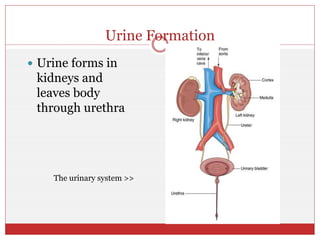
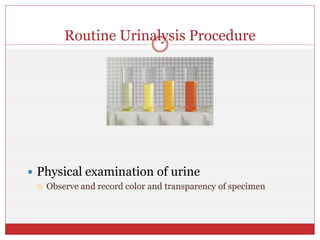
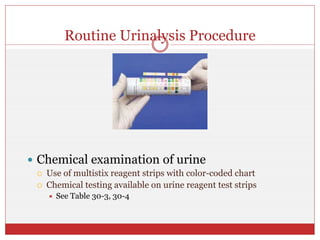
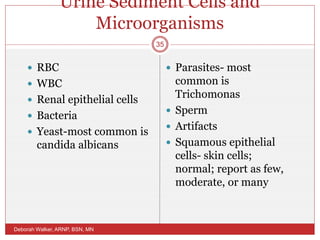
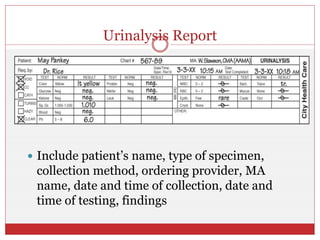
The document discusses urine formation and urinalysis. It describes how the kidneys filter waste from the blood to form urine, which is composed primarily of water and dissolved substances. It outlines the steps of routine urinalysis, including physical examination to assess attributes like color, specific gravity, and chemical testing using reagent strips. Microscopic examination of urine sediment is discussed to identify any cells, crystals, casts, bacteria, or parasites present that could indicate health issues. Quality control procedures and documentation standards are also reviewed.