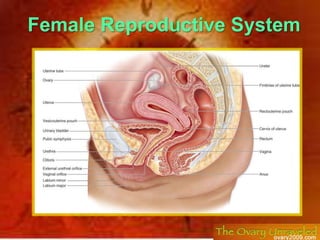
Female Reproductive Anatomy Overview
- 2. Primary sex organ: ovary Genital ducts: Fallopian tube Uterus Vagina Accessory glands: Greater vestibular (Bartholin’s) Copulatory organ (external genitalia): The vulva
- 3. They are the primary sex organs. Functions: 1-Exocrine function: produce ova 2-Endocrine function: secrete estrogen & progesterone hormones. The Ovaries
- 4. Location and Description Each ovary is oval (almond) shaped, measuring 3 2 1 cm. ovarian fossa: The ovary usually lies against the lateral wall of the pelvis in a depression called the ovarian fossa, bounded by the external iliac vessels above and by the obturator nerve, the ureter & the internal iliac vessels, behind. The position of the ovary is variable.
- 5. The ovary has: 1) 2 ends: Upper (tubal) end: is directed up & laterally & attached to: Ovarian fimbria of the Fallopian tube. Suspensory (infundibulo-pelvic) ligament of the ovary, which is a peritoneal fold that forms the upper lateral part of the broad ligament. It transmits the ovarian vessels & nerves from the side wall of the pelvis to the broad ligament. Lower (uterine) end: is directed down & medially. It is attached to the upper lateral angle of the uterus by the ligament of the ovary. 2) 2 surfaces: Lateral surface: related to the parietal peritoneum of the lateral pelvic wall & obturator nerve and vessels (in the floor of the fossa). Medial surface: related to fimbriated end of Fallopian tube. 3) 2 borders: Posterior border: free. Anterior border: attached to the upper lateral part of broad ligament by mesovarium (which transmits the ovarian nerves & vessels to the hilum of the ovary).
- 6. Ligaments Of The Ovary 1) Suspensory ligament of the ovary: It extends laterally from the tubal end of the ovary to the side wall of the pelvis. It is a peritoneal fold which transmits the ovarian vessels, nerves & lymphatics to the broad ligament. 2) Mesovarium: It is peritoneal fold that extends from the upper layer of broad ligament to the anterior border of the ovary. It transmits the ovarian vessels & nerves to the ovary. 3) Ligament of the ovary: It is a fibromuscular cord that extends from the uterine end of the ovary to the lateral angle of the uterus.
- 7. Blood Supply Arteries The ovarian artery arises from the abdominal aorta at the level of the first lumbar vertebra. Veins The ovarian vein drains into the inferior vena cava on the right side and into the left renal vein on the left side.
- 8. Lymph Drainage The lymph vessels of the ovary follow the ovarian artery and drain into the para-aortic nodes Nerve Supply: Parasympathetic: From pelvic splanchnic nerves (S 2, 3, 4). Sympathetic: from T 10, 11. The blood supply, lymph drainage, and nerve supply of the ovary reach the ovary by passing through the suspensory ligament of the ovary. The vessels and nerves finally enter the hilum of the ovary via the mesovarium
- 9. The Fallopian (Uterine) Tubes 2 tortuous tubes (about 10 cm long), open on the superolateral angle of the uterus. They have free end open into the peritoneal cavity close to the ovary. Lie in the upper border of the broad ligament
- 10. Intramural (interstitial) part: It is the shortest (1 cm) and narrowest part. It passes through the wall of the superoateral angle of the uterus to open into the uterine cavity. Isthmus: It is narrow and 2 cm in length . Ampulla: It is the longest (5 cm), thin-walled, tortuous and widest part. It is the site of fertilization. Infundibulum (fimbriated end): It is 2cm in length and funnel-shaped. It pierces the broad ligament to open into the peritoneal cavity near the ovary. Its margins carry fimbria which spread over the medial surface of the ovary. Parts Of The Uterine Tube From Medial To Lateral
- 11. Tubal ligation: A simple and effective method of birth control is to surgically ligate the uterine tubes, preventing spermatozoa from reaching ova. Conduct of the ovum in the uterine tube to the uterine cavity is helped by: ciliary movement of mucosal lining & peristaltic movement of the tube
- 12. Blood Supply Of The Uterine Tube Arterial supply: Medial 2/3: by the uterine artery. Lateral 1/3 : by the ovarian artery. Venous drainage: By veins accompanying the arteries into the uterine and ovarian veins. Lymph drainage: Most of the tubal lymphatics pass to the para-aortic L.Ns. Lymphatics of the isthmus pass to the superficial inguinal L.Ns. Commonest site of fertilization is the ampulla of the uterine tube. Implantation of the embryo in the uterine tube rather than the uterus can cause an ectopic pregnancy.
