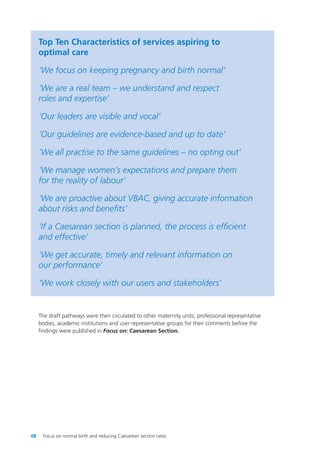
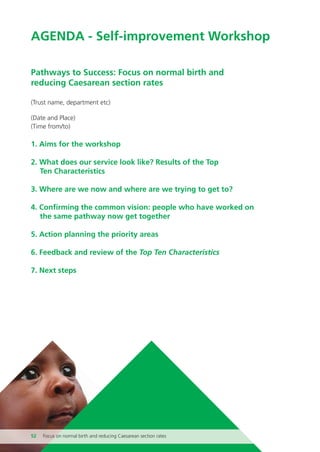
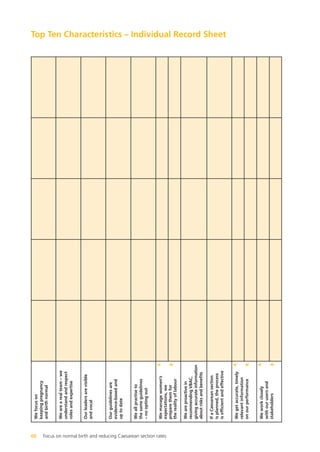
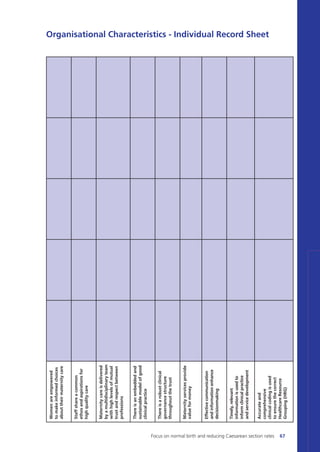
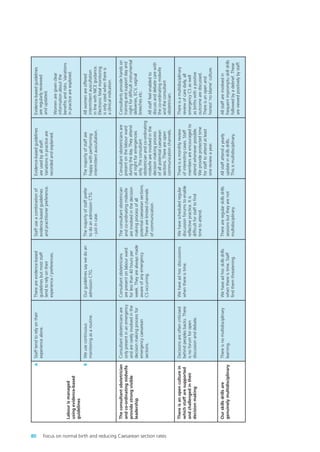
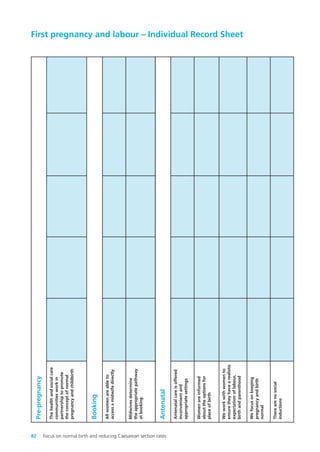
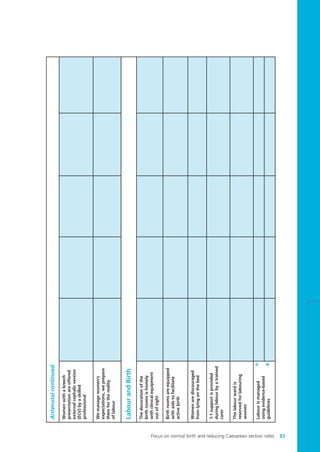
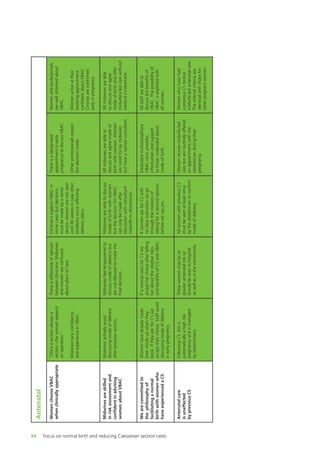
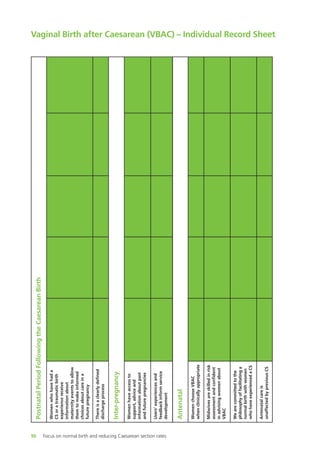
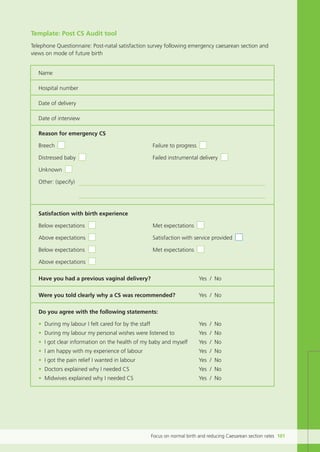
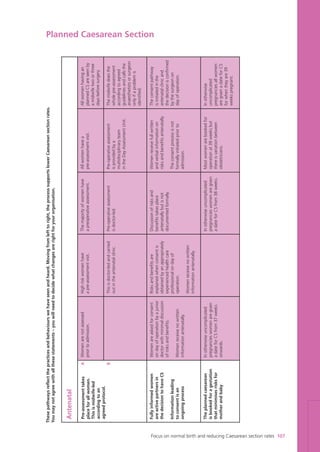
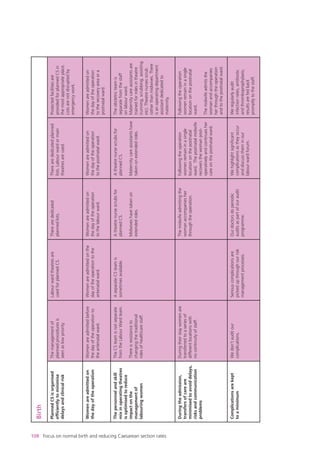
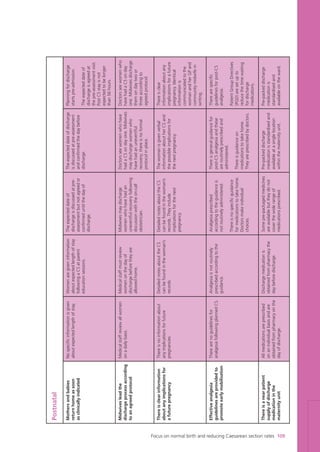
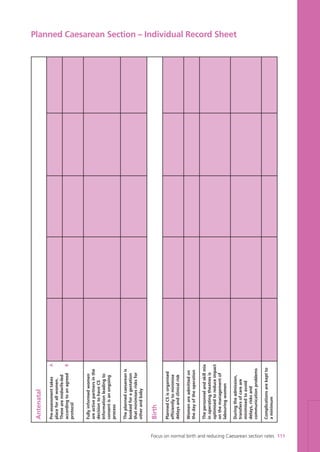
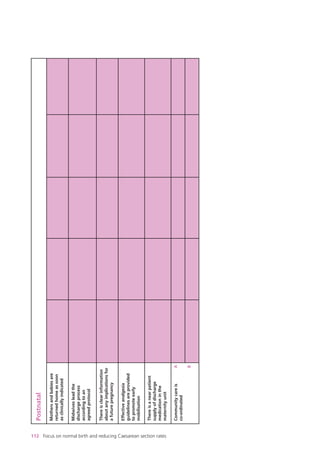
This document provides an overview of a toolkit aimed at helping NHS trusts reduce their Caesarean section rates. The toolkit was developed by the NHS Institute for Innovation and Improvement based on visits to maternity services with low C-section rates. It includes self-assessment tools covering key areas like first pregnancies, VBAC, and organizational characteristics. The goal is to help services evaluate their practices and develop action plans to promote normal birth and reduce C-section rates in a safe and sustainable way.