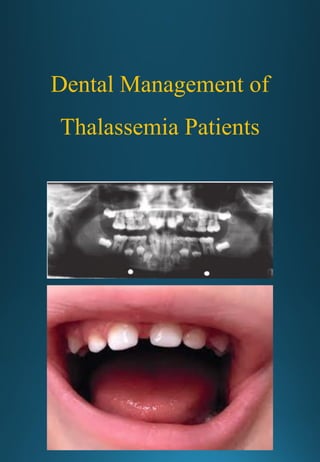
Dental Management of Thalassemia Patients
- 1. Dental Management of Thalassemia Patients
- 2. CLINICAL AND RADIOLOGICAL STUDY OF ORO-FACIAL MANIFESTATIONS IN THALASSAEMIA By Dr. SHILPA PATIL Dissertation submitted to the Rajiv Gandhi University of Health Sciences, Karnataka, Bangalore In partial fulfillment of the requirements for the degree of MASTER OF DENTAL SURGERY In ORAL MEDICINE AND RADIOLOGY Under the Guidance of Dr. ASHOK L. M.D.S. Professor and Head DEPARTMENT OF ORAL MEDICINE AND RADIOLOGY BAPUJI DENTAL COLLEGE AND HOSPITAL DAVANGERE, KARNATAKA, INDIA. March - 2006
- 3. i
- 4. ii
- 5. iii
- 6. iv
- 7. v ACKNOWLEDGEMENT My humble gratitude to the ALMIGHTY GOD, for the blessing showered upon me. People and events by their profound influence shape an individuals personality, life and career. It is indeed a privilege and pleasure to mention a few such names who have moulded me into what I am today. The individual most responsible for the completion of this study is my Guide and Professor Dr.ASHOK L., M.D.S., Professor and Head, Department of Oral Medicine and Radiology, Bapuji Dental College and Hospital, Davangere. His tireless pursuit for academic excellence and professional insight were a source of constant encouragement and inspiration. I will be indebted to him for his overwhelming help and kindness. To be like him one day will be an ongoing task. I would like to express my heartfelt gratitude and deep appreciation to my esteemed teachers Dr.RAJESHWARI A., Professor, Dr.SUJATHA G.P., Associate Professor, Dr.SHIVAPRASAD S., Associate Professor, Dr.ATUL P.S., Reader and Dr.SANJAY N.B., Reader, Department of Oral Medicine and Radiology, Bapuji Dental College and Hospital, Davangere. Their insistence on learning the basics, thinking logically and working systematically have spurred me to do the best that I could. I also extend my sincere thanks to Dr.NAGABUSHAN D, Dr.ANITHA, Dr.SHIVAKUMAR G.C., Assistant Professors, for their help in my hour of need and thoughtful suggestions. I express my sincere thanks to Dr.K. SADASHIVA SHETTY Principal, Bapuji Dental College Hospital, Davangere, for
- 8. vi providing excellent facilities to complete my post- graduation course. I am extremely grateful to my colleagues Dr.SARBJEET, Dr.CEENA, Dr.HEMA, Dr.GURU, Dr.SANGAMESH, Dr.SHRUTI, Dr.NAGARAJ, Dr. RANJANA, Dr.SHILPASHREE, Dr.SHILPA B.J., and Dr.VIJAYA LAKSHMI. I would like to express my regards and sense of indebtness to them because of their help, constructive comments, suggestions and support, this study has seen the light of this day. My sincere thanks to Mr.D.K.SANGAM, Bio-Statistician, for his service in carrying out the Statistical analysis. I would like to thank Mr. Surendra of DYNA COMPUTERS, for deciphering my writing and typing this thesis in time. I am thankful to Mrs.VANDANA, Mrs.CHANDRAMMA, Mr.HANUMANTHAPPA, Mr.BASAVANAGOWDA, Mr.SATISH & Mr.SHIVAKUMAR, for their help during the course of my study. Acknowledgement is also due to my cherished friends whose love, support and humour has indeed been life saving. My FATHER and MOTHER and my wonderful brother Dr.SANDEEP, have been a most important source of moral support, and have always been there when I needed them, I am forever indebted to them. My MOTHER-IN-LAW, SISTER-IN-LAW and my NIECES have been a constant source of encouragement. My bundle of joy my daughter TANISHKA who has given me so much at the time when she needed me the most. My friend and Companion Dr.ASHWIN who initiatives make me what I am today. I am indebted and incomplete without them.
- 9. vii Last but not the least I thank my PATIENTS for their kind co-operation inspite of their sufferings. Date : Place : Davangere. Dr. SHILPA PATIL LIST OF ABBREVIATIONS USED ALT Alanine Amine Transferase DMFT Decayed Missing Filled Teeth DNA Deoxy Ribonucleic Acid EMH Extra Medullary Hemopoiesis gm/dl Gram per deciliter GVHD Graft Versus Host Disease Hb Hemoglobin HbA Adult hemoglobin HbA2 Adult hemoglobin 2 HbF Fetal Hemoglobin HbH Hemoglobin H IgA Immunoglobin A IgG Immunoglobin G IgM Immunoglobin M IOPA Intraoral Periapical Radiograph MCH Mean corpuscle hemoglobin MCV Mean Corpuscles volume OHI-S Oral Health Index Score OPG Orthopantomograph RBC’s Red Blood Cells SNA Sella Nasion Point-A TM Thalassaemia major
- 10. viii WBC White Blood Count α Alpha β Beta β+ Reduced rate of β chain formation βo Complete absence of production of beta chains γ Gamma δ Delta
- 11. ix ABSTRACT Background & Objectives : Thalassaemias are the most common single gene disorder in the world and represent a major health burden. Oro-facial changes occur during the disease process mainly because of marrow expansion to compensate for anemia. The aim of this study was to evaluate the orofacial and radiological features in thalassaemia and to co-relate them to the duration of the disease process. To also find out if oro-facial manifestations could aid in early diagnosis and provide a clue to the progress of the disease. Methods : A group of 25 thalassaemia patients were evaluated for oral manifestations by clinical examination and with radiographs (IOPA radiograph, OPG and lateral cephalometric radiograph) for oro-facial changes. Lateral cephalometric radiographs were traced using Steiner’s analysis to check for maxillary prognathism. Results : 25 thalassaemia patients were in the age range of 3-28 years, with a male predominance of 44% and maximum cases were β-thalassaemia major (88%). 18 (72%) patients were poorly built and nourished. All the patients showed pallorness, icterus and frontal bossing with no changes in eyes, lips, parotid gland or on tongue. A mean dmft of 1.8 (±2.3) was recorded with a female predominance. Angle’s Class II molar relationship with increased overjet was present in 8% of cases. IOPA findings were one case showed thin lamina dura, 3 cases had short roots and all cases had enlarged marrow spaces. OPG showed altered trabeculae in 5 cases. Lateral cephalometric radiograph showed widened dipolic space in 4 cases, hair on end appearance in one case and maxillary prognathism in 3 cases with mean SNA angle 80.44o .
- 12. x Interpretation & Conclusion : The severity of the oro-facial changes depended on the age, duration of illness, time of transfusion and spleenectomy. Thus they can help to predict prognosis of the disease. Keywords : Thalassaemia ; Oro-facial manifestations ; Marrow spaces ; Pallor ; Steiner’s analysis ; OPG.
- 13. xi CONTENTS PAGE NO. 1. INTRODUCTION 01 2. AIMS AND OBJECTIVES 04 3. REVIEW OF LITERATURE 05 4. MATERIALS AND METHOD 65 5. RESULTS 83 6. DISCUSSION 95 7. CONCLUSION 105 8. SUMMARY 106 9. BIBLIOGRAPHY 108 10. ANNEXURES 119
- 14. xii LIST OF TABLES SL.NO. TITLE PAGE NO. Table 1 Age Range and Mean Age 87 Table 2 Male and Female Incidence 87 Table 3 Types of thalassaemia in the study 87 Table 4 General Physical Examination Findings 87 Table 5 Extra Oral Findings 88 Table 6 Intra Oral Findings 88 Table 7 DMFT Index 88 Table 8 Molar Relationship 89 Table 9 Anterior Incisor Relationship 89 Table 10 IOPA Findings 89 Table 11 OPG Findings 90 Table 12 Lateral Cephalograph Findings 90
- 15. xiii LIST OF GRAPHS SL.NO. TITLE PAGE NO. Graph 1 Graph Showing Sex Distribution 91 Graph 2 Graph Showing Type of Thalassaemia 91 Graph 3 Graph Showing Findings of General Physical Examination 92 Graph 4 Graph Showing DMFT Index 92 Graph 5 Graph Showing Molar Relationship 93 Graph 6 Graph Showing Anterior Teeth Relationship 93 Graph 7 Graph Showing IOPA Radiograph Findings 94 Graph 8 Graph Showing OPG Findings 94 Graph 9 Graph Showing Lateral Cephalograph Findings 94
- 16. xiv LIST OF PHOTOGRAPHS SL.NO. TITLE PAGE NO. Photograph 1 Armamentarium for Clinical Examination 77 Photograph 2 Armamentarium for IOPA Radiograph 77 Photograph 3 Armamentarium for OPG Radiograph 78 Photograph 4 Armamentarium for Lateral Cephalographic Projection 78 Photograph 5 Patient positioning for IOPA Radiograph 79 Photograph 6 Patient positioning for OPG 79 Photograph 7 Patient positioning for lateral cephalometric projection 80 Photograph 8 Chemicals for processing of radiographs 80 Photograph 9 Armamentarium for Lateral Cephalometric Radiograph Tracing 80 Photograph 10 Frontal view of the patient 81 Photograph 11 Lateral view of the patient 81 Photograph 12 IOPA of Control Subjects 81 Photograph 13 IOPA of Thalassaemia Patient 81 Photograph 14 OPG of the Thalassaemia patient 82 Photograph 15 Lateral cephalometric projection of thalassaemia patient 82 Photograph 16 Cephalometric Tracings on Acetate Sheet 82
- 17. 1 INTRODUCTION We are guilty of many errors and faults, but our worst crime is abandoning the children, neglecting the foundation of life. Many things we need can wait. The child cannot. Right now is the time her bones are being formed, her blood is being made and her senses are being developed. To her we cannot answer “Tomorrow”. Her name is “Today”. In this we have a crucial role to play. - Gabriela Mitral Tissue that connects and communicates is called connective tissue. One such connective tissue is blood. The formed elements of the blood and its liquid portion plays an extraordinary role in many physiologic mechanisms and processes in the human body. The alteration of cells, serum or other components is a result of a hereditary diathesis, nutritional deficiency or exposure to certain chemicals. Other times, a focal or disseminated infection or a defect in one of the elements causes the disturbance. When the disturbance of one of these constituents occurs, severe clinical manifestations result.1 The various blood diseases present polymorphic clinical expressions, one of which is the relatively constant involvement of oral structures. Oral manifestations of blood disorders are clinically similar to those lesions which occur in the oral cavity as a result of some local phenomenon, usually irritation or infection.1 Amongst various blood disorders Hereditary Hemolytic anaemias are of considerable complexity which encompass a variety of clinical manifestations ranging from benign conditions to complex disorders posing as public health problem.2 Hemolytic anaemias may be broadly classified depending upon whether the abnormality is within or outside the erythrocyte into two groups.3
- 18. 2 Extrinsic (extra corpuscular) hemolytic anaemias where the defect lies outside the RBC, are usually acquired. Intrinsic (intra corpuscular) hemolytic anaemias where the defect lies within RBC’s, can be either congenital or hereditary. Thalassaemias are a group of inherited pathologic conditions characterized by deficient synthesis of either α or β chains of globin in the adult hemoglobin molecule. Thalassaemias pose a challenging problem mainly due to variable phenotypes associated with these syndromes. Thalassaemias produce a wide variety of signs and symptoms and complications in those who inherit this disease. Clinicians may encounter patients with α or β thalassaemia in their clinical practice. They should be aware of possible oral manifestations of the condition, similarities to iron deficiency anemia, changes reflected in dental radiographs and possible complications as a result of the disease process or its treatment. The dentists recognition or suspicion of a possible blood dyscrasia maybe important from several different aspects4,5 : 1. The patient with such disease may be totally unaware of the condition, but comes to his Dentist for periodic care, whereas he may see his physician only sporadically. 2. The dentist is much more likely to take radiographs routinely than the physician. 3. The patient may be aware of some oral changes related to his disease and thus seek dental treatment. 4. The patient may be aware of his disease but still need routine or emergency dental care.
