Diagnosis of hemolytic anemia
- 1. Diagnosis of Hemolytic Anemia
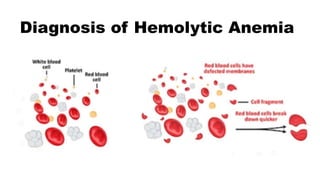
- 2. • Hemolytic anemia is defined as anemia due to a shortened survival of circulating RBCs due to their premature destruction. • Typical lifespan of a RBC is ~ 110 to 120 days (four months) • Hemolytic anemia may be mild to potentially life- threatening .
- 3. Causes of Hemolytic anemia can be categorized as : 1. Intrinsic or Extrinsic to the RBC (Intracorpuscular versus Extracorpuscular defects) 2. Inherited or Acquired 3. Acute or chronic 4. Immune versus Non-immune mechanism 5. Intravascular versus Extravascular hemolysis Most of the inherited conditions are intracorpuscular Most of the hemolysis by an immune mechanism is extravascular.
- 4. 1. Intrinsic (or intracorpuscular): 1. Molecular defect inside the RBC ( e.g G6PD deficiency ,Hemoglobinopathies) 2. An abnormality in membrane structure or function (e.g Hereditary Spherocytosis) Intrinsic or Extrinsic to the RBC (Intracorpuscular versus Extracorpuscular defects)
- 5. 2. Extrinsic (or extracorpuscular): a. Antibodies directed against RBC membrane components (eg, AIHA, alloimmune hemolytic anemia, acute hemolytic transfusion reaction , delayed hemolytic transfusion reaction , some drug- induced hemolytic anemias). b. Stasis, trapping, and destruction of RBC in an enlarged spleen (Hypersplenism). c. Mechanical trauma to the RBCs (Malfunctioning cardiac valves, ventricular assist devices); fibrin stands across vessels that shear RBCs in DIC; or platelet microthrombi in TTP, HUS, or drug- induced thrombotic microangiopathy (DITMA).
- 6. 2. Extrinsic (or extracorpuscular): d. Exposure to compounds with oxidant potential (eg, aniline dyes, dapsone, phenazopyridine) in individuals with an underlying metabolic defect such as G6PD deficiency, congenital methemoglobinemia, or unstable Hgb variants (eg, sulfonamides), as well as those without an underlying defect e. Administration of Rho(D) immune globulin to an RhD-positive individual (eg, for treatment of immune thrombocytopenia) or administration of IVIG f. Destruction of RBC by pathogens (eg, malaria, babesiosis, bartonellosis, clostridium perfringens) g. Less common causes include snake and insect bites, certain toxins, thermal burns, and copper poisoning (eg, Wilson disease).
- 7. Immune versus non-immune Immune hemolysis generally refers to RBC destruction by antibodies and/or complement proteins bound to the RBC surface. Immune hemolysis is characterized by: 1. A positive direct antiglobulin test (DAT; also called direct Coombs test) and/or 2. A positive indirect antiglobulin test (also called indirect Coombs test, or, in the setting of pretransfusion testing, referred to as an antibody screen).
- 8. Immune causes Warm autoimmune hemolytic anemia Drug-induced immune hemolysis Transfusion reactions (eg, ABO incompatibility, alloantibodies) Paroxysmal cold hemoglobinuria Paroxysmal nocturnal hemoglobinuria Cold agglutinin disease Intravenous infusion of IVIG or anti-RhD immune globulin Immune versus non-immune
- 9. Non-immune causes Hereditary Enzyme deficiencies (eg, deficiencies of G6PD, pyruvate kinase, glucose-phosphate isomerase, 5' nucleotidase) Hemoglobinopathies (eg, sickle cell disease, thalassemias, unstable hemoglobins) Membrane defects (eg, hereditary spherocytosis, hereditary elliptocytosis, hereditary stomatocytosis) Acquired Liver disease Hypersplenism Infections (eg, Bartonella, Babesia, malaria, clostridial sepsis) Oxidant agents (eg, dapsone, nitrites, aniline dyes) Toxins (eg, lead, copper, snake and spider bites) Infusion of a hypotonic solution Microangiopathic hemolytic anemia (eg, TTP, HUS, aortic stenosis, prosthetic valve leak) Immune versus non-immune
- 10. Intravascular hemolysis : Hemolysis that occurs primarily within the vasculature. Direct trauma, as in bongo drummers and march hemoglobinuria (runners' or foot- strike hemolysis) Shear stress, as in defective mechanical heart valves Heat damage, as in thermal burns Complement-induced lysis, as in PNH Osmotic lysis following infusion of hypotonic solutions Lysis from bacterial toxins (eg, clostridial sepsis) Lysis from exposure to high concentrations of copper Thrombotic microangiopathies (TMA) including TTP, HUS, or drug-induced TMA Acute hemolytic transfusion reaction Administration of Rho(D) immune globulin to RhD-positive individuals, such as for treatment of ITP Immune hemolysis that overwhelms the reticuloendothelial system (In the vasculature or in the reticuloendothelial macrophages in the liver and spleen) Intravascular versus Extravascular hemolysis
- 11. (In the vasculature or in the reticuloendothelial macrophages in the liver and spleen) Intravascular versus Extravascular hemolysis Extravascular hemolysis refers to hemolysis that occurs primarily via macrophages of the reticuloendothelial system in the liver, spleen, bone marrow, and lymph nodes. Severely damaged RBCs, especially those coated with complement, are primarily destroyed in the liver, an organ that receives a larger proportion of the cardiac output than the spleen. Poorly deformable RBCs such as spherocytes or sickled cells are primarily destroyed in the spleen, in the cords of Billroth.