- 13. Uterus It is a hollow pear-shaped muscular organ. Location: It is located in the central part of the pelvis: Anterior to the rectum posterosuperior to the bladder. Dimension: measuring 3 2 1 inches
- 14. Parts Of The Uterus 1)Fundus: It is dome-shaped part that lies above level of the opening of the Fallopian tubes. It is completely covered by peritoneum. It is related to coils of small intestine & sigmoid colon. 2) Body: is the part extending from level of opening of the Fallopian tubes to the constriction called isthmus. It contains uterine cavity. It is the site of implantation of the zygote & also the site of menstruation.
- 15. 3) Isthmus: Slight constriction between the body and the cervix. 4) Cervix: it has supra-vaginal & vaginal parts Supra-vaginal part: Anteriorly: it is not covered by peritoneum and related to the U.B. Posteriorly: it is covered by peritoneum of Douglas pouch which separates it from the rectum. Laterally: it gives attachment to the broad ligament and is related to the ureter and uterine vessels just below the root of the broad ligament. Vaginal part: is surrounded by the vaginal fornices.
- 16. The cavity of the uterine body is triangular in coronal section, but it is a cleft in the sagittal plane. The cavity of the cervix, the cervical canal, communicates with the cavity of the body through the internal os and with that of the vagina through the external os. Before the birth of the first child, the external os is circular. In a parous woman, the vaginal part of the cervix is larger, and the external os becomes a transverse slit
- 17. Relations Of The Uterus Anteriorly: The body of the uterus is related anteriorly to the uterovesical pouch and the superior surface of the bladder. The supravaginal cervix is related to the superior surface of the bladder. The vaginal cervix is related to the anterior fornix of the vagina. Posteriorly: The body of the uterus is related posteriorly to the rectouterine pouch (pouch of Douglas) with coils of ileum or sigmoid colon within it. Laterally: The body of the uterus is related laterally to the broad ligament and the uterine artery and vein. The supravaginal cervix is related to the ureter. The vaginal cervix is related to the lateral fornix of the vagina. The uterine tubes enter the superolateral angles of the uterus, and the ligament of the ovary (posterior) and round ligament of the uterus (anterior) are attached to the uterine wall just below this level.
- 19. Arterial supply by the uterine artery: It is a branch of the anterior division of internal iliac artery. It passes medially on the floor of the pelvis in the root of the broad ligament crossing the ureter, about 2 cm lateral to the cervix. It ascends along the side of the uterus in a tortuous course between the 2 layers of the broad ligament. It turns laterally below the Fallopian tube to end by anastomosis with ovarian artery, which also assists in supplying the uterus. It supplies: uterus + medial ¾ of Fallopian tube + vagina. Venous drainage Each venous plexus is drained by a pair of uterine veins which ends into internal iliac vein.
- 21. Lymphatic drainage of the uterus
- 22. Lymphati c drainage Fundus + upper part of the body + uterine tube para-aortic L.Ns Lower part of the body external iliac L.Ns. Cornu of the uterus its lymphatics pass along the round ligament of uterus into the superficial inguinal L.Ns. Cervix internal iliac & external iliac & sacral L.Ns. Nerve supply Sympathetic from T12 & L1 (produce uterine contraction & vasoconstriction). Parasympathetic from S2, 3, 4. (produce uterine relaxation & vasodilatation).