- 19. 3 5. The degree of cephalofacial deformities in this disease is closely related to the severity of the disease and the time of institution of therapy, thus provide a clue to the progress of disease. Several of these haemoglobin disorders have been reported from our population but the most prevalent seems to be the thalassaemias and to a lesser extent structural hemoglobinopathies.6 Various reports of population surveys and case reports from various parts of India prove that India is a rich reservoir of the Thalassaemia gene.7 Early literature has been extensively reviewed by various authors.8 From their review it can be inferred that the peculiarly heterogenous population divided into different endogenous groups, the origin and evolution of which are not traceable pose a difficult problem for the collection of data about these abnormal hemoglobins and as a result data in this country are inadequate. Taking the above aspects into consideration along with the available scattered Indian reports and the scarcity of available data in the Karnataka region, the present study is conducted to evaluate the oral manifestations in thalassaemia patients.
- 20. Aims & Objectives 4 AIMS AND OBJECTIVES AIMS : 1) To evaluate the oro-facial manifestations in thalassaemia. 2) To evaluate the radiographic features of oro-facial structures in thalassaemia. 3) To find out whether any co-relation exists between the duration of thalassaemia and severity of oro-facial clinical and radiological features. OBJECTIVES : 1) To find out if oro-facial manifestations could aid in early diagnosis. 2) To find out whether oro-facial clinical and radiological features could provide an indication to the progress of the disease.
- 21. Review of Literature 5 HISTORICAL REVIEW In 1889, Von Jaksch described an anemia accompanied by splenomegaly and leucocytosis which he thought was of specific nature and to which he gave the name “Anaemia infantum pseudoleucaemica”. This was subsequently called “Jaksch- Hayem-Luzet’s” anemia after the names of the authors who described it more fully.9 In 1925, Cooley TB and Lee P10 presented a brief report of five children with anemia of the type generally described by Von Jacksch (1889), but which they set apart because of peculiar mongoloid appearance caused by the enlargement of cranial and facial bones combined with clinical features. Cooley TB and Lee P (1923)9 were first to describe the typical mongoloid facies in Thalassemia. Rietti (1925)10 presented an account of primary hemolytic icterus.6 Cooley TB (1927, 1928)10 further refined his concepts of what he called erythroblastic anemia. Whipple and Bradford (1932)10 presented the first complete autopsy report of patient with Cooley’s anemia in which they called attention to excessive pigment deposition in many organs. They first suggested the term thalassemia. Lehndroff H. (1936),9 was the first to propose that the condition was not only familial, but inherited Caminopetros (1938)10 proposed that the disorder was transmitted as a mendelian recessive.
- 22. Review of Literature 6 Gatto (1942)10 and Valentine & Neel (1944)10 suggested a mode of genetic transmission of severe forms of Cooley’s anemia. Valentine and Neel (1944)10 proposed the terms “thalassemia major” and “thalassemia minor”. Angelini (1937)9 and Caminopetros (1938)9 proposed the existence of genetic carrier, as evidence by blood studies, fragility tests and mild roentgenographic changes. Caffey (1937)9 also had hypothesized that mild cases can reach adult life and transmit the disease. Thoma and Co-workers (1944) and Novak (1944)4 were among the first to report in the dental literature on the radiographic changes associated with thalassemia. Vecchio (1948)10 first described the presence of increased alkali resistant hemoglobin in patients with thalassemia and demonstrated increased fetal hemoglobin in thalassemia. Hamilton, et al (1950), Kalpan and Zuelzar, (1950)10 demonstrated that the erythrocytes of patients with thalassemia major and minor had a decreased survival time. Sturgeon, et al (1955)10 described intermediate types of thalassemia clinically. Kunkel and Wallenius (1955)10 described an increase in the percentage of A2 hemoglobin in thalassemia major.
- 23. Review of Literature 7 Sturgeon and Finch (1957)10 demonstrated that patients with thalassemia major, despite extreme erythroid hyperplasia of their bone marrow, were characterized by ineffective delivery of erythrocytes to the circulation Itano (1957)10 proposed thalassaemia may be caused by mutation interfering with normal globin synthesis. Sturgeon et al (1960)10 described α chain thalassaemia. In the past 20 years, the two important forms of thalassemia α and β Thalassemia have been recognized as the most common monogenic disease in humans. In recent years, the molecular biology and genetics of the thalassemia syndromes have be described, revealing the wide range of mutations encountered in each type of thalassemia. β thalassemia alone can arise from any of more than 150 mutations.
- 24. Review of Literature 8 DEFINITION S.F. Parkin (1968)11 defined thalassaemia as a hemolytic anemia, found typically in peoples of Mediterranean origin and due to a dominant Mendelian inherited abnormality of hemoglobin synthesis. The primary features of the disease are the continued production of fetal hemoglobin (Hb-F) and the formation of erythrocytes of aberrant structure which are low in hemoglobin content and which have a drastically reduced life span. Sandra F.Schnall and Edward J. Benz Jr. (2003)12 defined thalassaemia syndromes as heterogenous inherited disorders that arise from mutations in the globin genes that reduce or totally abolish synthesis of one or more of the globin chains. They result in hypochromia and microcytosis and in the more severe forms, anemia. As a group, they compromise the most single gene disorder. Jon Aster (2003)13 defined thalassaemias as a heterogenous group of genetic disorders of haemoglobin synthesis characterized by a lack of or decreased synthesis of globin chains.
- 25. Review of Literature 9 SYNONYMS The word thalassaemia is derived from thalassa, which in the Greek word for “Great sea”.11 Synonyms include Mediterranean anemia, Cooley’s anemia, hereditary heptocytosis and target-oval cells syndrome.11 In its homozygous form it goes by the names, Cooley’s anemia or thalassaemia major. Whereas in its heterozygous form it goes by the names, thalassemia minor or Rietti-Greppi-Micheli’s syndrome. Silverstonni and Bianco named it “Thalassaemia minima when this hematological anomaly does not entail any clinical manifestations.14
- 26. Review of Literature 10 EPIDEMIOLOGY Thalassaemia was first considered to affect people living in the central and eastern Mediterranean regions and those who had emigrated (Eg. North American) from these areas. Thus this disorder was considered to be frequently encountered in Italy, Sardinia, Sicily and Greece and elsewhere in Mediterranean islands. Later it came to be realized that thalassaemia was also to be found in many countries throughout the world – commonly in some, but less frequently in others – and to affect people of many races.15,16 α-thalassaemia are frequently seen in South East Asia, especially in Thailand. It occurs with varying frequency in India. β-thalassaemia is common in parts of India and Pakistan. β and α - thalassaemias, although found world wide, differ in their incidence. β-thalassaemia is particularly frequent in Italy, Sardinia and Sicily and in Greece. It occurs less frequently in Eastern Mediterranean, through middle east to Pakistan and India. Chatterjee (1959)17 reported an incidence of 3.7% for heterozygous β- thalassemia in the Bengalees in Calcutta. Labie et al (1961)18 reported a high incidence of 14% to 17% in Madras, South India. Haemoglobin D or HbD- Punjab is a β chain variant and was first reported from Poona in a Sikh soldier. Saha and Banerjee (1965)19 surveyed in Punjab and reported, a high incidence of heamoglobin-D in Sikhs.
- 27. Review of Literature 11 ETIOLOGY The etiology is obscure. It appears that both hereditary and inheritance are involved, to a varying extent, the trait can be transmitted by genes from either parents.11 Cooley, Witwer and Lee (1927)9 originally believed that the disorder was not primarily hemolytic but rather a disorder of hematopoiesis due to a metabolic fault which also affected bone maturation. Wipple and Bradford (1932)9 offered the possibility of an inherited metabolic disorder or a deficiency disease. They compared the lack of a vital factor to that found in pernicious anemia. Lehndorff (1936)9 suggested that the primary disturbance lay in a disturbed bone marrow, which because of some hereditary or “mutational” influence was creating defective red cells. Nittis and Spiliopulos (1936)9 suggested that Mediterranean anemia may be a peculiar form of malaria. Eight thalassemic children were treated with quinine. Within 3 months after treatment, all had improved clinically and hematologically. Caminopetros (1937)9 was of opinion that a coincidental malarial infection in Mediterranean anemia was effective in relieving many of the symptoms. Smith (1942)9 found no history of malaria in members of 16 families with thalassaemia whom he studied. Fawdry (1944)9 on the basis of his studies on conducted Greeks and on Cyprus, concluded that malaria played no part in the causation of disease.
- 28. Review of Literature 12 Damashek (1943)9 has suggested that a disturbance existed in the metabolism of hemoglobin, particularly in development of a normal amount in the cytoplasm of the nucleated red blood cells of the bone marrow. Cooley (1945)9 postulated either a primary progressive abnormality of the bone marrow or a hyperplasia due to long continued over stimulation. The fundamental defect lies obviously in the production of red blood cells. Valentine and Neel (1945)9 on the basis of their exhaustive original studies and analysis of the recorded cases, concluded that Mediterranean anemia is due, not to lack of extrinsic iron, but to an inherited inability of the body to utilize or synthesize some substance essential to normal erythropoiesis. This deficiency being quantitatively much greater in the fatal form of the disease than in the milder genetically related variety.