- 13. Overview of the evaluation The diagnosis of hemolytic anemia is suspected in a patient with chronic or new onset symptoms of anemia (eg, fatigue, weakness, shortness of breath), a low hemoglobin level, and an increased reticulocyte count that is not explained by accelerated RBC production due to recent bleeding; repletion of iron, vitamin B12, folate, or copper; or administration of erythropoietin. Additional laboratory testing is often used to confirm the diagnosis of hemolytic anemia and to determine the likely cause. Testing to confirm hemolysis may be done simultaneously with testing to determine the cause, or sequentially. In some cases, testing to confirm hemolysis may be omitted if specific testing to determine the cause of hemolysis is rapidly available and likely to be definitive.
- 14. History and physical examination 1. A systematic approach, starting with a thorough history and physical examination is the cornerstone of the evaluation. 2. Helpful clues from the history and physical examination include the following, if present: a. Rapid onset of symptoms of anemia in the absence of bleeding is consistent with brisk hemolysis. b. Jaundice is consistent with brisk hemolysis that overwhelms the capacity of the reticuloendothelial system to convert heme to storage iron. c. Dark urine is consistent with intravascular hemolysis. d. Recent blood transfusion suggests possible acute hemolytic transfusion reaction; transfusion in the previous four weeks also raises the possibility of a delayed hemolytic transfusion reaction. e. Initiation of a new medication with potential for causing hemolysis suggests possible drug- induced etiology. f. History of hemolytic anemia or unexplained anemia in family members suggests an inherited disorder; this is more likely if multiple first degree family members are affected. g. History of pigmented gallstones or presence of gallstones implies chronic hemolysis that overwhelms the reticuloendothelial system.
- 15. Laboratory confirmation of hemolysis Most experts consider the diagnosis to be accepted if there are a majority of the following findings: 1. Anemia that is not due to another obvious cause. 2. Increased reticulocyte count that is not explained by accelerated RBC production due to recent bleeding; repletion of iron, vitamin B12, folate, or copper; or administration of erythropoietin. 3. Signs of RBC destruction such as Increased reticulocytes
- 16. Laboratory confirmation of hemolysis Additional test results that are consistent with a specific cause of hemolytic anemia (eg, schistocytes or spherocytes on peripheral blood smear; free hemoglobin or pink serum; newly positive direct antiglobulin [Coombs] test [DAT]; hemoglobin analysis demonstrating an abnormal hemoglobin) are highly supportive and in some cases diagnostic if schistocytes spherocytes
- 17. CBC/blood smear review • All patients for whom the diagnosis of hemolytic anemia is considered will have had a CBC . Hemolysis will be associated with some degree of anemia in the majority of cases. • Review of the peripheral blood smear is an extremely valuable tool for determining the presence and cause of hemolytic anemia. In many cases, findings on the blood smear are essential to providing life-saving treatment. Examples include thrombotic microangiopathies (TMAs) such as TTP or drug- induced TMA (DITMA); infections such as malaria or Babesia; and bite cells
- 18. High reticulocyte count • A high reticulocyte count implies an accelerated production of RBCs in the bone marrow. Increased reticulocytes is a typical finding in hemolytic anemia but is not specific for hemolysis; the bone marrow can also increase RBC production in response to bleeding, nutrient repletion (eg, vitamin B12, folic acid, iron), or erythropoietin administration. The absence of reticulocytosis does not eliminate the possibility of hemolysis, as some individuals have concomitant bone marrow suppression or reduced bone marrow function that interferes with production of reticulocytes. • The degree of reticulocytosis can be estimated from the peripheral blood smear, as reticulocytes are larger than mature RBCs, lack central pallor, and have a bluish tint (polychromasia) . The count can be quantified from a manual count on a peripheral blood smear stained for reticulin
- 19. High reticulocyte count • Reticulocytes can be expressed as a percentage of RBCs or as an absolute number; these numbers can be corrected for the degree of anemia and the lifespan of the reticulocytes in the circulation. In cases of markedly increased reticulocytosis or failure of the bone marrow to produce reticulocytes, any of these measures is likely to be a relatively good indicator of the degree of reticulocytosis. However, the corrections make the count more accurate, and in some
- 20. Reticulocyte percentage • The reticulocyte percentage conveys the percentage of all RBCs that are reticulocytes. • Since it is relative to the total RBC count, it may be artificially increased in severe anemia and artificially decreased if the patient is not anemic. • The normal reticulocyte percentage in a patient without hemolysis is in the range of 1 to 2 %. • In patients with hemolysis and an otherwise intact bone marrow, reticulocyte percentage is at least 4 to 5 %, and often considerably higher.
