OT 537 Session 1B
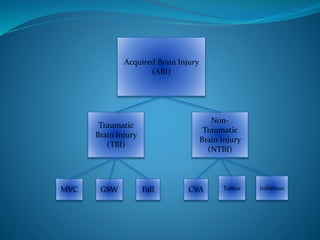
- 1. Acquired Brain Injury (ABI) Traumatic Brain Injury (TBI) Non- Traumatic Brain Injury (NTBI) CVA Tumor InfectionMVC GSW Fall
- 2. Traumatic Brain Injury (TBI) An injury caused by a bump, blow, jolt to the head or penetration to the brain that disrupts normal brain function Range from mild to severe Recommended resource: www.cdc.gov/TraumaticBrainInjury
- 3. TBI: Facts and Statistics ~1.7 million people sustain a brain injury annually in the U.S. TBI is a contributing factor to a third of all injury- related deaths in the U.S. Most TBIs that occur each year are concussions or other forms of mild TBI. Medical costs (direct and indirect, such as lost productivity) of TBI are estimated at over $80 billion in the United States yearly.
- 4. TBI Statistics By Age and Gender Children aged 0 to 4 years, adolescents aged 15 to 19 years, and adults >65 years old are most likely to sustain a TBI. Adults aged >75 years old have the highest rates of TBI-related hospitalization and death. In every age group, TBI rates are higher for males than for females. Males aged 0 to 4 years have the highest rates of TBI- related emergency department visits. Recommended resource: www.mayfieldclinic.com/PE-BrainTumor.htm
- 5. Leading Causes of TBI: Falls - 35.2% Motor Vehicle-Traffic Crashes (MVC) and Traffic-Related Incidents - 17.3% “Struck by/against” events - 16.5% Assaults - 10%
- 6. TBI and the Military Blasts are a leading cause of TBI for active duty military personnel in war zones. TBI is the signature wound of the wars in Iraq and Afghanistan.
- 7. TBI: Signs and Symptoms Recommended reference: www.cdc.gov/traumaticbraininjury/pdf/BlueBook_factsheet-a.pdf
- 8. TBI: Signs and Symptoms Chronic headache/neck pain Difficulty remembering, concentrating, or making decisions Perpetual fatigue Mood changes Changes in sleep patterns Light-headedness, dizziness, or loss of balance Increased sensitivity to light or sounds Nausea/vomiting Blurred vision Loss of sense of smell or taste Ringing in the ears http://www.cdc.gov/ncipc/tbi/Signs_and_Symptoms.htm
- 9. Acquired Brain Injury (ABI) Traumatic Brain Injury (TBI) Non- Traumatic Brain Injury (NTBI) CVA Tumor InfectionMVC GSW Fall
- 10. Non-Traumatic Brain Injuries Cerebrovascular accident (CVA, or “stroke”) Brain aneurysm (also called a cerebral or intracranial aneurysm) Brain tumor (benign/malignant, primary/secondary) Hypoxia or anoxia Infection – bacterial, viral, or other type
- 11. TBI vs. Non-TBI A TBI is a sudden injury to the head causing damage to the brain. Closed Head Injury – resulting from dynamic (acceleration/deceleration) or static loading (crush injury). Penetrating (Open) Head Injury Acquired Brain Injury (ABI) – can contribute to problems with cognitive abilities, thought coordination, communication difficulties, organizational skills and memory, physical problems, social difficulties, and independent functioning Localized/specific injury or effects vs. diffuse/whole-brain injury or effects No two cases will be the same. Differences will depend on factors including – Location of the injury in the brain Areas/structures of the brain affected Pre-injury influences
- 13. Consequences of ABI Acute phase – often profound deficits Long-term effects – subtle to severe Research indicates that around 90% of those with severe ABI overcome most of their physical difficulties within the first year. Problems common to all brain injuries include – Headaches Fatigue Epilepsy/seizures Although physical difficulties can present problems, it is the cognitive difficulties and personality changes that are the most distressing, since these have a greater impact on social, work, and family life. In the later stages - often viewed as a “hidden disability” Recommended resources: -http://www.lovethatmax.com/2008/11/what-happened-to-max.html -www.braininjurynetwork.org -http://www.strokesmart.org
- 15. Brain Map With a TBI, the brain may be injured in a specific location or the injury may be diffused to many different parts of the brain. Recommended resource: www.neuroskills.com/brain.shtml#map
- 16. Damage to the Cerebral Cortex
- 17. Damage to the Cerebral Cortex Wernicke’s aphasia – receptive language deficit Broca’s aphasia – expressive language deficit
- 18. The Story of Phineas Gage
- 19. The Frontal Lobe Frontal lobe damage also seems to have an impact on divergent thinking, or flexibility and problem solving ability.
