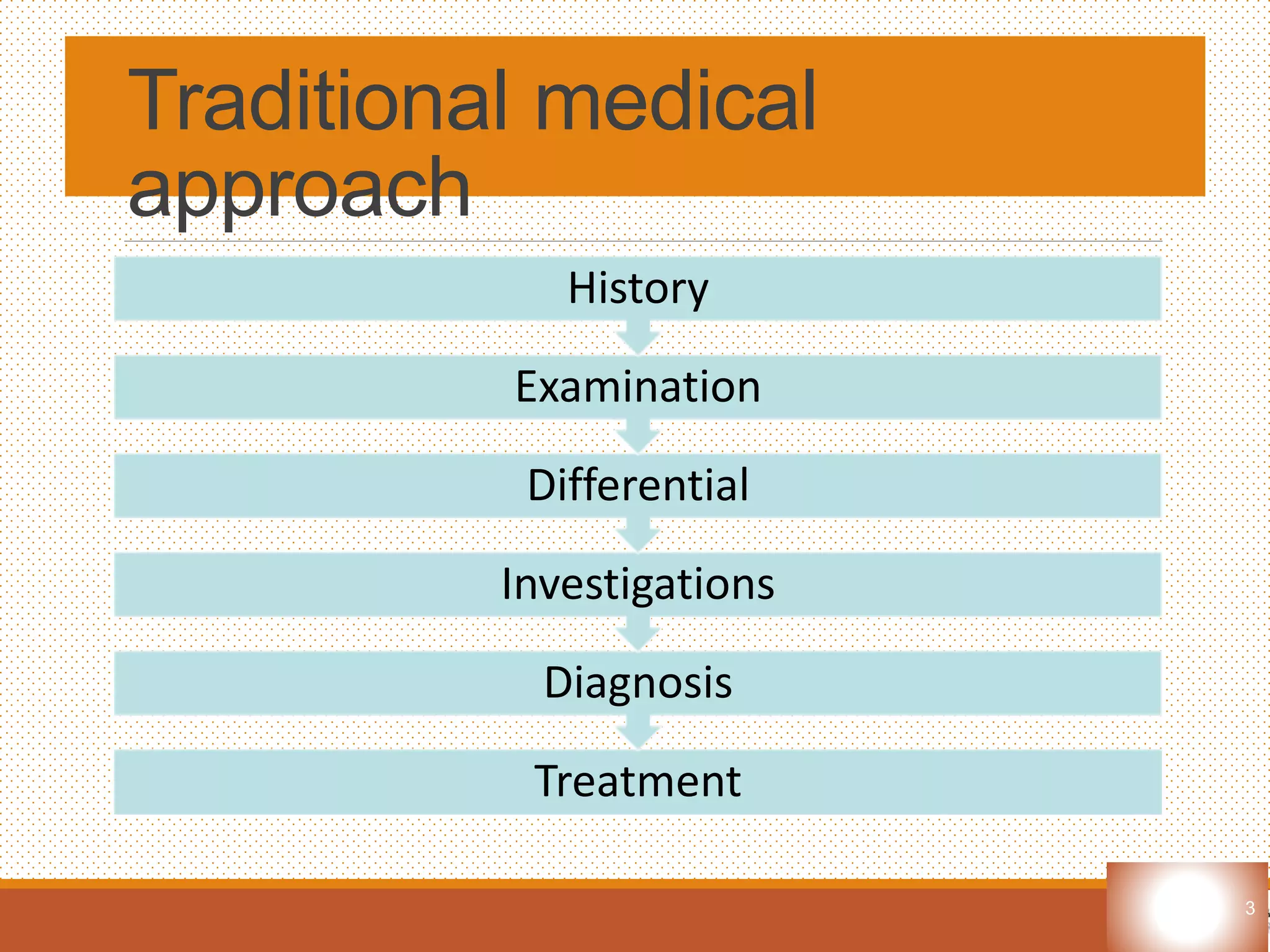
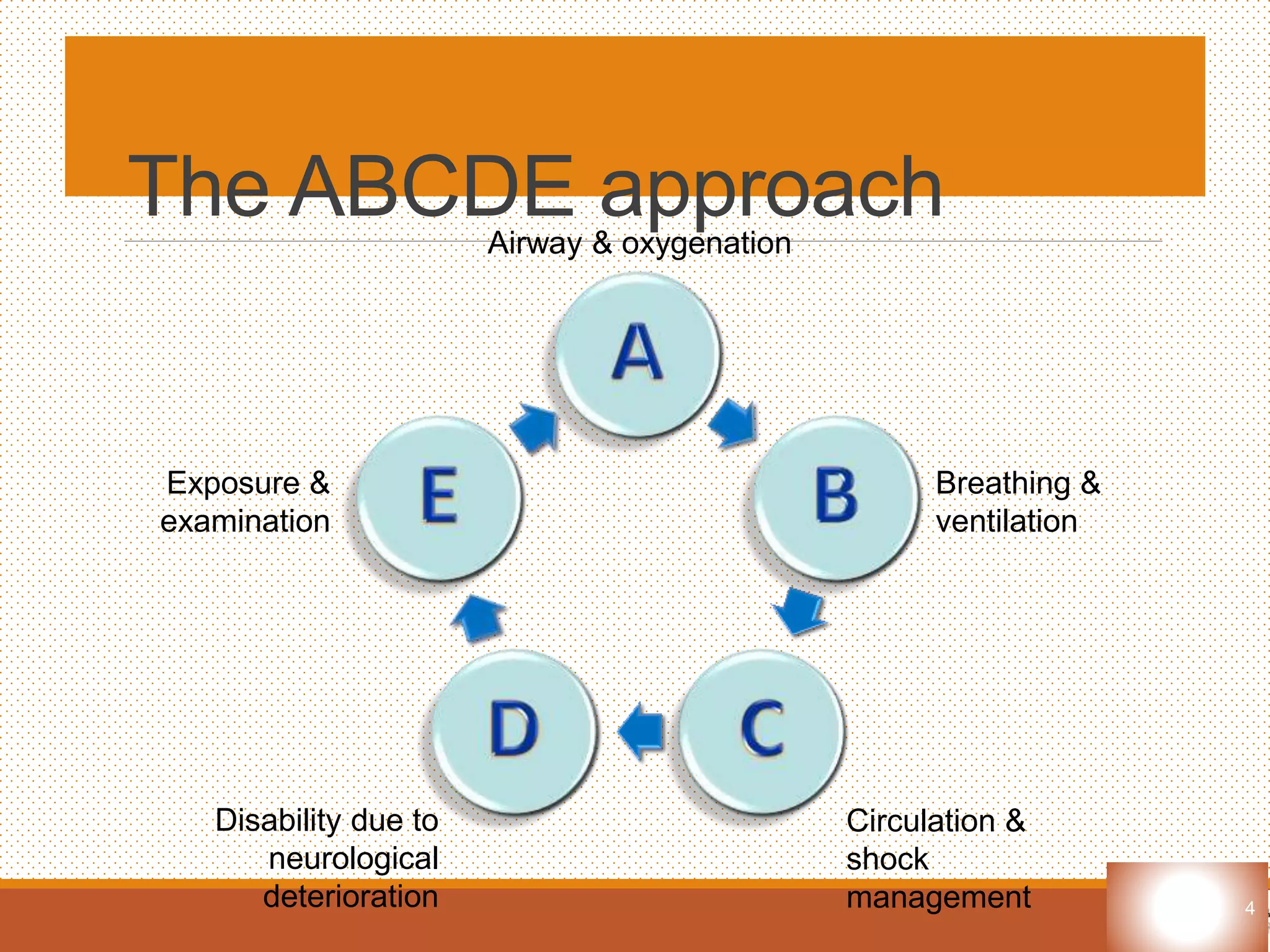
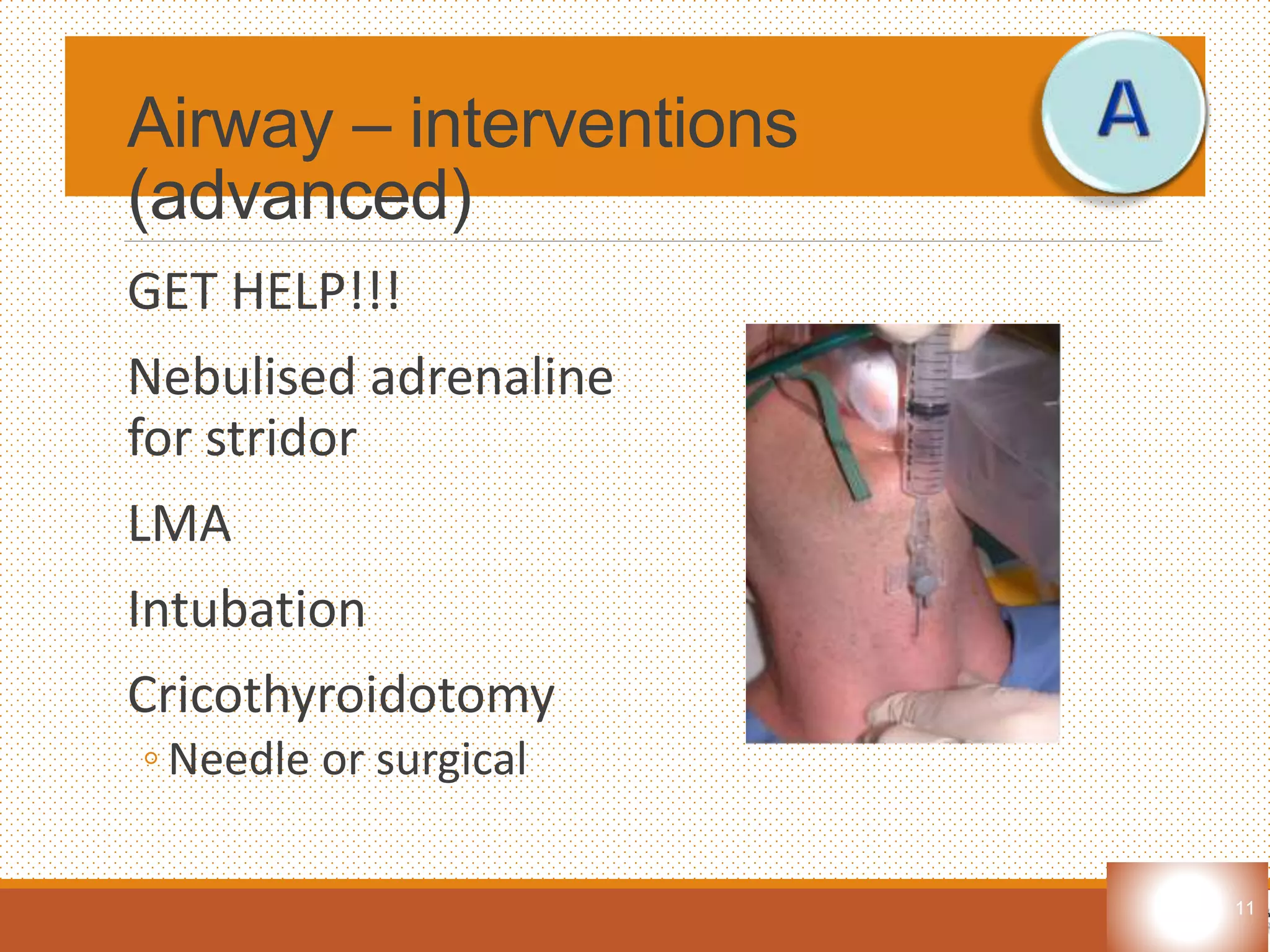
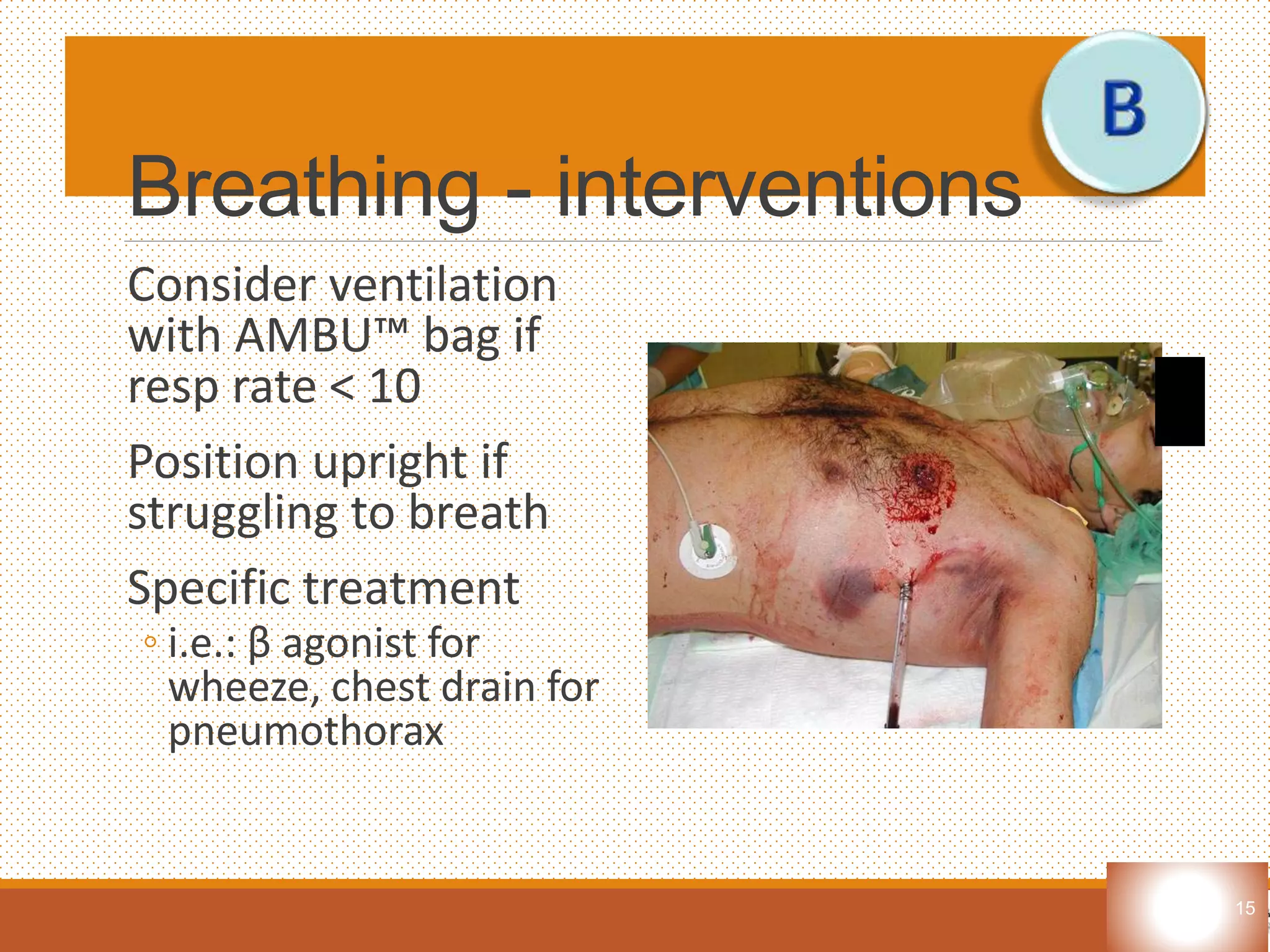
The document outlines the ABCDE approach for assessing and treating critically ill patients, focusing on airway, breathing, circulation, disability, and exposure. It emphasizes the importance of rapid assessment, immediate life-saving interventions, and continuous reassessment. Additionally, it discusses the primary and secondary survey processes, detailing specific interventions for various life-threatening conditions.