- 29. Review of Literature 13 PATHOPHYSIOLOGY OF THALASSEMIA Thalassemias are inherited disorders of Hb synthesis resulting from an alteration in the rate of globin chain production. A decrease in the rate of production of a certain globin chain(s) (alpha, beta, gamma and delta) impedes Hb synthesis and creates an imbalance with the other, normally produced globin chains. Since 2 types of chains pair with each other to form normal Hbs, an excess of the normally produced type is present and accumulates in the cell as an unstable product leading to the destruction of the cell. This imbalance is the hallmark of all forms of thalassemia.20 Bannerman Grioften and Moore (1959)21 were the first to report presence of a possible defect in heme synthesis in thalassemia. The type of thalassemia usually carries the name of the under produced chain(s). The reduction varies from a slight decrease to complete absence of production. For example, when β chains are produced at a lower rate, the thalassemia is termed β+, whereas β-0 thalassemia indicates a complete absence of production of beta chains from the involved allele.20 The consequences of impaired production of globin chains ultimately result in less Hb being deposited in each RBC, leading to hypochromasis. The Hb deficiency causes RBCs to be smaller, leading to the classic hypochromic and microcytic picture of thalassemia.20 In the most common type of β thalassemia trait, the level of HbA2 (delta2/Alpha2) usually is elevated. This is due to the increased utilization of delta chains by the excessive free α chains resulting from lack of adequate β chains with
- 30. Review of Literature 14 which to pair. The delta gene, unlike β and α genes, is known to have a physiologic limitation in its ability to produce adequate delta chains; by pairing with the α chains, delta chains produce Hb A2 (approximately 2.5-3% of the total Hb). Some but not all of the excessive α chains are used to form Hb A2 with the δ chains, while the remaining α chains precipitate in the cells, reacting with cell membranes, intervening with normal cell division, and acting as foreign bodies, leading to destruction of RBCs.20 In other types of β thalassemia traits, the mutation is not limited to the β gene but extends to the adjacent δ gene; thus, no elevation of Hb A2 is expected, and instead, γ chains are activated resulting in elevation of HbF. Less common are the types associated with elevation of both Hbs A2 and F. In the severe forms, such as β thalassemia major or Cooley’s anemia, the same pathophysiology applies with significant exaggeration. The significant excess of free α chains brought about by the deficiency of β chains causes destruction of the RBC precursors in the bone marrow. Cellular Pathophysiology : The consequences of accumulation of the excessive globin chains in the various types of thalassemia are quite different. In β thalassemia, excessive α chains, unable to form Hb tetramers, precipitate in the RBC precursors and, in one way or another, produce most of the manifestations encountered in all of the β thalassemia syndromes. This is not the situation in α thalassemia. The excessive chains in α thalassemia are γ chains earlier in life and β chains later on. Both are able to form homotetramers that, although relatively unstable, nevertheless remain viable and able
- 31. Review of Literature 15 to produce soluble Hb molecules such as Bart (4 γ chains) and H (4 β chains). These basic differences in the 2 main types of thalassemia are responsible for the major differences in their clinical manifestations and severity.20 Alpha chains accumulating in the red cell precursors are insoluble, precipitate in the cell, interact with the membrane (causing significant damage), and interfere with cell division. This leads to excessive intramedullary destruction of the red cell precursors. In addition, the surviving cells arriving in the peripheral blood with intracellular inclusion bodies (excess chains) are subject to hemolysis. This means that both hemolysis and ineffective erythropoiesis cause anemia in the patient with β Thalassemia. The ability of some red cells to maintain the production of γ chains, which are capable of pairing with some of the excessive α chains to produce HbF, is advantageous. Binding some of the excess α chains undoubtedly reduces the symptoms of the disease. Increased production of Hb F in response to severe anemia adds another mechanism to protect the RBCs in patients with β thalassemia. The elevated HbF increases oxygen affinity leading to hypoxia, which, together with the profound anemia, stimulates the production of erythropoietin. As a result, severe expansion of the ineffective erythroid mass leads to severe bone expansion and deformities. Both iron absorption and metabolic rate increase, adding more symptoms to the clinical and laboratory manifestations of the disease. The large numbers of abnormal red cells processed by the spleen, together with its hematopoietic response to the anemia if untreated, results in massive splenomegaly, leading to manifestations of hypersplenism.
- 32. Review of Literature 16 If one corrects the chronic anemia in these patients by giving regular blood transfusions, the severe expansion of the ineffective marrow is reversed. However, by doing so, another source of iron is added, which, together with the excessive iron absorption normally present in such patients, leads to a state of iron overload. Most nonheme iron in healthy individuals is bound tightly to its carrier protein, transferrin. In iron overload conditions, such as severe thalassemia, the transferrin becomes saturated, and free iron is found in the plasma. This iron is harmful since it provides the material for the production of hydroxyl radicals and additionally accumulates in various organs such as the heart, endocrine glands, and liver, resulting in significant damage to these organs. Certain modifiers may result in the development of milder types of thalassemia. Factors that may reduce the degree of globin chain imbalance are expected to modify the severity of the symptoms : co-inheritance of alpha thalassemia, the presence of higher HbF level, or the presence of a milder thalassemia mutation all typically ameliorate the symptoms of thalassemia.20
- 33. Review of Literature 17 CLASSIFICATION Sandra F.Schnall and Edward, Benz Jr. (2002).12 Classified thalassemia based on the globin chain involved into ; 1. α-Thalassemia - Reduced (α + Thalassemia) α globin synthesis - Absent (αo – Thalassemia) α globin synthesis 2. β-thalassemia - Reduced β globin (β+ -Thalasemia) synthesis - Absent β globin (βo – Thalassemia) synthesis 3. δ β - Thalassemia – Both δ and β globin synthesis are reduced or absent. 4. Hereditary persistence of fetal hemoglobin. In these conditions, synthesis of elevated amounts of fetal hemoglobin persists in adult life. Jon Aster (2003)13 gave clinical and genetic classification of thalassaemia. Clinical and Genetic Classification : Clinical Nomenclature Genotype Disease Molecular Genetics β-Thalassemias Thalassemia major Homozygous βo Thalassemia (β0 /βo ); homozygous β+ Thalassemia (β+ / β+ ) Severe, requires blood transfusions regularly Rare gene deletions in β0 /β0 Defects in transcription process, or translation of β- globin messenger RNA Thalassemia minor β0 / β Asymptomatic with mild or no anemia ; RBC abnormalities seen α-Thalassemia Silent Carrier α / αα Asymptomatic; No RBC abnormality α-thalassemia trait α / αα (Asian) ; - α / - α (black African) Asymptomatic ; like Thalassemia minor HbH disease - / - α Severe anemia tetramers of β-globin (HbH) formed in RBCs Hydrops fetalis - / - Lethal in utero Gene deletions mainly
- 34. Review of Literature 18 ALPHA THALASSAEMIAS Alpha thalassaemias are disorders in which there is a defective synthesis of alpha globin chains resulting in depressed production of haemoglobins that contain α chains i.e. HbA, HbA2 and HbF. The molecular defects underlying α thalassaemias are extremely heterogenous. α thalassaemias are categorized according to absence or presence of α globin gene production as ; Alpha-0 (αo ) Thalassemia-those with absent synthesis of α globin chains. Alpha-+ (α+ ) Thalassemia – Where there is reduced synthesis of α globin chains. They are further subdivided according to molecular defects into deletional and non-deletional types.22 There are normally four α-globin genes, the severity of the clinical syndromes shows a great variation, depending on the number of affected α-globin genes. The anemia stems both from lack of adequate hemoglobin and from the effects of excessive unpaired non-α chains (β, γ, δ). However, the situation is somewhat complicated by the fact that, normally different non α chains as synthesized at different times of development. Thus, in the newborn with α-thalassemia, there is an excess of unpaired γ-globin chains resulting in formation of γ4 –tetramers called Bart’s hemoglobin, whereas in adults, the excess of unpaired β-globin chains aggregate to from tetramers called hemoglobin H (HbH). Since the non-α chains in general form more soluble and less toxic aggregates than those derived from α-chains, the hemolytic anemia and ineffective erythropoiesis
- 35. Review of Literature 19 tend to be less severe than with β-thalassemias of similar degree of chain imbalance. A variety of molecular lesions have been detected in α-thalassemia. The most common cause of reduced α-chain synthesis seems to be the deletion of α-globin gene. Non deletional forms of alpha thalassaemia affect the alpha2 gene (α2).23 The gene is the dominant of the two alpha genes and the mutation of the α2 gene ultimately determine the phenotype of the disease, which is of more severe type when compared to the deletion mutants.22 It should be noted also that iron deficiency can induce a decrease in α globin synthesis that mimics the decrease that occurs in α thalassaemia.24 Clinical Phenotypes of Alpha Thalassaemia : The majority of normal individuals have 4 α globin genes (αα/αα) and 2% of population have 5 α globin genes (ααα /αα). Rarely individuals have 6 α globin genes (ααα/ααα) (αααα/αα), although the extra globin genes are functional these individuals are no different from normal.22 α Thalassemia syndromes are classified on the basis of the number and position of the α-globin genes deleted, which in turn determine the clinical syndrome. α-globin genes occur in linked pairs on each of the two chromosomes 16. Each α- globin gene normally contributes approximately 25% of the α-globin chains and may be deleted independently.
- 36. Review of Literature 20 Accordingly α thalassemias are22 ; 1. One α-gene deletion : Single carrier state. 2. Two gene deletion : α-thalassemia trait. 3. Three α-gene deletion : HbH disease 4. Four α gene deletion : Hb Bart’s hydrops foetalis. Single Carrier State : This condition results due to an absence or abnormality of one α gene. This is an asymptomatic condition difficult to diagnose and the diagnosis can be made only from family studies of HbH cases or by the direct study of number and structure of α genes.20 Some cases show a mild elevation of Hb barts in the range of (0.5 to 3%) at birth, but characteristic RBC inclusions cannot be demonstrated. In most cases Hb levels and RBC indices are within normal range. About 15% cases show slight reduction in the mean corpuscles volume (MCV) and mean corpuscle hemoglobin (MCH). Alpha Thalassemia Trait : In this condition there is lack of two alpha chain genes either on the same or on the opposite chromosomes.20 Affected individuals are asymptomatic and have normal or slightly reduced Hb levels, with low MCV and MCH and hypochromic red cells. About 4-8% Hb barts may be present at birth. When HbA2 levels are increased it is difficult to distinguish this condition from high HbA2 β-thalassemia trait25 and when HbA2 is decreased it may be difficult to distinguish it from iron deficiency anemia and sideroblastic anemias.26
- 37. Review of Literature 21 This is because a relative deficiency of α globin synthesis is also noted in iron deficiency and sideroblastic anemias. Hemoglobin H disease (HbH disease) : HbH disease is characterized by a chronic hemolytic anemia of variable severity and a clinical picture of thalassaemia intermedia.22 It results when the total output is equivalent to one functional alpha globin gene. It is seen most frequently in south east Asian and the Mediterranean regions where it results with the interaction of αo and α+ Thalassemia. It may also result from homozygosity for non deletional mutants affecting the dominant alpha2 globin gene.27 There seems to be a critical threshold of α chain output below which the syndrome of HbH results. HbH disease has also been described in individuals as an acquired defect with myeloproliferative disorders.28 It is also associated with mental retardation and other developmental disorders. Family studies show that neither of the parents are carriers and that atleast one chromosome usually number 16 in the HbH case had a denova mutation involving deletion of the entire α globin gene complex. HbH can be diagnosed at birth by the finding of 19-27% of Hb Barts in cord blood. But it usually diagnosed by the finding of 2-40% of HbH in peripheral blood of older children and adults.20 Hepatosplenomegaly is seen in 70-80% cases and Hb levels vary between 8- 11 g/dl, but may be as low as 3-4 g/dl. Peripheral smear study shows microcytosis, hypochromia as well as anisopoikilocytosis and target cells. Reticulocyte count is 4- 5%. In spleenectomized patients many red cells may contain one or more Heinz bodies.