- 20. The Frontal Lobe • Vulnerable to injury due to its location/size • Injury can come from direct impact to front of the head • Most common region of mild-moderate TBI • Can cause changes in personality, cognition (executive function), physical abilities, and behavior
- 21. The Frontal Lobe
- 22. Damage to the Frontal Lobe Difficulty sequencing Perseveration Attention deficits Personality changes/ social behavior Difficulty with problem-solving Loss of spontaneity Uncontrollable emotional, social, and sexual behavioral changes Poor initiation of voluntary movements Difficulty interpreting feedback from the environment Dysdiadochokinesia
- 23. The Parietal Lobe Near the back and top of the head Guides visual attention, touch perception, goal-directed movements, and manipulation of objects
- 24. Damage to the Parietal Lobe Difficulty naming objects (anomia) Inability to focus visual attention Problems with motor planning (apraxia) Impaired spatial orientation and constructing things (constructional apraxia) Left parietal damage can result in Gerstmann’s Syndrome: Difficulty with writing (agraphia) and math (acalculia) Inability to distinguish the fingers on the hand (finger agnosia) Right/left confusion Damage to the right parietal lobe can result in neglecting part of the body or space (left neglect) May also result in denial of deficits (anosagnosia)
- 25. The Temporal Lobe Located on the side of the head, above the ears Involved in the primary organization of sensory input Highly associated with memory skills Hearing ability Memory acquisition Some visual perceptions Categorization of objects
- 26. Damage to the Temporal Lobe Difficulty understanding spoken words (Wernicke's aphasia) Disturbance of selective attention Difficulty identifying and categorizing objects Difficulty recognizing faces (prosopagnosia) and visually locating objects Short-term memory loss Interference with long-term memory Changes in sexuality Persistent talking Increased aggressive behavior
- 27. The Occipital Lobe Located posteriorly, at the back of the head; not particularly vulnerable to injury b/c of its location The center of the visual perception system Involved in visuo-spatial processing, discrimination of movement, and color discrimination
- 28. Damage to the Occipital Lobe Vision defects (visual field cuts) Difficulty identifying colors Difficulty visually locating objects Hallucinations and visual distortions Word blindness Inability to recognize object movement Difficulty reading and writing Poor processing of visual information
- 29. The Cerebellum Located at the base of the skull, just above the brain stem, at the back of the head Involved in the coordination of voluntary motor movement, balance and equilibrium, and the regulation of muscle tone Relatively well protected from trauma
- 30. Damage to the Cerebellum Impaired gross and fine motor coordination Loss of the ability to walk Poor postural control Inability to make rapid movements (adiadochokinesis) Impaired control of eye movements (nystagmus) Tremors and/or dizziness Slurred speech The patient may appear to be intoxicated based on symptoms.
- 31. The Brain Stem Deep in the brain, leads to the spinal cord Plays a vital role in basic attention, arousal, and consciousness. All information to and from our body passes through the brain stem on the way to or from the brain Like the frontal and temporal lobes, is located in an area near bony protrusions making it vulnerable to damage during trauma. Controls breathing, heart rate, swallowing reflexes, vision, and hearing. Controls sweating, blood pressure, digestion, temperature, level of alertness, and ability to sleep. Governs sense of balance (vestibular function)
- 32. Damage to the Brain Stem Impaired regulation of temperature, heart rate, and respiration Difficulty swallowing food and drink (dysphagia) Difficulty with balance and movement Nausea and dizziness (vertigo) Impaired arousal and sleep regulations
- 33. Ataxia Results from impairment of the cerebellum or the motor pathways leading to and from the cerebellum. Ataxia is characterized by incoordination, impaired sitting balance, and standing balance. It can occur in the trunk and both the UE/LE. Trunk—impaired postural stability. UE—causes dysfunction of the gross and fine motor coordination. LE—impaired ability to ambulate while maintaining balance.
- 34. Postural Deficits A result of imbalance in muscle tone throughout the body (pelvis, trunk, head and neck, scapula, and UE/LE)
- 35. Balance A highly integrated dynamic process Impacted after brain injury by muscular weakness/spasticity, vestibular or proprioceptive deficits, ROM deficits, and visual impairment Addressed by OT in functional terms
- 36. Sensation Clients with TBI may exhibit signs of absent or altered sensation. Light Touch Sharp/Dull Proprioception Hot/Cold Pain Kinesthesia Two point discrimination Stereognosis Clients can also have altered smell/taste secondary to cranial nerve injuries.
