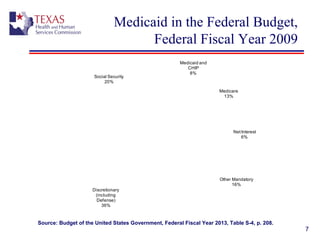
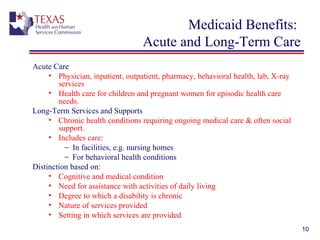
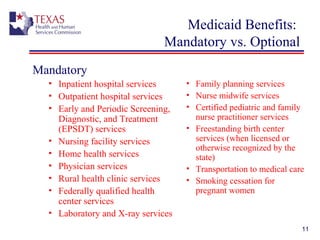
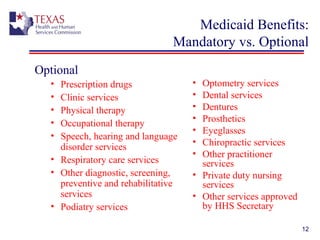
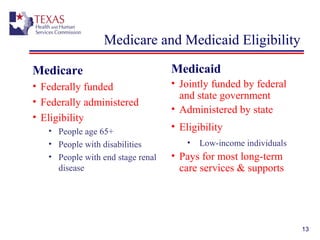
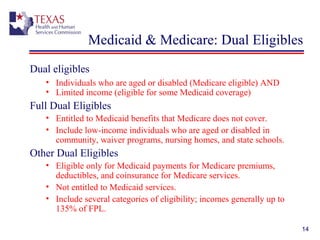
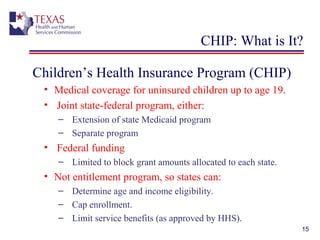
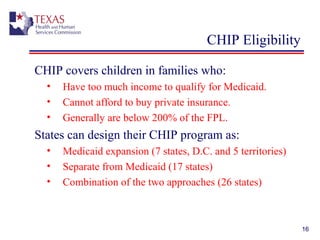
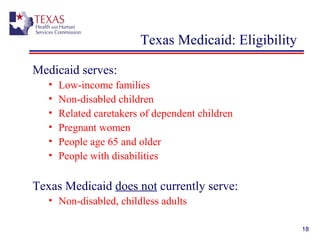
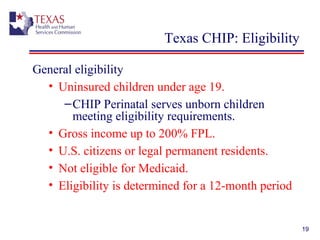
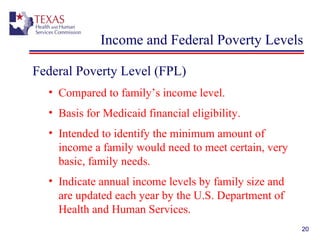
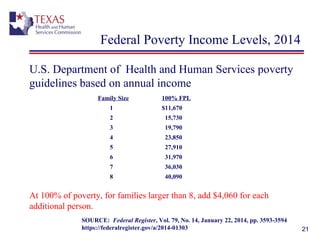
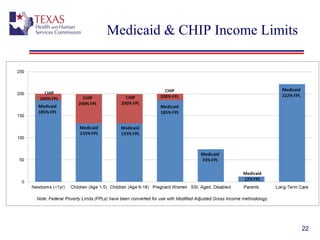
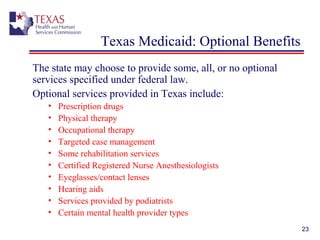
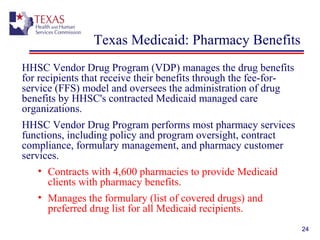
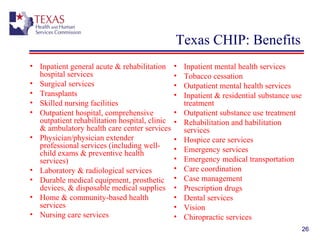
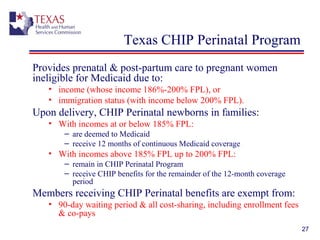
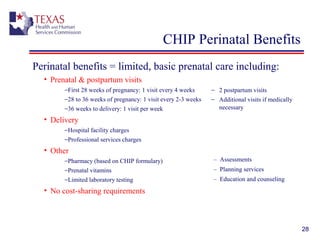
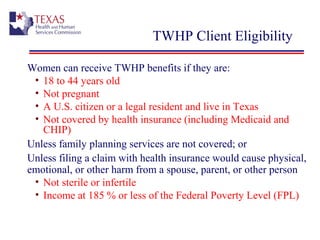
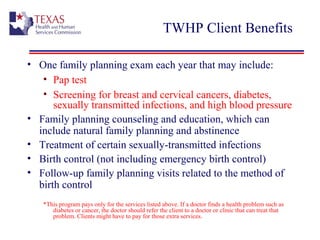
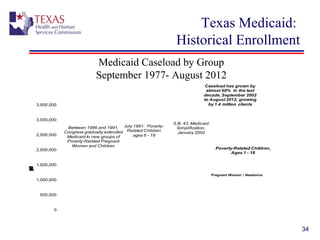
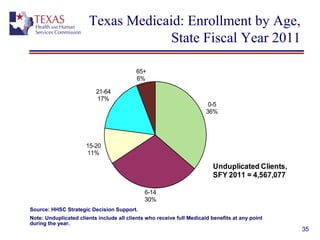
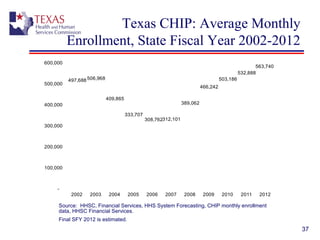
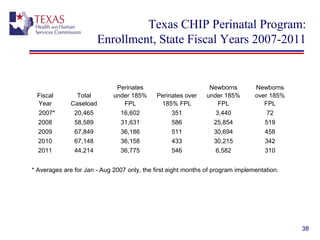
