compared to total ulceration. Iritis sometimes is associated with Mooren's ulcer. Hypopyon is rare unless secondary infection is present. Glaucoma and cataract may complicate the process
- 32. Advanced Mooren's ulcer characterized by gross destruction of cornea, leaving behind a central island of tissue
- 33. Differential Diagnosis Although Mooren's ulcer has a characteristic clinical picture, several other diseases can present with peripheral keratitis and ulceration. The differential diagnosis of Mooren's ulcer includes other inflammatory and noninflammatory causes of peripheral thinning and ulceration. ocular systemic Terrien’s Marginal degenerations Tuberculosis Pellucud Marginal degenerations Varicella zoaster Idiopathic furrow degeneration Syphillis Staphylococcal marginal Keratitis Sarcoidosis Rosacea keratitis CVDs Exposure keratitis RA GPA
- 34. Diagnosis As previously stated, Mooren's ulcer is idiopathic, and the characteristic features must occur in the absence of any systemic process that may cause PUK. Thus, it is a diagnosis of exclusion. Detailed history with specific attention to history of systemic illness, and a complete ocular and systemic examination. The laboratory studies should include complete and differential blood cell counts, platelet counts, erythrocyte sedimentation rate, rheumatoid factor, antinuclear antibody, antineutrophil cytoplasmic antibodies, chest X-ray examination, liver enzymes, and fluorescent treponemal antibody absorption test. Additional testing is done as indicated by the review of systems and physical examination. Infectious etiologies should be excluded by appropriate cultures, because microbial keratitis can rapidly progress and is usually amenable to antibiotic therapy.
- 35. Treatment The goals of treatment in Mooren's ulcer are to stop the ulcerative process and allow reepithelialization of the cornea. Four strategies underlie most of these treatments: (1) local immunosuppression, (2) systemic immunosuppression, (3) removal of local stimulatory antigens, and (4) removal of distant stimulatory antigens. The following stepwise approach to management is recommended: (1) topical corticosteroids, (2) conjunctival resection, (3) systemic immunosuppression, and (4) additional surgery. Topical corticosteroids: These are used aggressively on an hourly basis, along with topical prophylactic antibiotics and cycloplegic medications. When the cornea shows signs of reepithelialization the steroid therapy is tapered gradually over months. It is important to monitor for cataracts and an increase in intraocular pressure. Conjunctival resection: This removes involved conjunctiva and blocks collagenase and the immune response to corneal antigen by providing a biological barrier. In this procedure, conjunctiva adjacent to the corneal ulcer is resected up to 2 clock hours on either side to bare sclera and extends 3–4 mm from the limbus. Postoperatively, topical corticosteroids and antibiotics are continued.
- 36. Systemic immunosuppression Those cases of bilateral or progressive Mooren's ulcer that fail therapeutic steroids and conjunctival resection will require systemic cytotoxic chemotherapy to bring a halt to the progressive corneal destruction. It is better to start this treatment sooner rather than later, before the corneal destruction has become too extensive for surgery. Systemic corticosteroids can be given to suppress inflammation and arrest progressive corneal thinning. The recommended dosage for oral prednisolone is 1–1.5 mg/kg body weight/day. The dosage is adjusted according to the severity of the disease and is tapered slowly when improvement occurs. Alternatively, to avoid side effects associated with long-term corticosteroid therapy, patients can be given intravenous pulse therapy of methylprednisolone. Other systemic immunosuppressants used in the management of Mooren's ulcer are: cyclophosphamide (2 mg/kg/day), methotrexate (7.5–15 mg once weekly), and azathioprine (2 mg/kg/day). The degree of fall in white blood cell count is considered as the most reliable indicator of immunosuppression produced by cyclophosphamide. Oral ciclosporin A (3–4 mg/kg/day) has been successfully used to treat a case of bilateral Mooren's ulcer unresponsive to local therapy as well as systemic immunosuppression. Ciclosporin A works by suppression of the helper T-cell population and stimulation of the depressed population of suppressor and cytotoxic T cells present in these patients. Although immunosuppression is effective, close follow-up is necessary to ensure that the white blood cell count does not reach a dangerously low level. The administering physician must be vigilant about adverse effects of these cytotoxic and immunosuppressive medications.
- 37. Additional Surgery Keratoepithelioplasty Lamellar keratectomy Lamellar keratoplasty- The procedure removes antigenic targets of the cornea, prevents immunological reactions, reconstructs the anatomy and prevents it from perforating, and improves vision. The surgical procedure involves removal of necrotic ulcerative cornea and reconstruction of anatomical structure using lamellar donor lenticule. The surgical plan depends on the shape of the ulcer and infiltration of the cornea. If the ulcer is smaller than a half circle of the limbus and the central cornea is not involved, a crescent-shaped lamellar graft is used. If the ulcer is larger than two-thirds of a circle of the limbus and the central cornea is intact, then a doughnut-shaped lamellar graft is used. If the central cornea is involved, a full lamellar graft is used to maintain visual acuity. For perforation of peripheral cornea, double lamellar grafts comprising a thin inner graft with endothelium for repair of perforation and another lamellar graft on the surface whose shape depends on the shape of the ulcer is used. Chen at al. reported a cure rate of 73.7% after the first procedure of LKP plus 1% ciclosporin A eyedrops and a final cure rate of 95.6%. Tissue adhesives and bandage contact lens Tectonic grafts (Patch graft or penetrating keratoplasty)
- 38. Prognosis • The clinical course, response to therapy, and eventual prognosis of Mooren's ulcer are related to disease presentation. • The disease can present as a unilateral disorder, a bilateral nonsimultaneous disorder, or a bilateral simultaneous disorder. • Patients with unilateral disease usually respond best to therapy and have the best prognosis. • Patients with simultaneous bilateral disease usually do the worst. Patients with nonsimultaneous bilateral disease fall in between.
