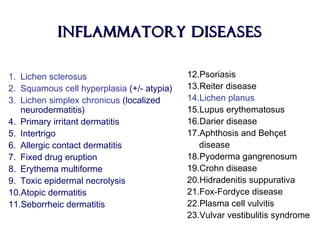
This document discusses several benign diseases of the vulva, vagina, and cervix. It describes conditions such as Bartholin's cyst, atrophic lichen (lichen sclerosus et atrophicus), and squamous cell hyperplasia. For each condition, it provides details on presentation, etiology, pathology findings, and treatment options. The document aims to comprehensively cover inflammatory diseases, blistering diseases, pigmentary changes, benign tumors, hamartomas and cysts, and congenital malformations that can affect the vulva, vagina, and cervix.