- 38. Review of Literature 22 Hb Barts Hydrops Fetalis : Thein and Weatherall (1988)22 stated that this condition is almost exclusively seen in the South East Asia and Mediterranean countries. Where it was caused by the interaction of 2 α0 determinants resulting in complete absence of alpha globin synthesis. Hb barts hydrops fetalis is incompatible with extra uterine life. The pregnancy continues for 30 to 40 weeks and usually resulted in the still birth of the baby within an hour after birth.20 Affected babies are pale, oedematous, have ascites, pleural and pericardial effusions with spleenomegaly. Jaundice is not marked, there is presence of extra medullary haemopoiesis in the liver, spleen and other sites. The Hb ranges from 4-10g/dl and the blood film shows marked anisopoikilocytosis, microcytosis, hypochromia, erythroblastosis and reticulocytosis. Hb barts (γ4) constitutes 80-90% of the haemoglobin while 10% being embryonic Hb Portland and traces of HbH but no HbA. Oral Manifestations : Willaim N.A. and William A. Bechtold (1977)29 reported a case of α thalassaemia minor trait accompanied by clinical oral signs. They reported that the patient demonstrated anterior maxillary protrusion, splaying of the anterior teeth and severe generalized alveolar bone loss. In addition, there was an area of radiodensity in the mandible similar to that found in sickle-cell anaemia, and was considered to be an infarcted area of bone.
- 39. Review of Literature 23 ABSENCE OF ALL α-GLOBIN GENES30 Decreased Hb Most Hb made is 10-20% of Hb made Synthesis Hb Bart’s (γ4) Hb Portland ( γ2) Unstable and Unable to deliver Capable of O2 forms O2 to tissues delivery to precipitates tissues Shortened red Cell life span Keeps fetus alive Till the third Anemia Tissue hypoxia trimester Massively enlarged Heart failure Interferes with Extramedullary Placenta Organogenesis erythropoiesis and development Maternal complications Large Edema Congenital Large liver - Pre-eclampsia heart Ascites anomalies, Large spleen - Hypertension Pericardial Pleural including motor - Hemorrhage effusion effusion and cognitive - Retained placenta development
- 40. Review of Literature 24 BETA THALASSAEMIA INTERMEDIA CONCEPT : Thalassaemia intermedia is an ill-defined clinical term use to describe patients with phenotypes which are more severe than the usual asymptomatic thalassaemia trait, but milder than transfusion dependent thalassaemia major.31 It encompasses a wide spectrum from patients presenting after the age of two years and who are able to maintain a Haemoglobin level of 6 g/dl in childhood, without transfusion, to transfusion independancey in adult life, with Hb levels between of 10-12 g/dl. On the other hand, later on in life these patients are prone to develop iron over load and its complications despite, minimal blood transfusions.22 PATHOPHYSIOLOGY OF THAL INTERMEDIA : Weatherall and Clegg (1981)25 defined Βeta-thalassaemia intermedia as any patient with the Hb level persistently below 9-10 g/dl, particularly if there is associated splenomegaly. Many children go through life with these Hb levels but later on may require transfusions, specially following complication such as hypersplenism, or if the anaemia is worsened by folic acid deficiency, nutritional deficiency or recurrent infections. Therefore the same thalassaemia intermedia can cover a broad spectrum of conditions ranging from complete health with no requirements of transfusion to condition characterized by severe growth retardation and skeletal deformity requiring transfusions. The clinical and haematological manifestations of thalassaemia intermedia can be explained on the basis of the 3 chief causes as discussed earlier.
- 41. Review of Literature 25 1) There has been a mild defect in β globin chain synthesis which results in relatively little globin chain imbalance and hence a less severe disorder. This condition is characteristically seen in B+ homozygous Thalassemia of Negro variety. The genotype is mild homozygous B+ Thalassaemia (B+ /B+ ). 2) Co-inheritance of determinant for increased production of γ chains hence increased production of HbF associated usually with homozygous Bo - thalassaemia. 3) Co-inheritance of the genes for α thalassaemia which has been known to reduce the severity of the disorder, usually associated with homozygous B+ thalassaemia and to a lesser extent with B0 thalassaemia. The reason for the mild clinical picture in case of homozygous could be due to its ability to increase γ chain production sufficient enough to produce a mild intermediate form. This type of intermediate Bo thalassaemia seems to occur frequently in individuals of middle east and Indian background. It remains an enigma as to why patients with β-thalassaemia intermedia can maintain reasonable Hb levels while that counterparts with homozygous β-thalasaemia are not able to reasons could be ; 1) Presence of associated α thalassaemia gene which would reduce overall globin chain imbalance usually associated with the homozygous B+ thalassaemia. 2) Inheritance of two mild B+ thalassaemia genes one from each parent hence a milder degree of globin imbalance. 3) In cases where both parents have typical thalassaemia trait with no evidence of associated α thalassaemia and their off spring had mild Bo thalassaemia it
- 42. Review of Literature 26 could be an ability to synthesis more γ chains related to some defect which is not like the deletion observed in delta β-thalassaemia. 4) Double heterozygous conditions of β-thalassaemia with δ-β thalassaemia.32 Clinical Features of thalassaemia Intermedia : Clinical features of thalassaemia intermedia are extremely variable. It may present early in life with severe anaemia on one hand while it may not appear until later in life when complication such as hypersplenism develops growth and development maybe normal at one end of the spectrum or they maybe retardation of growth and severe clinical features as in homozygous β thalassaemia at the other end of the spectrum. Major symptoms in early childhood are anemia and mild jaundice. There is always some degree of hepatosplenomegaly, bone changes are variable and range from none to severe deformity, identical to that seen in β-homozygous thalassaemia. The course is that of a well compensated chronic anaemia, which may be exacerbated during period of infection, folate deficiency or hypersplenism. While patients usually require, no blood transfusions occasional transfusions may be required during periods of increasing anaemia. Haematology : Blood Picture : There is a variable degree of anaemia with Hb levels in the range of 5 to 10 gms/dl. Red cells are typically thalassaemia, MCh and MCH are low, peripheral smear shows moderate to marked abnormalities in shape and size of RBCs. Reticulocyte counts are also elevated.
- 43. Review of Literature 27 Oral Manifestations : Ficarra et al (1987)5 reported a case of Thalassemia intermedia in which the oro-facial deformities was the first sign of the disease, which prompted the consultation. A 10 year old black girl visited her dentist for facial lineaments, large maxillary bones. The OPG demonstrated ground glass appearance of maxilla and mandible with obliteration of the maxillary sinuses. Subsequent skull radiographs displayed sinus obliteration and parietal, frontal and occipital thickening. He also discussed the other oral manifestations like Mongoloid features caused by prominence of cheek bone, protrusion or flaring of maxillary anterior teeth and depression of nose. The oral mucosa exhibited the characteristic anaemic pallor. Radiographic features in skull were characteristic thickening of the dipole and elongated trabeculae, giving a hair-on-end appearance, thinning of lamina dura and circular radiolucencies in the alveolar site of mandibular bone. In general the jaws exhibited mild osteoporosis with a peculiar trabecular pattern of the maxilla and mandible was evident characterized by an apparent coarsening of some trabeculae and disappearance of others resulting in a “salt and pepper effect”. Thus they concluded that degree of cephalofacial deformities in this disease was closely related to the severity of the disease and the time of institution of therapy.
- 44. Review of Literature 28 β-THALASSAEMIAS MAJOR AND MINOR The β thalassaemias result from over 150 different mutations of the β-globin genes that result either in the absence of the β globin chains (βo thalassaemia / β- thalassemia major) or a reduction in their output (β+ thalassaemia / β- thalassaemia minor).33 Since β chain synthesis replaces γ chain synthesis during the first few months of life it might be expected that β thalassaemia would manifest at about that time. The disease commonly presents within the first year of life.25 Symptomatology : Clinical manifestations appear insidiously. Clinical features may be attributable due to ; o Severe anemia o Blood transfusion Frequently, affected infants fail to thrive or gain weight. They show progressive pallor, feeding problems, diahorrea, irritability, recurrent bouts of fever and progressive enlargement of the abdomen due to hepatosplenomegaly. If an accurate diagnosis is made at this stage and the infant started on a regular blood transfusion, morbidity may be reduced. However if the child is not adequately transfused the typical picture of homozygous thalassaemia develops in the next few years. Modell (1976)34 and Costin G, Kogot MD et al (1979)35 explained that the child who is not transfused fails to thrive and shows growth retardation early in life, in
- 45. Review of Literature 29 association with severe anemia and hypersplenism. He also shows poor musculature, reduction of body fat, poor appetite and lethargy. On the other hand, growth retardation yet persists inspite of high transfusion regimes and this was manifested initially as failure or reduction in the pubertal growth spurt. Improvement in growth and height with regular transfusions have been reported by some workers34,36 but disapproved by others.37 Splenomegaly is one of the most constant findings in homozygous β thalassemia. Progressive enlargement of the spleen in an untransfused or poorly transfused child is the rule. However, there is evidence that children maintained on high transfusion regime develop less marked spleenomegaly.34 Hyperspleenism may produce numerous complications including RBC sequestration, shortening of the autologous RBC survival and a striking expansion of the total blood volume. Pancytopenia, thrombocytopenia and purpura with bleeding are rare but well recognized complications of hyperspleenism seen in under transfused or un-transfused β- thalassemia cases.38 Smith CH, Erlandson ME et al (1964)39 were the first to notice that spleenectomy in a young thalassaemic patient was followed by increased incidence of severe infections. Most common being pneumococcal or streptococcal. The highest incidence being in the first few years. Skeletal changes are one of the predominant features observed in untransfused children. Characteristic findings were bossing of the parietal and frontal bones, protrusion of maxilla and prominent malar eminences with depression of the bridge of
- 46. Review of Literature 30 nose and puffiness of the eyelids which gives an appearance of typical thalassaemic facies. There is also a tendency to a mongoloid slant of eyes.34,35 Magli A, Fuslo R, et al (1982)14 reported the 33.3% ocular manifestations in 96 thalasemic minor patients. 14 patients showed colour alterations and 6 of them presented alternations of static perimetry as well. They concluded that those changes were due to bad oxygen perfusion of the retinal receptive units. In older children, iron over loading has been recognized as a complication of thalassemia for many years. The excess of iron of more than 28 gms, will result in overt symptoms34 and this is characteristically seen in children on high transfusion regimes, usually by the age of 11 years. Iron overloading affects many systems chiefly – cardiac, hepatic and endocrine. Inadequately transfused children show cardiac dysfunction. It presents as cardiomegaly or as sudden death or congestive cardiac failure.40 Endocrine dysfunction is due to wide spread haemosiderosis secondary to iron overload and causes diabetes mellitus. This is seen in the second decade. Failure or delay of puberty is well documented and presents as the first symptom in a well transfused homozygous patient. This is due to iron overloading which invades either pituitary or Gonads.34 Transfusion has changed the pattern of the disease and most children treated in this manner may survive towards the end of the 2nd decade. Modell CB (1976)34 suggested the following prognostic pattern. : Deaths in childhood or early in second decade result from inadequate transfusion leading to severe anemia, infections and complications of
- 47. Review of Literature 31 hyperspleenism such as thrombocytopenia and bleeding from other recurrent illness. Deaths in the 2nd and 3rd decade results from iron overload involving particularly myocardium. Transfusion dependent thalassaemics are unlikely to survive much beyond the third decade, although recent advances in iron chealating therapy may make it possible to reduce the effects of iron loading and hence a longer survival. Fucharoen S, Ketrichit P, et al (2000)41 reviewed the clinical manifestations of 378 β thalassemic patients by retrospective analysis. Most patients showed clinical symptoms by 10 years of age. The majority of patients survive with or without occasional transfusion. Spleenectomy was performed in 26.5% of patients. Patients came to the hospital because of anemia, fever, abdominal mass and jaundice. Gastrointestinal tract disturbances were the most common presenting symptoms (34.6%), especially abdominal pain (10%) and cholecystitis (5.1%), respiratory tract infection were found in 21.8% of patients and cardiovascular complications including congestive heart failure, occurred in 11.9%. Other less common symptoms and complications included bone pain, chronic leg ulcers, paraplegia and hypertension – associated convulsions and cerebral hemorrhage after multiple blood transfusion. Patients usually died between 20 to 40 years of age (6%), mainly from CCF and Septicemia.