- 39. Staphylococcal Marginal Keratitis • Staphylococcal marginal keratitis, also referred to as catarrhal infiltrates or ulcers, is a peripheral corneal disorder characterized by inflammatory infiltration that may lead to ulceration. • It is likely the most common disorder of the peripheral cornea. • Thygeson first reported the frequent association of catarrhal infiltrates with chronic conjunctivitis due to Staphylococcus. • These peripheral ulcers differed from central ulcers in their relatively benign course and the lack of bacteria found in corneal scrapings. • Accordingly, these lesions are thought to represent an antibody response to toxins rather than direct bacterial invasion.
- 40. Pathogenesis Similar to phlyctenulosis, bacterial antigens from chronic staphylococcal colonization of the eyelids are thought to trigger an immune response in a sensitized cornea. The immune response is most likely a type III hypersensitivity reaction resulting in immune complex deposition in the peripheral cornea. These complexes activate the complement pathway, attracting neutrophils to the site forming an opacity (catarrhal infiltrate). In support of this theory, immunoglobins and C3 complement have been demonstrated in marginal infiltrates.Further, Gram and Giemsa staining of corneal scrapings show neutrophils but no organisms.
- 41. Clinical features Patients with staphylococcal marginal keratitis usually present with pain, photophobia, foreign body sensation, and conjunctival injection. The symptoms are typically mild to moderate and are not specific.
- 42. Staphylococcal marginal keratitis. Fluorescein examination reveals overlying epithelial defects. These lesions can be confused with infectious keratitis, and microbial evaluation may be indicated
- 43. Differential diagnosis 1) infectious corneal ulcers. Infectious ulcers are usually more painful, more central in location, and have a modest anterior chamber reaction. 2) Herpes simplex virus keratitis - HSV infection begins with an epithelial defect followed by an infiltrate, which is the reverse order in staphylococcal marginal keratitis. Dendritic or geographic epithelial lesions and profound corneal hypoesthesia are other distinguishing features of herpes simplex keratitis. 3) peripheral ulcerative keratitis caused by collagen vascular diseases (e.g. rheumatoid arthritis). staphylococcal marginal keratitis tends to have a benign course, collagen vascular-associated ulcers tends to be more severe and progressive. staphylococcal marginal keratitis responds rapidly to topical corticosteroids, whereas patients with peripheral corneal ulcers related to collagen-vascular disease often need systemic immunosuppression to control inflammation and may worsen on topical corticosteroids
- 44. Diagnostic evaluation • The diagnosis of staphylococcal marginal keratitis is usually made based on clinical findings. • In cases where there is an overlying epithelial defect, exclusion of infectious processes is important. • corneal scrapings for culture- with an associated epithelial defect and a significant anterior chamber reaction/equivocal diagnosis • Microbial evaluation is also recommended if clinical improvement is not observed or if the infiltrates progress despite therapy.
- 45. Treatment • Topical corticosteroids (i.e. fluorometholone, loteprednol, and prednisolone acetate) are the mainstay in the treatment of acute marginal staphylococcal infiltrates. • In cases of corneal stromal infiltrates without epithelial breakdown, topical corticosteroids may be used immediately. In cases with epithelial breakdown and stromal ulceration, a broad- spectrum topical antibiotic should be used briefly prior to starting topical corticosteroids. • Eyelid hygiene is used to remove bacteria from the lashes and lid margins, while antibiotic ointments are used to limit bacterial colonization. • Systemic antibiotics (i.e. tetracycline, doxycycline, erythromycin) may be indicated when the disease is recurrent or if there is significant meibomian gland disease. • Recently, a topical form of azithromycin has become commercially available that is applied to the eyelid and may provide broad-spectrum antibioisis with once-daily dosing.
Editor's Notes
- Patient With Early Nasal Peripheral Ulceration Measuring About 1 O’ Clock Hour. There is inflammatory stromal infiltrate more central to the ulceration with associated episcleral inflammation.
- Slit lamp photograph of a patient with peripheral ulcerative keratitis (PUK). Note the sectoral location with associated scleritis, corneal infiltrate, and overlying epithelial defect.
- Staphylococcal marginal keratitis. (A) These infiltrates are hypersensitivity reactions to staphylococcal antigen usually associated with blepharitis. There is a clear ‘lucid’ interval between the infiltrate and the limbus. These lesions respond well to topical corticosteroids Multiple marginal infiltrates near the limbus. Some of these may coalesce into broader lesions