- 21. Corrected reticulocyte count • The reticulocyte percentage is a relative number. • For any given number of reticulocytes, a lower the total number of RBCs (the denominator) will raise the percentage of these RBCs that are reticulocytes. • Thus, the reticulocyte percentage can be multiplied by the patient's hematocrit divided by a normal hematocrit (eg, 45 %) to give a corrected reticulocyte percentage. • As an example, if reticulocytes are 10 % in a patient with a hematocrit of 22.5 %, the corrected count can be calculated as follows:
- 22. Absolute reticulocyte count • The absolute reticulocyte count has the advantage of accurately reflecting the degree of reticulocytosis regardless of the degree of anemia . • The normal absolute reticulocyte count is between 25,000 to 75,000/microL (ie, approximately 1 % of an absolute RBC count of 5,000,000 cells/microL). • An example of the utility of this measure is a severely anemic patient with a hematocrit of 18 %, a RBC count of 2,000,000/microL, and reticulocyte count of 3 %. • While the reticulocyte count of 3 % appears high, the absolute reticulocyte
- 23. Corrected absolute reticulocyte count • The more severe the anemia, the younger the reticulocytes are when they are released into the circulation, and hence the longer their lifespan in the circulation. • The absolute reticulocyte count can be corrected for the reticulocyte lifespan (RLS), also called the reticulocyte maturation time (RMT). • The RLS is 1.0, 1.5, 2.0, or 2.5 days at hematocrits of 45, 35, 25, and 15 percent, respectively . • In a patient with a hematocrit of 18 % and an absolute reticulocyte count of 60,000/microL, the RLS is approximately 2.5 days; thus, the corrected absolute reticulocyte count is (60,000 ÷ 2.5 = 24,000/microL), which is
- 24. Reticulocyte production index (RPI) • The RPI makes corrections for both the hematocrit and the reticulocyte lifespan : RPI = Reticulocytes (percent) x (HCT ÷ 45) x (1 ÷ RMT) • The RPI in an individual without hemolysis or blood loss is approximately 1. • A value in excess of 2 to 3 is considered increased, whereas a value <2 in a patient with anemia is considered inappropriately low .
- 25. High LDH and bilirubin; low haptoglobin • Hemolysis releases LDH and hemoglobin from RBCs. • Hemoglobin is bound by circulating haptoglobin, which facilitates heme recycling; hemoglobin is converted to bilirubin as part of the degradation and heme recycling process .
- 26. LDH and bilirubin • High LDH and bilirubin are not very specific for hemolysis, as there are numerous other possible causes of these abnormalities • When bilirubin elevation is due to hemolysis, the elevation is predominantly in the indirect (unconjugated) bilirubin.
- 27. Haptoglobin The normal range for serum haptoglobin is wide. A low haptoglobin is likely to be due to hemolysis, and an undetectable haptoglobin level is almost always due to hemolysis. Haptoglobin level of 25 mg/dL provided the best cutoff between hemolytic and non- hemolytic disorders . The sensitivity and specificity of a haptoglobin ≤25 mg/dL were 83 and 96 percent. Normal or increased haptoglobin does not eliminate the possibility of hemolysis because haptoglobin is an acute phase reactant that can be increased in the setting of inflammation . Other causes of low haptoglobin include abdominal trauma and congenital ahaptoglobinemia
- 28. Immediate management issues before the cause is identified Certain management issues may need to be addressed before the specific cause of hemolytic anemia is definitively established. Importantly, life-saving interventions should not be delayed while awaiting the results of diagnostic testing. 1.Rate of hemoglobin decline –Individuals with a very slow decline in hemoglobin may be able to adapt to and tolerate severe anemia without end organ ischemia, whereas those with brisk hemolysis and a rapid drop in hemoglobin level may be quite symptomatic and require more aggressive treatment and accelerated evaluation, even if the absolute hemoglobin level is not that low.