- 48. Review of Literature 32 OROFACIAL MANIFESTATIONS OF β THALASSEMIAS MAJOR AND MINOR The oro-facial manifestations of β-thalassemia are numerous and intense and are the result of bony changes occurring due to ineffective erythropoiesis, with formation of a bone expanding erythroid mass.42 The oral manifestations are more pronounced in thalassemia than in other dyscrasias of hemoglobin.43 If the abnormality has been present for a sufficient period of time, the facies may assume a somewhat mongoloid appearance owing to maxillary, and in particular premaxillary remodeling as a result of reactive marrow hyperplasia. This phenomenon does not occur in association with other hemoglobinopathies.43 Kalpan RI, Werther R et al (1964)44 commented that most noticeable changes that took place in the oral structures are associated with maxillary enlargement. The maxilla is mainly composed of cancellous bone containing marrow spaces, which was a part of hematopoietic system. Under the influence of the disorder these spaces and the entire maxilla go through a progressive enlargement producing the typical facial appearance, with high bulging cheek bones, retraction of the upper lip, protrusion of the anterior teeth, spacing between the teeth, increased overbite or open bite and varying degree of malocclusion. In severe cases, the maxillary tuberosity areas became widened and bulbous. The dentofacial appearance has been described as having a more of a “rodent” than a Mongoloid” cast.
- 49. Review of Literature 33 Baty JM, Blackfan KD et al (1932)44 commented that the patient with Thalassemia major resembled each other than they resemble the other members of their own families. The mandible ordinarily undergoes less enlargement than the maxilla. Jan Hess et al (1990)46 quoted that, in mandible marrow enlargement was less pronounced because of the dense cortical plates of mandible which prevented the expansion. Kaplan RI, Werther R et al (1964)44 described that oral mucosa displayed a characteristic pallor in Thalassemia major. The gingival tissues appeared thin and pale but are often otherwise normal. The incidence of gingivitis in children with the disease seems likely related to local factors such as poor oral hygiene, malocclusion and drying of the gingiva through the patient’s inability to close his mouth over the protruding teeth. The chronic anoxemia may in some cases predispose to gingival disorders. Kaplan RI, Werther R et al (1964)44 reviewed 50 patients with Cooley’s anemia to study dental and oral findings. They found maxillary enlargement in 32 (64%), 18 (36%) had deep overbite, 15 (30%) showed an open bite condition and 4 (8%) had some degree of cross bite, 25 (50%) showed more than one dentofacial deformity and 10 (20%) had apparently normal occlusion. The soft tissue changes included some degree of gingival inflammation in 16 (32%), 5 (10%) had one or more periodontal pockets, 5 (10%) showed supra and subgingival calculus and 2 (4%) showed only supragingival calculus. The author thought that gingival inflammation was not related to disease process.
- 50. Review of Literature 34 Johnston and Krogman (1964)47 studied the growth of face in 50 thalassemic major patients ranging from 2 years 10 months to 28 years 5 months. They concluded that children with Cooley’s anemia had their growth patterns altered in two ways, a retardation in their normal growth expectations and a retardation in their rates of growth. Cephalofacial manifestations of orthodontic significance was considered to be concentrated mainly in maxillary alveolar bone and in the palate. Parkin SF (1968)11 reviewed 5 cases of thalasssemia and remarked that they all had a characteristic facial appearance, with a broad base to the nose and a marked enlargement of the zygomatic and maxillary parts of the face. He described the child as “a child wearing grandama’s upper full dentures. The occlusal plane was much lower than usual in both deciduous and permanent dentitions, with increased overbite and overjet. There was a tendency toward buccal occlusion of maxillary teeth in the posterior segments. The teeth had a yellowish tinge, probably tetracyclins may have been administered at times to deal with recurrent infection. Willian NA, Richard L, et al (1980)48 reported a case of β Thalassemia minor with a rare combination with cleidocranial dysplasia in a 10 year old patient. Goldfaub A, Nitzna DW, et al (1983)49 reported two cases of β Thalassemia major who presented with pain and swelling of the parotid salivary gland. It was postulated that the impaired function of parotid gland was linked to iron deposits in the serous cells of this gland, which was particularly susceptible to iron damage, as demonstrated by low isotope incorporation as in scintigraphic imaging. Margot LVD, Robert PL (1986)50 reported a case of Thalassemia minor with glossodynia, depapillation of tongue and with median rhomboid glossitis with
- 51. Review of Literature 35 contact lesions on the palate and palatal petechiae with superimposed candidal infection. He also considered the risk factors of bacteremia and viral hepatitis in those patients. Weel F, Jackson IT, et al (1987)51 described a case of thalassemia major with gross dental and jaw deformities, who was operated to achieve a satisfactory aesthetic and functional result. Cannell H (1988)52 discussed the development of oral and facial signs in β- thalassaemia major like retraction of the upper lip, spacing and protrusion of the upper labial segment, anterior open bite and generalized maxillary enlargement. He reported a case of β thalassaemia major in a 26 year old man with corrugated maxillary alveolus. This sign warned of serious decline in the patient’s condition. The corrugations appeared to be a stage in the development of the well recognized “chipmunk facies”. Lamabadusuriya SP (1989)53 described a case of β thalasaemia major in a 11 year old Sinhalese girl who developed a lower motor neuron facial nerve palsy on the left side, together with a phernic nerve palsy, on the same side, during the course of the illness. Author attributes the cause of facial palsy as pinching of nerve at one of the narrow points along its course, such as within the facial canals, due to widening of diploe bone. The reason for phrenic nerve palsy was postulated as due to pressure from a small paravertebral mass of haematopoietic tissue. Jan Hess, Isaac Van Der Waal et al (1990)46 emphasized on the typical facial expression of thalassemic patients. he discussed the possibility of surgical treatment of the maxillary hypertrophy. However he concluded that in view of the
- 52. Review of Literature 36 limited life expectancy of these patients correction should not be performed before adolescence. Bucci E, Lo Muzio L, et al (1990)54 reported the findings of a study on 46 subjects affected by β-thalassaemia major who underwent periodic transfusion therapy. A reduced incidence of the caries process was observed, in all subjects treated from the first months of life. After a short review of the main problems posed by these patients during dental treatment, the authors propose a course of preventive antibiotic treatment to be carried out before the start of dental work. Siamopoulou-Mavridou A, Mavridis A, et al (1992)55 evaluated flow rates and chemistry of parotid saliva to dental caries and gingivitis in thalassemia major patients. Twenty one child patients with thalassaemic major (TM) and 83 healthy control children were examined for dental caries and gingivitis. Stimulated parotid saliva flow rates was measured and the saliva samples were tested for calcium, phosphorus, potassium, sodium, urea, lysozyme and immunoglobulin levels IgA, IgG, and IgM. The results showed that dental caries experience was significantly higher in the TM group. Parotid salivary flow rates in TM patients was not significantly different from those in the healthy controls. However the median saliva concentrations of phosphorus and IgA were significantly lower in the patients than in the controls. The concentration of lysozyme was also lower in the TM group, but the difference was not statistically significant. The findings could provide an explanation for the higher dental caries experience and gingivitis observed in the TM group. Scutellari PN, Orzincolo C, et al (1994)56 reviewed fifty four homozygous β thalassemic patients (26 men and 28 women) aged 7 to 24 years, who had been treated with high transfusion regimen (Hb levels = 9-10 g/dl) and chelation therapy
- 53. Review of Literature 37 (desferrioxamine, 35-50 mg/kg), underwent clinical and radiographic investigations. Their study was aimed at assessing the clinical and radiographic changes in the stomatognathic system (teeth, mandible and maxilla, occlusion relationship and dental bases). All patients underwent orhtopantomography and teleradiography of the skull. Twenty thalassemic patients (13 men and 7 women) of the same age but treated with low transfusion regimes (Hb levels = 5-6 g/dl) were examined as a control group. Results indicated that ; 1) in the control group, osteopenia was observed in both the alveolar process and the mandible, following marrow expansion, with diastema of incisors and several types of malocclusion nearly all of them associated with Angle’s Class II pattern 2) In adequately transfused patients, no lesions were observed in 55% of cases, which meant that current treatment methods can prevent bone abnormalities, especially if transfusions begin at birth. Nevertheless, osteopenia of the mandible (31.4%) and dental and/or skeletal malocclusions (40.7%) remained in many cases, because of persistent marrow expansion, which usually follows incorrect treatment. 3) General dental diseases – eg. caries, gingivitis, etc – affect both populations with the same incidence. Mason C, Porter SR, et al (1995)57 conducted a retrospective study to note the prevalence of clinically significant anemia and haemoglobinopathy in children requiring dental treatment under general anaesthesia in 1000 patients having low hemoglobin. 11 patients had sickle cell trait and 2 had β-Thalassemia trait. They concluded that pre-anesthetic haematological assessment of children needing minor dental surgery is rarely of any significant clinical value. Bassimitci S, Emel Yucel-Eroglu et al (1996)58 studied the effects of thalassaemia major on components of the craniofacial complex using cephalometric
- 54. Review of Literature 38 analysis of two samples consisting of 30 thalassaemic patients and 30 controls. Differences between the groups were tested by variance analysis. It was found that thalassaemia major had significant effects on components of the craniofacial complex. The typical thalassaemia patients had a moderate class II skeletal discrepancy with prounced vertical mandibular growth direction, prominent mandibular incisors, everted lips and a narrowed nasal cavity. Gotte P, Consolo U, et al (2001)59 evaluated the feasibility of orthodontic and maxillofacial surgical corrective treatment associated with an appropriate transfusion therapy in a β-thalassemic patient. They treated a patient who received a combined haematological, orthodontic and maxillofacial surgical treatment. Controls for evaluating the statement of results obtained were performed at different times after the end of the therapy and have shown that the therapeutic objectives had been achieved and maintained. Their results suggested that this facial disfigurement requires surgical and orthodontic correction by consolidated surgical-orthodontic techniques performed according to the appropriate anaemia therapy. Motalebnejad M, Jenabian N, et al (2002)60 reviewed the relationship of gingivitis and salivary immunoglobulins in 55 patients with thalassemia major. The results showed no significant difference between the rate of IgA, IgG and IgM in two groups. Also there was no relationship between severity of gingivitis and rate of salivary immunoglobulins. Abu Alhaija Es, Al-Wahadni AM, et al (2002)61 investigated cephalometrically the uvulo-glosso-pharyngeal dimensions in 15 subjects with β- thalassaemia major. The study group comprised of 8 males and 7 females with a mean age of 14.13 ± 1.06 years. The variables measured on the lateral cephalograms