- 37. Dysphagia A difficulty in chewing and/or swallowing There is a higher incidence of oral preparatory, oral, and pharyngeal stage dysphagia than esophageal dysphagia. A patient may also demonstrate abnormal tone in the oral muscles and/or abnormal oral reflexes. A patient may also demonstrate cognitive deficits which will interfere with sequencing chewing, swallowing, and breathing.
- 38. Behavior The first step to become more comfortable when working with individuals with TBI is to understand why they occur and how they manifest themselves. When working with an individual, you need to be aware of the environment, a patient’s triggers, and surrounding factors (ie. medication, family involvement, time of day, type of activity, etc.). Often behaviors include a patient being combative, agitated, disinhibited, or refusing to cooperate/participate in treatment.
- 40. Acquired Brain Injury (ABI) Traumatic Brain Injury (TBI) Non- Traumatic Brain Injury (NTBI) CVA InfectionMVC GSW
- 41. Classification of TBI Loss of Consciousness (LOC) Post-traumatic amnesia (PTA) Glasgow Coma Scale (GCS) MILD 0-30 minutes <1 day 13-15 MODERATE 30 minutes to 24 hours >1 day to <7 days 9-12 SEVERE >24 hours >1 week 3-8
- 42. Four Phases of Life in TBI Terms Survival Phase Establishing and living a new life (Duration: lifetime) Rehabilitation (or Recovery) Phase Rehab Facility, SNF, Home (Duration: weeks to months) Medical Treatment Phase Acute Phase – gurney to ICU (Duration: hours) Intensive Phase – ICU to acute hospital d/c (Duration: days/weeks) Pre-injury Phase
- 43. O.T. Evaluation Chart Review – Past medical history, diagnostic information Physical Evaluation – ROM, muscle tone, posture, sensation, transfers, ADLs and iADLs, motor abilities (Apraxia) Vision & Hearing – also visual-motor integration and visual perception Cognitive Evaluation Functional Status Emotional Status and Social Behavior See p. 1057 (RT) for resources for assessment and outcome tools
- 44. Glasgow Coma Scale scores range from 3-15. A score of 8 or below indicates a severe TBI, 9-12 moderate severity, and 13-15 a mild brain injury. Eye Opening Response: Spontaneous--open with blinking (4 points) Opens to verbal command, speech, or shout (3 points) Opens to pain, not applied to face (2 points) None (1 point) Verbal Response: Oriented (5 points) Confused conversation, but able to answer questions (4 points) Inappropriate responses, words discernible (3 points) Incomprehensible speech (2 points) None (1 point) Motor Response: Obeys commands for movement (6 points) Purposeful movement to painful stimulus (5 points) Withdraws from pain (4 points) Abnormal (spastic) flexion, decorticate posture (3 points) Extensor (rigid) response, decerebrate posture (2 points) None (1 point) The Glasgow Coma Scale (GCS) VIDEO: https://www.youtu be.com/watch?v=t MGhpMai4cQ
- 47. Rancho Los Amigos Scale Level I No Response: Total Assistance Level II Generalized Response: Total Assistance Level III Localized Response: Total Level IV Confused/Agitated: Maximal Assistance Level V Confused, Inappropriate Non-Agitated: Maximal Assistance Level VI Confused, Appropriate: Moderate Assistance Level VII Automatic, Appropriate: Minimal Assistance for Daily Living Skills Level VIII Purposeful, Appropriate: Stand-By Assistance Level IX Purposeful, Appropriate: Stand-By Assistance on Request Level X Purposeful, Appropriate: Modified Independent
- 48. Justin’s Story
- 49. Severe Disorders of Consciousness As seen in the ICU: • Trach • ICP Monitor • NG or G-tube • Restraints • Protocols for positioning and stimulation “The vast majority of individuals who cross that one-year mark without clear signs of consciousness are not going to recover consciousness after that.”
- 50. Transitioning from the Medical Treatment Phase to the Rehab/Recovery Phase after TBI Priorities: Medical stability Reduction of physical impairments Acquisition of basic self-care skills
- 52. Click here for demo videos: • Part 1 • Part 2
- 53. The Role of Occupational Therapy with Clients with Severe Disorders of Consciousness Restorative & Preventative Strategies ROM exercises Positioning protocols Tone alteration methods Reducing agitation by normalizing/regulating the environment Sensory stimulation (?) Family/caregiver education and support Intervention lays the foundation for later focus on occupational engagement.