- 23. Peritoneal Covering Of The Uterus The peritoneum reflected from the rectum to the upper part of the vagina, forming recto-uterine pouch, then cover the posterior surface of the uterus, fundus, anterior surface of the body of the uterus ,which is reflected at the isthmus on the upper surface of U.B. forming the utero- vesical pouch. So anterior surface of the cervix and vagina have no peritoneal covering
- 24. Broad Ligament It is a double-layered fold of peritoneum which extends from the side of the uterus to the side wall of the pelvis. Parts of the broad ligament: Mesosalpinx: the part between Fallopian tube & mesovarium & and round ligament of ovary. Suspensory ligament of ovary: the part lateral to the ovary. Mesometrium: the remaining medial lower part on the side of the uterus.
- 26. Broad Ligament It has:1) 2 layers: upper (posterior) layer: is related to the coils of small intestine, is connected to the ovary by mesovarium & is pierced by the lateral end of Fallopian tube lower (anterior layer) 2) 4 borders: upper free border: its medial 4/5 surrounds Fallopian tube its lateral 1/5 forms the suspensory ligament of the ovary lower border: rests on the pelvic floor medial border: attached to the side of the uterus lateral border: attached to the side wall of the pelvis
- 27. Contents Of The Broad Ligament: 2 tubes: 1-Fallopian tube: in the medial 4/5 of the upper free border. 2- ureter at root of the ligament. 2 ligaments: round ligament of ovary & round lig. of uterus. 2 arteries: 1)Uterine A. (in the root then along the medial border then along the upper border). 2)Ovarian A. (in the suspensory ligament of ovary). sympathetic nerve plexus plexus. 2 embryological remnants: epioophoron & paraoophoron. Connective tissue (parametrium) & lymphatics & L.Ns.
- 28. Positions Of The Uterus Normal position anteverted anteflexed: the long axis of the uterus is bent forward on the long axis of the vagina.This position is referred to as anteversion (90 degree) of the uterus . the long axis of the body of the uterus is bent forward at the level of the internal os with the long axis of the cervix. This position is termed anteflexion (170 degree) of the uterus .
- 29. Abnormal position: retroverted, retroflexed the fundus and body of the uterus are bent backward on the vagina so that they lie in the rectouterine pouch (pouch of Douglas). In this situation, the uterus is said to be retroverted. If the body of the uterus is, in addition, bent backward on the cervix, it is said to be retroflexed. Leads to back pain.
- 30. The uterus is supported mainly by: A) muscles 1) the tone of the Pelvic diaphragm (pelvic floor) muscles: levator ani muscles and coccygeus muscle. resisting downward push of uterus during increased intra-abdominal pressure. 2) Urogenital diaphragm: the muscles of the deep perineal pouch. 3) Perineal body: is a fibromuscular body between the vagina & anal canal; receiving the insertions of all perineal muscles. Thus, maintains the integrity of the pelvic floor. Supporting Factors Of Uterus
- 31. Levator Ani Muscle They form a broad muscular sheet stretching across the pelvic cavity, they support the pelvic viscera and resist the intra-abdominal pressure transmitted downward through the pelvis. The medial edges of the anterior parts of the levator ani muscles are attached to the cervix of the uterus by the pelvic fascia. It is incomplete anteriorly to allow passage of urethra and vagina in female. Action: it supports and maintains the pelvic viscera in position.
- 32. Some of the fibers of levator ani are inserted into a fibromuscular structure called the perineal body This structure is important in maintaining the integrity of the pelvic floor; The perineal body lies in the perineum between the vagina and the anal canal. It thus supports the vagina and, indirectly, the uterus.