- 55. Review of Literature 39 were tongue height and length, soft palate length and thickness, superior, middle and inferior pharyngeal airway space, and hyoid bone position. The thalassaemic group was compared with a normal control group matched for age and sex using a t-test. The results showed that thalassaemic patients had a smaller tongue size (length P<0.05, height P<0.001), shorter soft palate (p<0.001), smaller upper (p<0.001) and middle (p<0.05) pharyngeal airway spaces, and a shorter vertical pharyngeal length (p<0.05). The hyoid bone in thalassaemic patients was closer to the mandibular plane (p<0.001). Al-Wahadni AM, Taani DQ, et al (2002)62 conducted a study to determine whether β-thalassemia major is associated with an increase in the severity of periodontal disease and dental caries in 61 thalassemia patients. They were compared with 63 healthy controls for gingival index, probing pocket depth and DMFT. Thus, they concluded from their results that thalassaemia is not associated with increased levels of gingivitis or periodontitis. But is associated with higher dental caries experience Elham SJA, Hattab FN et al (2002)63 studied cephalometric measurements and facial deformities is 54 (24 M, 13 F) thalassaemic patients with mean age of 7.5 and compared with age and sex matched controls. The authors concluded that a Class II skeletal pattern short cranial base length, short mandible, increased anterior and reduced post vertical dimensions and severe facial disfigurement in 17% of patients was noted. Luglie PF, Campus G, et al (2002)64 carried out the investigation to determine the oral status in a group of 18 (15 males ; 3 females) patients with thalassaemia major (TM) with 18 healthy controls using the decayed, missing, and
- 56. Review of Literature 40 filled teeth (DMFT) index and the oral hygiene index (OHI)-S. Spontaneous saliva was collected from each subject, and the biochemical composition (calcium, phosphorous, potassium, sodium, urea) were determined and salivary Streptococcus mutans levels were evaluated. Dental status (DMFT index) was almost equal in the two groups (10.3 in TM vs 9.4 in controls, p=0.34). The occurrence of plaque (OHI-S 2) was higher in the control group, but no statistically significant association was observed between oral hygiene conditions in the two groups (Fisher’s exact test 0.47, p=0.79). Biochemical saliva composition was very similar in the two groups; only the urea concentration was lower in TM, and this difference was statistically significant (p=0.002). The TM patients had an increased presence of mutans streptococci at detectable levels. Their findings confirmed that, although no substantial differences were found between the two observed groups, further investigations are needed to determine the theoretical risk of oral diseases in thalassemic patients. Piras V, Tuveri F, et al (2003)65 suggested that the type of malocclusion most often seen in β thalassemic patients was represented by Angle’s class II, they evaluated the influence of other factors on malocclusion particularly sexual development, the level of serum ferritin, ALT, and age at first transfusion. 122 β- thalassemic patients and 39 homozygotes, (Age 16-27 years), undergoing treatment have been analysed. The results of the statistical analysis showed that hypogonadism can play an important role in determining malocclusions in male β thalassemic patients (Odds ratio 4, 5; CI 1, 5-13). No other factor has shown any statistically relevant influence on dental occlusion. They concluded, it would therefore be interesting to further investigate the hormonal mechanisms that can alter bone development in thalassemic youngsters; the prevention of such alterations will surely contribute to improving the quality of life in these patients, particularly now that their
- 57. Review of Literature 41 life expectancy has been significantly extended by the progress made in transfusional therapy and ferrochelation. Al-Wahadni A, Qudeimat MA, et al (2005)66 examined the arch dimensions of Jordanian patients with β-thalassemia major in comparison with an unaffected control group. The sample consisted of 24 patients who suffered from beta- thalassaemia major (mean age = 13.9 ± 3.1 years) and an unaffected 24 control group (mean age = 13.5 ± 2.9 years) matched for dental age, sex, and incisor and molar relationships. Alginate impressions of the maxillary and mandibular dental arches of all participants were taken. All measurements of the arch dimension were made on the casts using an electronic digital sliding caliper. In the mandibular arch, when compared with the patients with thalassaemia, the unaffected control group subjects showed a (statistically) significantly larger incisor width, larger arch depth, and larger left and right anterior arch lengths (1.18, 2.58, and 1.85 and 1.12 mm, respectively). In the maxillary arch, there was a statistically significant difference in the mean incisor width (±2.16 mm), arch depth (±3.14 mm), inter molar width (±121 mm) and in the left anterior arch length (±1.97). The canine widths, premolar widths, left and right posterior arch length, and curve of Spee of both arches showed no statistically significant differences between the two groups. The authors concluded patients with β-thalassaemia major exhibited; a narrower maxilla; a shorter maxilla and mandible and smaller incisor widths for the maxillary and mandibular arches when compared to unaffected subjects.
- 58. Review of Literature 42 CARIES RISK IN THALASSAEMIA PATIENTS Ventura (1955)67 theorized that the endocrine dysfunction caused by thalassaemia is responsible for increased dental caries prevalence. Kaplan RI, Werther R, et al (1964)44 in their DMF study in 50 β thalassaemia major patients found that there was a total of 110 carious primary teeth (average 2.2 per patient), 125 carious permanent teeth (average 2.5), 25 missing permanent teeth (average 0.5), 38 filled primary teeth (0.75 average) and 126 filled permanent teeth (average 2.5 per patient). There was also 10 patients (20%) who showed teeth in perfect condition with no carious areas and no restorations. The overall DMF rate was 8.3 per patient which was compared to DMF rate of 7.0 per child in control group. The authors concluded that dental caries in these patients appeared to be associated primarily with dental neglect. The parents are more concerned with the serious physical problems, paying less attention to the dental ailments and only seek dental care when the child is in pain. Bucci E, Lo Muzio L, et al (1990)54 reported the findings of a study of 46 subjects affected by β-thalassaemia major who underwent periodic transfusion therapy. A DMFT rate of 4.70 for males and 5.90 for females was observed the authors concluded that, reduced incidence of the caries process was seen in subjects treated from the first months of life. After a short review of the main problems posed by these patients during dental treatment, the authors propose a course of preventive antibiotic treatment to be carried out before the start of dental work.
- 59. Review of Literature 43 Leonardi R, Verzi P, et al (1990)68 stated that mean DMFT values for thalassaemic males and females were as low as 1.5 and 1.6 respectively. They also found that 90% of males and 66% of females were affected by caries. Siamopoulou-Mavridou A, Mavridis A, et al (1992)55 evaluated flow rates and chemistry of parotid saliva to dental caries and gingivitis in thalassemia major patients. 21 children with thalassaemic major (TM) and 83 healthy control children were examined for dental caries. Stimulated parotid saliva flow rates were measured and the saliva samples were tested for calcium, phosphorus, potassium, sodium, urea, lysozyme and immunoglobulin levels (IgA, IgG, IgM). The results showed that dental caries experience was significantly higher in the TM group. Parotid saliva flow rates in TM patients were not significantly different from those in the healthy controls. However the median saliva concentrations of phosphorus and IgA were significantly lower in the patients than in the controls. The concentration of lysozyme was also lower in the TM group, but the difference was not statistically significant. The findings could provide an explanation for the higher dental caries experience and gingivitis observed in the TM group. DeMattia D, Pettini PL, et al (1996)69 evaluated the oro-maxillofacial alterations and correlating them to transfusion indexes, serum ferritin levels, splenectomy and age in 60 thalassaemia major patients. The caries index (DMF) for the permanent teeth in 60 subjects was 5.12 ± 4.76. By utilizing Spearman’s rank test the number of teeth with caries in the permanent dentition (DMF) and in the mixed dentition (DMF + dmf) was correlated to the average value of ferritin, with the ferritin peak, with transfusion requirements and with the age of the patient at the date of the clinical examination. A significant inverse correlation was demonstrated
- 60. Review of Literature 44 between transfusion requirements and caries in the mixed dentition. The overall number of caries in both groups of splenectomized and non splenectomized subjects, of the same average age, was almost identical. Consequently, spleenectomy and the higher number of caries are statistically more probable in individuals affected by thalassemia, of increasing age, without however being mutually correlated. Hattab FN, Abdalla MH, et al (2001)70 conducted a study on caries risk in 54 patients with Thalassemia major. They found a higher DMFT rate (22.7%) more than that reported in normal Jordanian sample (DMFT 6.26 vs 4.84). The authors emphasized the need for effective preventive measures, education and dental treatment need to be stressed for this caries risk group. Al-Wahadni AM, Taani DQ, et al (2002)62 conducted a study to determine whether β-thalassemia major is associated with an increase in the dental caries risk in 61 thalassemia patients. They were compared with 63 healthy controls DMFT. Thus, they concluded from their results that thalassaemia is associated with higher dental caries experience Luglie PF, Campus G, et al (2002)64 carried out the investigation to determine the oral status in a group of patients with thalassaemia major (TM). 18 TM patients (15 M, three F) and 18 healthy controls randomly matched for age and sex were examined for dental caries DMFT index. Dental status (DMFT index) was almost equal in the two groups (10.3 in TM vs 9.4 in controls, p=0.34). They concluded that, although no substantial differences were found between the two observed groups, further investigations are needed to determine the theoretical risk of oral diseases in thalassemic patients.
