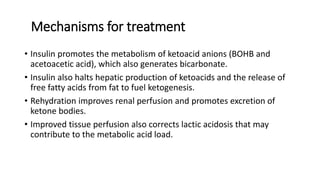
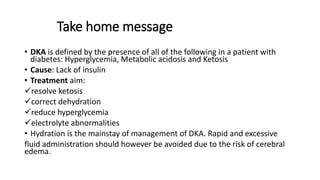
DKA is a life-threatening complication of diabetes that results from a lack of insulin. It is characterized by hyperglycemia, metabolic acidosis, and ketosis. The presented case involves a 9-year old patient with type 1 diabetes and DKA symptoms including drowsiness, abdominal pain, vomiting, and fruity breath odor. Treatment involves intravenous fluids to correct dehydration, insulin to resolve ketosis and lower blood glucose, and monitoring of electrolytes. Care must be taken to avoid complications of over- or under-hydration such as cerebral edema.












![Fluids therapy cont’d
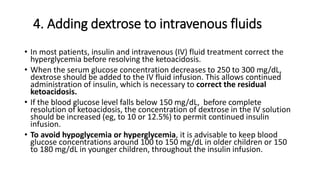
• Initial volume expansion of 10 to 20 mL/kg should be administered as
an IV bolus, using isotonic saline (0.9% normal saline]) or Ringer's
lactate in first 1-2 hrs
• If circulating volume is still compromised after the initial bolus is
complete, additional IV bolus infusions of 10 to 20 mL/kg can be
given
• Once the child is hemodynamically stable calculate fluids for
maintenance.
Dehydration should be corrected slowly to avoid cerebral edema](https://image.slidesharecdn.com/dka-191220033607/85/Dka-18-320.jpg)