- 33. and the condensations of pelvic fascia, which form three important B) ligaments. The Transverse Cervical, Pubocervical, and Sacrocervical Ligaments These three ligaments are attached to the cervix and the vault of the vagina and play an important part in supporting the uterus and keeping the cervix in its correct position
- 34. Ligaments of the cervix: 1. Transverse cervical (Mackenrodt’s ) cardinal ligament: It is the main supporting factor of the uterus. It a fan-shaped ligament, which is formed of condensed extraperitoneal tissue between the side wall of the pelvis and side of cervix & vagina. 2. Pubo-cervical ligament: It is a condensation of extraperitoneal tissue, which extends from the front of cervix & upper part of vagina to the back of the pubis, around the sides of the urethra. 3. Utero-sacral (sacrocervical) ligament: It is a condensation of extraperitoneal tissue, which extends from the back of the cervix to the front of 2nd & 3rd pieces of sacrum, around the sides of the rectum.
- 35. 4) The round ligament of the uterus,: which represents the remains of the lower half of the gubernaculum, extends between the superolateral angle of the uterus, through the deep inguinal ring and inguinal canal, to the subcutaneous tissue of the labium majus. It helps keep the uterus anteverted (tilted forward) and anteflexed (bent forward). The round ligament of the uterus and 5)the broad ligament are considered to play a minor role in supporting the uterus.
- 36. Uterine Prolapse Damage to the levatores ani muscles or ligaments of the cervix during childbirth or general poor body muscular tone may result in downward displacement of the uterus called uterine prolapse. In advanced cases, the cervix descends the length of the vagina and may protrude through the orifice. if the perineal body is damaged during childbirth, prolapse of the pelvic viscera may occur. Caesarean section: opening the abdomen, when normal child birth is not possible. Hysterectomy: removal of uterus in case of cancer.
- 37. Vagina It is a fibromuscular tube extends upward & backward from the vestibule to the cervix It is copulatory organ in female & serve as a passage for menstrual flow & child birth. Its upper part surrounding the cervix forming Anterior, posterior , right lateral and left lateral fornices. It is 8 cm long vaginal opening may be partially covered by the hymen
- 38. Relations Anterior wall: (7 cm) Not covered by peritoneum Its upper 1/3 is pierced by the cervix. Its middle 1/3 is related to the base of U.B. Its lower 1/3 is related to the urethra. Posterior wall: (9 cm) Its upper1/4 is covered by peritoneum which is reflected to the rectum to form the recto-vaginal (Douglas pouch) which contains coils of ileum Its middle 2/4 related to rectum. Its lower 1/4 is related to perineal body and anal canal. Lateral relations (from above downwards): Upper part: uterine artery & ureter. Middle part: levator ani (sphincter vaginae). Lower part : greater vestibular gland (in the perineum)
- 39. Fornices of vagina: These are 4 pouches formed by the upper part of vagina around the vaginal part of cervix (2 lateral, 1 anterior & 1 posterior) The posterior fornix is the deepest one & the only one covered by peritoneum Lateral one related to uterine artery & ureter.
- 40. Arterial supply It is supplied by: Uterine artery. Vaginal artery. Middle rectal artery. Internal pudendal artery. Venous drainage The vaginal veins form plexuses that drains into internal iliac vein. Lymphatic drainage Upper 1/3 external iliac L.Ns. Middle 1/3 internal iliac L.Ns. Lower 1/3 superficial inguinal L.Ns. Nerve supply Upper 2/3 (pain insensitive) by autonomic fibers Sympathetic: L1, 2 Parasympathetic: S 2, 3 Lower 1/3 (pain sensitive) brs. of pudendal nerve.
- 42. Supports of the Vagina The upper part of the vagina is supported by: the levatores ani muscles and the transverse cervical, pubocervical, and sacrocervical ligaments. These structures are attached to the vaginal wall by pelvic fascia. The middle part of the vagina is supported by the urogenital diaphragm. The lower part of the vagina, especially the posterior wall, is supported by the perineal body
- 43. External Genitalia (Vulva) Mons pubis - Fatty area overlying the pubic symphysis Covered with pubic hair after puberty Labia – skin folds Labia majora—hair-covered skin folds Labia minora—delicate, hair-free folds of skin Contain the vestibule: Greater vestibular glands Urethral orifice Vaginal orifice Clitoris located at the anterior regions of the labia minora: composed of sensitive erectile tissue