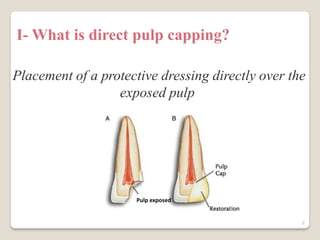
Direct pulp capping involves placing a protective material directly over an exposed dental pulp to encourage healing and formation of reparative dentin. It is a conservative treatment alternative to root canal therapy to save a tooth's vitality when the exposure is small. Success rates range widely from 13-98% depending on factors like the type of exposure, quality of the restoration, and operator skill. Calcium hydroxide and mineral trioxide aggregate are commonly used capping materials that induce healing, but newer options like Biodentine show promise as well. Future trends may involve techniques like lasers, gene therapy, or stem cells to further improve pulp capping outcomes.