- 29. Immediate management issues before the cause is identified 2. Transfusion – Patients with severe anemia should be transfused with RBCs, especially if there is active bleeding, symptoms of organ ischemia, or ongoing brisk hemolysis. It may be appropriate to obtain a pre-transfusion blood sample that can be stored for later analysis, particularly if an inherited cause of hemolytic anemia is suspected. For patients with possible immune-mediated hemolysis for whom crossmatch compatible blood cannot be identified, blood designated for immediate release can be transfused. 3. Plasma exchange – In cases of presumed thrombotic microangiopathy (TMA; ie, microangiopathic hemolytic anemia and thrombocytopenia), diagnostic testing may take hours to days. 4. Hydration and hemodynamic support – For individuals with apparent severe intravascular hemolysis (eg, acute hemolytic transfusion reaction [AHTR] due to ABO incompatible transfusion), free hemoglobin in the circulation can cause renal failure, hypotension, and DIC .
- 30. In some of the obvious/classic presentations of hemolytic anemia, it may make sense to proceed directly to specific diagnostic testing : Anemia and thrombocytopenia with numerous schistocytes on the blood smear suggests a TMA such as TTP, HUS, or drug-induced TMA. Rapid onset of fever, back pain, dark urine, and pink plasma following a blood transfusion suggests an AHTR. Lifelong anemia, splenomegaly, and RBC morphology typical of one of the inherited disorders such as spherocytes , elliptocytes , or stomatocytes suggests a congenital RBC membrane/cytoskeletal defect. A blood smear characteristic of sickle cell disease or thalassemia in a patient with classic findings suggests a hemoglobinopathy. A rapid drop in hemoglobin level after exposure to a drug known to cause hemolysis suggests Post-diagnostic testing to determine the cause Obvious cause- proceed to specific testing
- 31. • In some cases, the cause of hemolysis may be less clear. As examples, the presence of numerous spherocytes could indicate autoimmune hemolytic anemia or hereditary spherocytosis. • For such individuals, use the direct antiglobulin (Coombs) test (DAT) to distinguish between hemolysis due to an immune mechanism (eg, AIHA) and hemolysis that is less likely to be due to an immune mechanism. Post-diagnostic testing to determine the cause Cause not obvious- start with Coombs test
- 32. • Used to determine whether patient RBCs are coated with IgG, complement, or both. The assay is performed by taking washed patient RBCs and incubating them with anti-human IgG and anti-human C3d antibodies. In AIHA, anti-human antibodies and/or anti-C3d antibodies form bridges (agglutination) between red cells by binding the human antibodies on the patient's red cells Cause not obvious- start with Coombs test Post-diagnostic testing to determine the cause
- 33. Selected testing to further narrow the diagnosis Post-diagnostic testing to determine the cause Other features that may be useful to test for in narrowing the diagnostic possibilities include the following: Evidence of intravascular hemolysis (eg, pink serum, positive serum free hemoglobin, positive urine dipstick for heme, positive urine for hemosiderin) suggests one of the following: 1. AHTR 2. Overwhelming bacterial infection (eg, from clostridium perfringens) 3. Paroxysmal nocturnal hemoglobinuria (PNH) 4. Paroxysmal cold hemoglobinuria (PCH) Red to brown urine in a patient with a normal plasma color may be due to transient hemolysis (if the samples were not evaluated simultaneously) or to a cause other than intravascular hemolysis (eg, myoglobinuria, beet ingestion).
- 34. Selected testing to further narrow the diagnosis Post-diagnostic testing to determine the cause Other features that may be useful to test for in narrowing the diagnostic possibilities include the following: Splenomegaly suggests a congenital, infectious, or neoplastic process. Abnormal finding on blood smear: 1. Spherocytes , microspherocytes, and elliptocytes suggest AIHA, assessed by DAT; or hereditary spherocytosis, assessed by tests for reduced eosin-5- maleimide (EMA) binding, increased osmotic fragility, and/or genetic testing. Elliptocytosis may also suggest myelodysplasia, assessed by bone marrow evaluation with chromosomal analysis. 2. Acanthocytes (spur cells) and target cells suggest liver disease. 3. Blister or "bite" cells suggest oxidant injury in the setting of G6PD deficiency. 4. Red cell "ghosts" indicate severe intravascular hemolysis, most often associated with overwhelming bacterial infection (eg, from clostridium perfringens).
- 35. • Thank you