- 61. Review of Literature 45 RADIOLOGICAL CHANGES IN THALASSAEMIA The first detailed description of bone changes in thalassaemia appeared in 1927 report under the name of radiologist Lawrence Reynolds.71 Cooley, Witwer, and Lee (1927)11 described the basic changes that occur in thalassaemia major and Caffey (1965)9 reviewed new radiographic findings. Roentgenologic findings are so characteristic and striking that the X-ray film alone sometimes clinches the diagnosis or at least provides a strong clue to the nature of the disease, the blood picture and other examinations subsequently helps in establishing the diagnosis.72 The radiographic changes in thalassemia are derived from erythroid hyperplasia of bone marrow, having a more noticeable appearance than the other hemolytic anemias. The persistence and overgrowth of the erythrocyte forming marrow causes enlargement of the medullary cavities and thinning of the overlying cortical walls in the long bones and skull. As the patient reaches puberty, these changes are less obvious in peripheral skeleton but they become more pronounced in the skull, spine and pelvis.9 In skull, spine and pelvis, in which red marrow persists throughout life, the roentgenographic changes may in contrast become more pronounced, even after puberty, thus hands which are the optimal sites for roentgen identification of disease during infancy and early childhood become the least diagnostic sites after puberty.71 Mukherji M. (1938)72 described the radiographic changes in the cranial bones as, widening of the diploic space, thinning of the tables especially of the outer,
- 62. Review of Literature 46 sometimes so marked that the outer table may be totally deficient and closely packed striations at right angles to the tables. The striations may be coarse or fine. Baty JM, Blackfan KD et al (1932)45 described this appearance as “hairs standing on end”. Early in the disease or in mild cases striations may be absent, but there is always diffuse osteoporosis and expansion and later on thickening of the cranial bones. Early changes start in the horizontal plate and squamous portion of the frontal bone gradually spread backwards to the parietals and the occipital. The striations follow a different order, begin in the parietals, extend to the occipital and affect lastly the superior and temporal portions of the frontal bone, the lower portions of the frontal do not usually show the striae. In paranasal bones, overgrowth of marrow impedes their pneumatization from the outset and in some cases completely suppresses it. In temporal bones, pneumatization may be normal or completely suppressed. The frontal sinuses maybe normal, small or absent.70 When the remaining of the calvarium is thickened, there is usually a conspicuous lack of such thickening in the occipital squamosa In some severe cases, localized destruction of the overlying bone suggests the development of localized tumors of red marrow in the generally hyperplastic marrow. Caffey J. (1957)71 described that pneumatization is most consistently and most markedly retarded in the maxillary sinuses, in contrast pneumatization of the ethmoidal labyrinths is not affected, probably because normally there is little or no marrow or marrow space in these bones.
- 63. Review of Literature 47 The long and short tubular bones show expansion of the medullary canal, atrophy of the cortical layer, destruction of the cancellous tissue and a few coarse irregular trabeculations near the ends of the shafts, giving a “ground glass appearance” or “rain-drop” spaces within the cortex and a “chicken wire” appearance of enlarged marrow spaces and coarse trabeculation.50 Expansion of the shafts is usually uniform throughout their entire extent causing a rectangular contour of the tubular bones, but sometimes expansion is more pronounced at the ends producing an hour-glass, or dumb-bell shape; occurring at the lower ends of the femur the picture is that of an erlenmyer flask as in Gaucher’s disease.72 Flat bones are similarly involved. They show osteoporosis and reticulation. In fact all the bones of the skeleton are affected.3 Other radiographic manifestations include – osteoporosis of the vertebral bodies. Radionuclide studies show a generalized decrease in the skeletal uptake. Premature fusion of the epiphysis in the tubular bone of the extremities. Pathologic fractures take place as the result of cortical atrophy in 33% of patients and were most frequently in the long bones of lower extremities. Secondary hemochromatosis due to repeated transfusions. Arthropathy may also be noted. Jonh Caffey (1951)71 reported that the skeletal changes are absent or minimal during the first year of life in thalassaemia and that the rarefaction characteristic of the disease during early childhood is followed by a relative sclerosis during later childhood.
- 64. Review of Literature 48 Kaplan RI, Weather R et al (1969)44 reviewed dental and oral findings in 50 Cooley’s anemia cases. Roentgenographically the maxillary and mandibular bones showed a coarsened trabecular pattern in 43 cases (86 percent), with increased radiolucency, enlarged marrow spaces and thinning of the cortical layer of bone. Johnston FE and Krogman WM (1964)47 reviewed the patterns of growth in 50 children with thalassemia major. Each child was subjected for posterior-anterior (PA) radiograph of the hand and wrist to permit an assessment of skeletal age and growth rate, lateral and PA cephalometric image of head and face were taken for an accurate evaluation of cephalofacial growth. The authors concluded that cephalofacial manifestations of orthodontic significance seem to be concentrated mainly in maxillary alveolar bone and in the palate. Wolman IJ and Ortolani M (1964)73 reported that transfusions can help control the changes on the exterior of the skull and in other bones which are reflections of the extramedullary hemopoiesis process. Poyton HG and Davey KW (1968)74 recorded the changes visible in radiographs used in dentistry in 16 cases of thalassemia. In their series, the radiographs taken were – periapical views of posterior teeth, anterior occlusal projections of mandibular and maxillary teeth and surrounding bone and a lateral skull radiograph. The frequency of occurrence of certain radiographic appearances were ; 1. Teeth Short roots and spike shaped – This was most frequently seen in mandibular first molars and central incisors. This was observed in 9 (56.25%) of their cases. 2. Alveolar bone - Blurring or effacement of trabeculae (87.5%).
- 65. Review of Literature 49 - Large bone marrow spaces and pronounced trabeculae – 7 (43.75%) cases showed this change. This was seen most frequently in the anterior region of mouth. - Circular radiolucencies in the alveolus. This was observed in the lower anterior region (31.25%). 3. Lamina dura and crypts of teeth - Thin lamina dura and crypts – was seen in 14 cases (87.5%). - Crypts separated from teeth – This was seen less frequently than the thinning of crypts and was observed in posterior regions only (37.5%). 4. Maxilla and mandible - Osteoporosis was present in seven (43.75%) cases. It was considered an associated factor of the disease. - A sharply demarcated intermaxillary suture. It was thought as a recognized variant of normal (43.75%). - Prominent anterior maxilla – 12 (75%) cases - Small paranasal sinus – 10 (62.5%) cases - Enlarged muscle attachment at the angle of the mandible – 3 (18.75%) cases. - Thin cortex at posterior and inferior margins of the ramus (87.5%). 5. Skull - Thickening of calvarium of skull, mostly in the anterior region – 14 (87.5%) cases. - Fine granular pattern of bone (93.7%). - Circular holes in the diploe – 5 (31.25%) cases. - Condensed inner plate of Calvarium – All cases (100%). - Striations in the calvarium – 2 (12.5%) cases.
- 66. Review of Literature 50 - Shape of pituitary fossa – In 12 (75%) case the pituitary fossa was modified in shape over anterior surface. Thus the authors analysed and assessed the importance of radiographic changes. The authors concluded that following radiographic observations were significant in thalassaemia - blurring of the trabeculae, large bone marrow space and pronounced trabeculae; thin lamina dura and crypts, osteoporosis, prominent anterior maxilla, small paranasal sinus thin cortex at posterior and inferior margin of ramus, thickening of calvarium of skull, fine granular pattern of bone and condensed inner plate of calvarium. Parkin SF (1968)11 described the striations on the skull radiograph as “crew- cut” appearance. He also reported 4 cases of thalassaemia with radiographic changes. He reported that intraoral radiographs showed normal teeth and lamina dura, with a slightly altered periapical bone pattern consistent with hyperplastic bone marrow. Lateral radiographs of the skull showed the typical widened dipole in the frontal bone with hair-on-end appearance. Roy AN et al (1971)75 reviewed 150 cases of Thalassemia to study radiological changes in the bone. In their study, skull radiographs showed enlargement of dipole, thinning of cortices and generalized mottling in 74% of cases. 12% of patients had hair-on-end appearance whereas 14% of patients had normal appearance. Logothetis J, Ruth BL, et al (1971)76 conducted a cross-sectional study on 138 patients with Cooley’s anaemia from 2 to 28 years of age. They reported hair-on end appearance in 5.8% of their patients on the skull radiographs.
- 67. Review of Literature 51 Negovanovic D, Stojimirovic E, et al (1977)77 discussed Roentgeno morphologic aspects of osseous lesions in thalassaemia. They mentioned, in bones two functionally different organs are closely mingled: osseous tissue and osseous hematopoietic system. In cases of aggression toward osseous hematopoetic system osseous lesions, with their evolutive stages, are formed. Certain evolutive stags are so characteristic in their morphology that radiologic diagnosis of the illness can be made without any hesitation. Scutellari PN, Orzincolo C, et al (1985)78 conducted xeroradiographic investigations of the skull, hand, and elbow on 27 patients with homozygous β- thalassaemia. The results were compared with plain radiographic examinations. Xeroradiography was shown to demonstrate cortical thinning of long bones, swelling of the diploic space in the skull, and reticulated patterns in the elbow better than standard radiography. Moreover, the use of “positive’ mode imaging was shown to have advantages in the study of the skull and extremities. Weel F, Jackson IT, et al (1987)51 reported that the bone marrow of membranous bone is used extensively as an ancillary haemopoetic organ and the “rodent facies” with increased overbite and upper teeth exposure results. Scutellari PN, Orzincolo C, et al (1988)79 reviewed that the main abnormalities of the hand and skull in a group of patients who underwent hypertransfusion regimen and compared with the lesions observed in a control group of low-transfused patients. A possible correlation with transfusion regimen was discussed; since bone lesions are explained on the basis of relationship between proliferating bone marrow and bone cortex, hypertransfusion regimen will prevent the
- 68. Review of Literature 52 development of abnormalities, only if established early in life. For this reason, skeletal lesions in Cooley’s anaemia have changed their “classical” radiographic patterns. In the skull, the diploic space may become normal, and the overgrowth of facial bones moderate; the pneumatization of paranasal sinuses may not be completely impeded by the swelling of the jaws, the “hair-brush” pattern may disappear completely. The normalized picture of the hand remains a typical differential sign of prepubertal and adult patients. Orzincolo C, Castaldi G, et al (1988)80 described the solitary or multiple circumscribed osteolytic areas in seven patients, selected from 250 patients with homozygous β-thalassaemia. On radiographic examinations, these areas appear as purely osteolytic lesions with well defined margins not associated with sclerosis. Orzincolo C, Castaldi G, et al (1989)81 described that the skull in homozygous β-thalassaemia may present several abnormalities, such as osteopenia, widening of the diploic space, and a “hair-on-end” appearance. In some cases it presents also a particular stratified appearance caused by a variable number of osseous lamellae, parallel with the inner table. This “lamellated skull was observed in 16 out of 150 (10.6%) patients affected by the disease. Possible mechanisms were discussed. The lamellar osseous changes could be due to repeated periosteal osteoblastic reactions to the sinusoidal neovascularization associated with marrow hyperplasia in poorly transfused patients. Leonardi R., Verzi P, et al (1990)82 evaluated dental age in growing subjects with Cooley’s anemia. 34 patients aged from 4 to 11.8 years were examined. They noted that there were no difference between dental age and chronological age.