- 54. The Role of Occupational Therapy with Clients with Emerging Functional Statuses after TBIStrategies to Promote Alertness/Participation and “Just Right Challenges” Optimizing motor function with a purposeful/functional foundation Improving strength and endurance Targeting balance and more automatic skills Maximizing freedom of movement and access to making choices while maintaining safety Addressing social-emotional and behavioral challenges Consulting with family/caregivers and rehab team “One step forward, two steps back”
- 55. The Role of Occupational Therapy in Facilitating Community Reintegration in Clients after TBI Centered on improving the acquisition and application of skills in the following areas: Physical abilities including functional mobility Cognitive functioning Social integration Productivity Perception of self Interpersonal relationships Independent living skills (ADLs and iADLs) OT intervention in this phase typically involves relearning (remediating) and learning new ways to do things (compensatory strategies).
- 56. Tips for Providing Intervention Allow time for rest. Keep the environment and instructions simple. Set reasonable goals. Give feedback and redirect when necessary. Provide choices and vary activities. Remember: Many times patients do not remember the facts, but they remember how they felt!! An OT Intervention Session Recommended resource: http://tbirecovery.org/LongTermPhase.html
- 57. Ten Years Strong: Nate’s Journey After TBI
Editor's Notes
- Each year, TBI’s contribute to a substantial number of deaths and cases of permanent disability.
- There is a difference in prevalence of TBI in both categories of age and gender. Almost half a million ER visits for TBI are made annually by children aged 0 to 14 years in the U.S.
- https://bianys.org/resources/documentary-films/ (11 mins. long)
- The second category of ABI is NON-TRAUMATIC brain injuries, which are the result of non-violent causes.
- 3:20
- CNS handout—Brain Injury Reference Guide http://www.neuroskills.com/brain.shtml
- Aphasia - inability to comprehend and formulate language because of damage/dysfunction in specific brain regions (typically on left side of brain).
- https://youtu.be/X4fGlny5cPg
- ”- fewer spontaneous facial movements, spoke fewer words (left frontal lesions) or excessively (right frontal lesions).
- Test: Patient is told e.g. to pronate and supinate his hands in rapid succession, holding forearms vertically. In cerebellar diseases, the movements are irregular and inaccurate.
- Can be divided into two functional regions, one that’s involved with sensation and perception and the other that’s concerned with integrating sensory input, primarily with the visual system
- http://www.neuroskills.com/brain.shtml
- CNS handout—Brain Injury Reference Guide http://www.neuroskills.com/brain.shtml
- http://www.neuroskills.com/tbi/bcerebel.shtml http://www.neuroskills.com/brain.shtml
- Cerebellar injury results in movements that are slow and uncoordinated. Individuals with cerebellar lesions tend to sway and stagger when walking.
- http://www.neuroskills.com/tbi/bbstem.shtml
- CNS handout—Brain Injury Reference Guide http://www.neuroskills.com/brain.shtml
- In what age groups and in which gender are TBIs most often diagnosed? Which type/classification of TBI is most common overall? What’s the difference between a primary TBI and a secondary TBI?
- R&T p. 1046
- A person can go back and forth from decorticate to decerebrate, but eventually, if not treated promptly and things like intracranial pressure aren't stabilized, the patient will go all decerebrate and the outcome will be death.
- https://www.youtube.com/watch?v=aAvyVJ7SJZ8 https://youtu.be/lr8yMCAZKoI
- Video: https://youtu.be/hFVJlOCC-FU (9:14) Part 2 - https://youtu.be/vQyCamZbO0M (6:45)
- DISCUSS EMOTIONAL SIDE OF TBI – seen in interview with Tracy Morgan Pp. 1050-1051 (RT) Aimed at fostering alertness and goal-directed behavioral responsiveness Early rehab intervention – results in shorter acute care stays and higher Rancho levels at d/c CONTROVERSIAL: sensory stimulation programs for coma arousal. Insufficient evidence re: facilitation of alertness, but can be helpful in identifying emergence from coma by exposure to opportunities to respond to external stimuli
- See p. 1054 (RT) Intervention for people with continued cognitive impairment can focus on motor activities (esp. gross motor) with an automatic basis (playing catch). Over time, more refined motor skills are targeted and finally cognitive function. “Neuro Storms”
- https://www.aota.org/~/media/Corporate/Files/AboutOT/Professionals/WhatIsOT/RDP/Facts/Community%20Reintegration%20fact%20sheet.ashx Through guided, graded instruction within the context of the client’s community, occupational therapy practitioners may work with individuals in real life settings such as the grocery store, bank, mall, bus/train, workplace, home, or any other environment in which they need to regain competence in occupational performance.
- (p. 1051 – RT)
- https://youtu.be/RwoZhXyjBhs 6:33