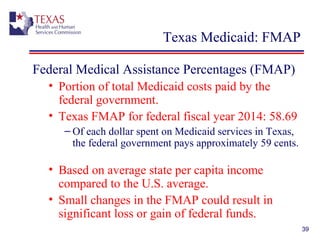
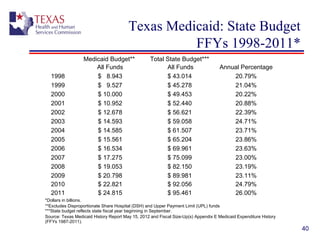
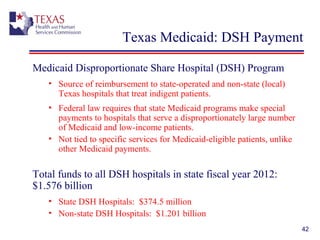
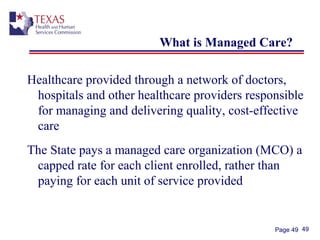
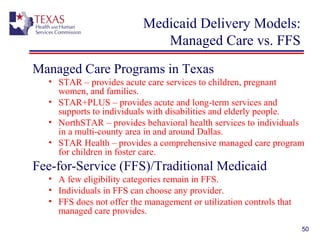
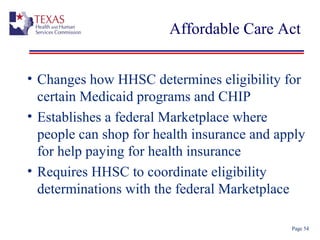
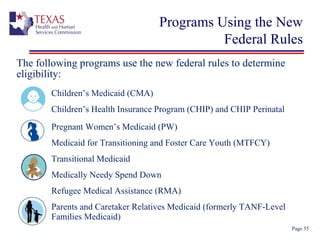
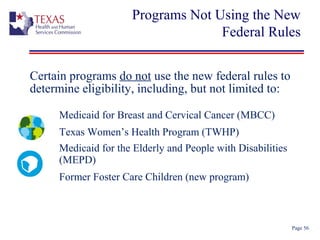
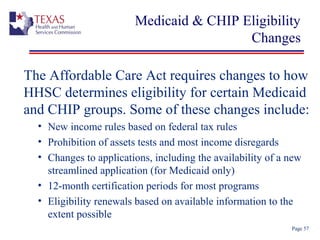
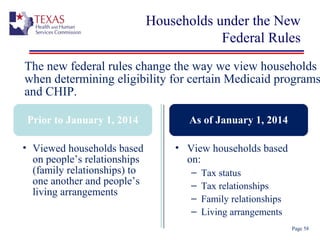
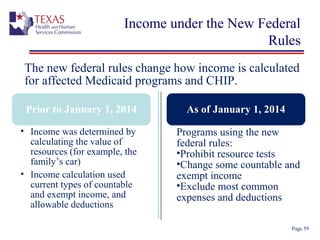
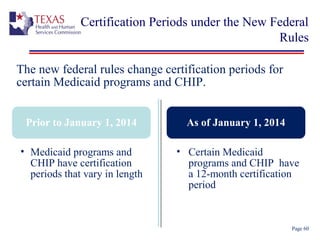
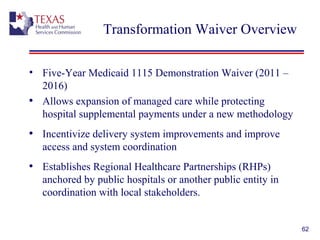
The document provides an overview of Texas Medicaid and CHIP, detailing eligibility, enrollment, and benefits for various populations including low-income families, children, and pregnant women. It discusses the federal and state administration of these programs, their funding, and the distinctions between mandatory and optional benefits. Additionally, it highlights current challenges and initiatives within Texas's Medicaid and CHIP frameworks.