- 69. Review of Literature 53 Wisetsin S. (1990)83 studied cephalography in 60 thalassemic patients between the age of 11-16 years and 60 age matched controlled patients. He found that 18.2% showed absence of frontal sinus, 63.3% had thickening of frontal bone and parietal bone, mostly in anterior region. 36.6% had fine granular patterns of bone, 8.3% had hair-on-end appearance and 73.3% had thin cortex at posterior and inferior margins of ramus. De Luca B, Magnano C, et al (1991)84 evaluated the skull, thorax, hand and wrist standard radiographs of 29 patients affected by Cooley’s disease who were treated upto 1983 with a low transfusion regimen, rather with a high transfusion regimen. The patients have been divided into two groups, according to the prevalence of the first or the second transfusion regimen. Almost all the changes described in the literature have been found in the radiographs but completely modified. In the youngest patients the most significant appearances were ribs and hand changes, that can be considered as the most important feature in their radiological monitoring. However they mentioned that the new transitional radiological syndrome will rapidly modify with the establishment of the high transfusional regimen.
- 70. Review of Literature 54 MANAGEMENT OF THALASSEMIA The thalassaemia are the most common single gene disorder in the world and represent a major health burden worldwide. Over the last two decades broader understanding of the disease pathophysiology led to successful prenatal diagnosis, improved supportive care that resulted in decreased morbidity and prolonged life expectancy. The various treatment modalities are85,86 ; Transfusion therapy in Thalassemia has two goals 1. To prevent anemia 2. To suppress endogenous erythropoiesis as to avoid ineffective erythropoiesis. • Blood transfusion is mandatory for all children with thalassaemia major and for those children with thalassaemia intermedia who cannot maintain Hb% above 7 gm% or for those who show evidence of growth retardation, severe bony changes or hypersplenism. Regular blood transfusions are presently the mainstay of treatment of thalassaemia. Transfusion regimen may be (1) low transfusion regimen where Hb% is maintained around 6-10 gm% (2) hypertransfusion ; Hb level 10-12 gm% and supertransfusion where Hb% is maintained at 12-14 gm%.73 The popular transfusion regime of today is a hypertransfusion regime which aims at maintaining men hemoglobin levels at 12.5 gm/dl and pre-transfusion level not less than 10 gm%. Such a regimen permits normal growth and physical activity, suppresses erythropoiesis, thus preventing skeletal changes and gastrointestinal iron absorption
- 71. Review of Literature 55 and also inhibits extra-medullary hemopoiesis, thereby preventing splenomegaly and hypersplenism. With this regime, requirement of blood is high only at the initiation of therapy, and does not produce more iron overload than the low transfusion regime. Complications of Transfusions : 1) Febrile Reactions : It is seen in 3-20% of patients and may be due to leucocyte or platelet antibodies, antibodies against RBC antigens, allergic reactions to other plasma or blood proteins, or due to pyrogens present in transfused blood. 2) Hemolytic transfusion reactions 3) Other reactions uncommonly seen and thought to be of uncertain etiology are sudden development of hypertension, convulsions, cerebral hemorrhage and edema after multiple transfusions. 4) Transfusion transmitted diseases like malaria, syphilis, hepatitis B, Hepatitis C, Cytomegalovirus and HIV infection can occur. IRON OVERLOAD AND CHELATION THERAPY87 : Two factors contribute to iron overload in thalassemic child : a) Enhanced gastrointestinal absorption of iron b) Transfusional siderosis Transfusional iron overload leads to deposition of iron in the heart leading to cardiomyopathy and irregularity of heart beats, in the pancreas, in the islet of Langerhans leading to diabetes, in the liver and spleen leading to hepatosplenomegaly, hepatic fibrosis and cirrhosis of liver, in the pituitary glands leading to growth retardation, delayed puberty, in the thyroid and parathyroid gland
- 72. Review of Literature 56 leading to those sub clinical or clinical organ dysfunction, and in the skin leading to bronze or black discoloration of skin. Increased susceptibility to bacterial infection especially yersenia is seen with iron overload. Iron accumulation in the myocardium can lead to death, either by involving the conducting tissues or by causing intractable cardiac failure due to cardiomyopathy. Despite extensive research for ideal chelating agent, desferrioxamine currently the only chelating agent of real value for the management of thalassaemia, being able to promote the excretion of iron. DESFERRIOXAMINE (DFO) : Given on daily basis for a minimum of 5-6 times per week, it is given subcutaneously over 6-8 hours using an infusion pump. The daily dose of Desferal is about 30-70 mg/kg and should be tailored according to the need for the patient. In general, the goal is to keep the serum ferritin level below 1000 ng/ml. ROLE OF VITAMIN C : Ascorbic acid deficiency increases insoluble iron (hemosiderin). Vitamin C helps in conversion of hemosiderin into ferritin from which iron can be chelated. Addition of vitamin C 100 mg daily prior to DFO therapy increase iron excretion. 60% of DFO chelated iron is excreted in urine, and 40% in stool.
- 73. Review of Literature 57 NEWER CHELATING AGENTS88 : Deferriprone (L1) : It mobilizes from transferrin, ferirtin, and hemosiderin. It is undergoing extensive trials in USA, UK, Canada, India and various other centres. SPLENECTOMY: With the advent of hyper and super-transfusion therapy, splenomegaly and hypersplenism have become a rarity and hence splenectomy is usually not needed in these patients. If the child has already developed splenomegaly and signs of hypersplenism and is above 5 years of age, splenectomy is indicated. The indications for splenectomy are ; 1) An increase in the yearly requirement of packed cells more than double the basal requirement i.e. packed cell 200 cc/kg / year or more. 2) Decrease in WBC and platelet count, which is a late manifestation of hypersplenism. All children needing splenectomy should receive pneumococcal vaccine (pneumoax MSD), H-influenaza vaccine, and meningococcal vaccine 4 weeks prior to surgery. In endemic areas, prophylactic antimalarial treatment may be given to prevent malaria. Prophylactic penicillin therapy must be continued life long. Episodes of infection should be treated promptly and newer antibiotics may be empirically started to prevent septicemia and other complications. Blood culture and sensitivity of antibiotics must be performed to guide treatment.
- 74. Review of Literature 58 BONE MARROW TRANSPLANTATION89 : A ray of hope for permanent cure and better future for children with genetic disorders has brightened with the rapid advancement in the techniques and the success of bone marrow transplantation. The principles of bone marrow transplantation in thalassaemia are ; a) To destroy and prevent regeneration of defective stem cells, b) sufficient immune suppression for good engraftment of normal marrow, c) to infuse stem cells with normal gene for β-globin; d) to prevent GVHD with high doses therapy of Busulphan, Cyclophosphamide, total body irradiation and other modalities. All over the world over 1000 transplantations have been done with a 70-80% cure rate. NEOCYTE TRANSFUSION : Propper et al (1980)86 introduced the concept of transfusing thalassemic children with young red cells (neocytes). In conventionally used unit of blood, red cells have a survival of 60 days. The mean age of a neocytes being 120 days, they survive in the recipient for 90 days, thus reducing the amount of blood required and prolonging the interval between two transfusions. PHARMACOLOGICAL METHODS TO INCREASE GAMMA CHAIN PRODUCTION AND GENE MANIPULATION : It has been noted that hypomethylation of gene increases its expression and when methylated, the gene is not expressed. A number of drugs like 5’Azacytidine and hydroxyurea have been shown to increase the production of γ chains both in
- 75. Review of Literature 59 animals and human beings by causing hypomethylation of gene by decreasing the activity of the enzyme DNA methyl transferase. This increase in γ chain synthesis prevents the α chain precipitation by forming HbF (a 2 g2) and thereby increasing the life span of red cells. Butyrates : This drug is given I.V. infusion slowly over 6-8 hours in dose of 200-400 mg/kg/day and has shown to increase HbF to 8-12% and cause a rise in Hb% by 2-3 gm%. The problem with this drug is the tedious I.V. route. L-carnitine, an analogue of butyrate, has been tried in thalassemic patients but response obtained has been poor in most of the trials. Genetic Engineering90 : Insertion of normal gene in the stem cells of recipient remains a known challenging goal of future therapy. There are two main approaches to gene therapy; 1) Somatic approach in which non germ line cells are involved; 2) Transgenic approach in which transfused gene can be expressed in subsequent generations. This therapy is still in experimental stage and likely to be the therapy of future management of thalassaemia. Antenatal Diagnosis and Genetic Counseling : As thalassaemia is inherited in an autosomal recessive manner there are 25% chances of producing thalassaemia major child in each pregnancy. Population screening, identification of carriers, genetic counseling, antenatal diagnosis in women at risk and selective termination of affected fetus can prevent the birth of thalassaemia major child.
- 76. Review of Literature 60 Prenatal diagnosis can be done by estimation of relative rate of globin biosynthesis by fetoscopy and fetal blood sampling around 16-18 weeks of intrauterine life or by analysis of foetal DNA by ultrasound guided chorionic villous biopsy at around 8-9 weeks of gestation or fetal amniocytes by amniocentesis, if both the parents are carriers.
- 77. Review of Literature 61 DENTAL TREATMENT OF PATIENTS WITH THALASSEMIA When subjecting a patient with Thalassemia for dental treatment, attention should focus on the obtainment of as much information as possible to ensure safe dental management and adequate distinction among thalassemic subjects. In this sense, the type of thalassemia must be established, along with the treatments received, the degree of iron accumulation related organ involvement, and consequently also patient prognosis and life expectancy. The medical diagnosis of the specific type of thalassaemia involved is of great help, since the planning of dental treatment differs according to whether the patient presents thalassemia major or intermedia and is always conditioned by the current medical condition of the patient, future medical therapies and therefore life expectancy. In patients with thalassaemia trait, more complex treatments can be considered. The simple case history recorded by the dental professional is therefore essential for providing oral health, adequate dental treatment and quality of life.42 The salient characteristics of such patients are clearly the possible orofacial deformities and malocclusions. Such problems in patients with thalassaemia intermedia and other less severe variants maybe dealt with surgically, including remodeling of the maxillary protuberance prior to simple dental therapies for aligning the anterior incisors. Likewise, a maxillary osteotomy for positioning the jaw more posteriorly in relation to the mandible can afford an improved esthetic outcome. However, such treatments are not indicated in patients with thalassaemia major, particularly if blood transfusion and chelator therapy has been shown to be scanty effective.
