More Related Content
Similar to 2014 nature.pdf
Similar to 2014 nature.pdf (20)
2014 nature.pdf
- 1. NATURE REVIEWS | NEUROLOGY ADVANCE ONLINE PUBLICATION | 1
Department of
Neurology, Mayo Clinic,
200 First Street SW,
Rochester, MN 55905,
USA.
benarroch.eduardo@
mayo.edu
The clinical approach to autonomic failure
in neurological disorders
Eduardo E. Benarroch
Abstract | Central or peripheral neurological disorders can manifest with autonomic failure or autonomic
hyperactivity, which may affect the sympathetic, parasympathetic and/or enteric nervous systems. Disorders
causing autonomic failure can be classified according to the presence or absence of associated neurological
manifestations, such as peripheral neuropathy or parkinsonism, and their temporal profile (acute or subacute,
chronic progressive, static, or episodic). A systematic approach allows focused evaluation to detect treatable,
potentially disabling or life-threatening conditions. Subacute isolated autonomic failure affecting sympathetic,
parasympathetic and enteric nervous system function, in various combinations, occurs in autoimmune
autonomic ganglionopathy, which might be the first manifestation of an underlying neoplasm. Autonomic
failure can be an important feature of several types of peripheral neuropathy, including sensorimotor peripheral
neuropathies, sensory ganglionopathy, and distal painful peripheral neuropathies. Progressive autonomic
failure occurs in neurodegenerative synucleinopathies such as multiple system atrophy and Lewy body
disorders. Autonomic failure may also occur in hereditary leukoencephalopathies or prion disorders. This
Review outlines the clinical approach to patients with generalized autonomic failure, focusing predominantly
on classification and diagnosis, but also touching briefly on treatment and management.
Benarroch, E. E. Nat. Rev. Neurol. advance online publication 27 May 2014; doi:10.1038/nrneurol.2014.88
Introduction
Autonomic disorders manifest with autonomic failure
or hyperactivity, which may be generalized or focal.
Autonomic failure can affect the sympathetic, parasympa
thetic or enteric nervous systems, either in isolation or in
various combinations, and can result from lesions at any
level of the CNS or PNS. Sympathetic failure manifests
primarily with orthostatic hypotension and anhidrosis
(absence of sweating), cranial parasympathetic failure
with intolerance to light, dry eyes (xerophthalmia) and
dry mouth (xerostomia), sacral parasympathetic failure
with urinary retention and erectile dysfunction, and
enteric nervous system (ENS) failure with gastroparesis
and constipation. In some cases, postural tachycardia
syndrome is a manifestation of an underlying autonomic
neuropathy. Many symptoms attributed to ‘dysautonomia’
in otherwise healthy young patients, such as gastroparesis
or urinary retention, are rarely associated with objective
evidence of autonomic failure.
This Review will focus on the clinical approach to
patients with generalized autonomic failure. The degen
erative synucleinopathies, autonomic ganglionopathies
and autonomic neuropathies have been reviewed in
detail elsewhere.1–5
Rather than providing an exhaustive
discussion of the wide spectrum of disorders associated
with autonomic failure, this article will focus on specific
examples to emphasize clinical cues and outline recent
concepts of the underlying pathobiology.
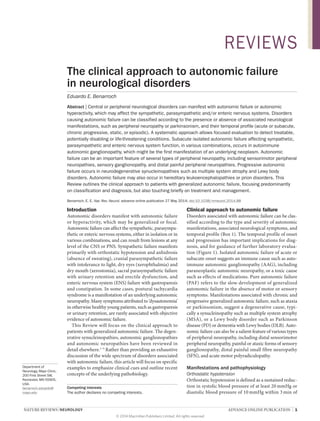
Clinical approach to autonomic failure
Disorders associated with autonomic failure can be clas
sified according to the type and severity of autonomic
manifestations, associated neurological symptoms, and
temporal profile (Box 1). The temporal profile of onset
and progression has important implications for diag
nosis, and for guidance of further laboratory evalua
tion (Figure 1). Isolated autonomic failure of acute or
subacute onset suggests an immune cause such as auto
immune autonomic ganglionopathy (AAG), including
paraneoplastic autonomic neuropathy, or a toxic cause
such as effects of medications. Pure autonomic failure
(PAF) refers to the slow development of general
ized
auto
nomic failure in the absence of motor or sensory
symp
toms. Manifestations associated with chronic and
pro
gressive generalized autonomic failure, such as ataxia
or parkinsonism, suggest a degenerative cause, typi
cally a synuclein
opathy such as multiple system atrophy
(MSA), or a Lewy body disorder such as Parkinson
disease (PD) or dementia with Lewy bodies (DLB). Auto
nomic failure can also be a salient feature of various types
of peripheral neuropathy, including distal sensori
motor
peripheral neuropathy, painful or ataxic forms of sensory
ganglionopathy, distal painful small fibre
neuropathy
(SFN), and acute motor polyradiculopathy.
Manifestations and pathophysiology
Orthostatic hypotension
Orthostatic hypotension is defined as a sustained reduc
tion in systolic blood pressure of at least 20 mmHg or
diastolic blood pressure of 10 mmHg within 3 min of
Competing interests
The author declares no competing interests.
REVIEWS
© 2014 Macmillan Publishers Limited. All rights reserved
- 2. 2 | ADVANCE ONLINE PUBLICATION www.nature.com/nrneurol
standing or head-up tilt.6
Some patients with neuro
genic orthostatic hypotension have postprandial hypo
tension.7
Manifestations of orthostatic hypotension
include lightheadedness, blurred vision and neck pain
(coat hanger distribution) among others; the symptoms
are worse in the morning, after meals, or on exposure
to heat.8,9
Neurogenic orthostatic hypotension is the mani
festation of impaired sympathetically mediated vaso
constriction of skeletal muscle and mesenteric vessels in
response to baroreceptor unloading due to orthostatic
stress. Neurogenic orthostatic hypotension may occur
as a consequence of disorders affecting the barosensi
tive sympathoexcitatory neurons in the rostral ventro
lateral medulla (for example, MSA); spinal preganglionic
sympathetic neurons (for example, MSA or PD); auto
nomic ganglia (for example, AAG or PAF); unmyelin
ated axons (SFN); noradrenaline availability (for
example, dopamine β‑hydroxylase deficiency); or vas
cular α1-adrenergic receptors (typically as a side effect
of drugs).10
Anhidrosis
Sweating is an important thermoregulatory activity
mediated by the sympathetic nervous system through
cholinergic activation of muscarinic M3
receptors in
the eccrine sweat glands. Depending on its distribu
tion and severity, anhidrosis might be asymptomatic
or might manifest with compensatory hyperhidrosis
(in unaffected areas) or heat intolerance. Anhidrosis
in autonomic failure may reflect impairment of central
thermoregulatory pathways, spinal preganglionic
sudomotor units, cholinergic sympathetic ganglion
neurons, peripheral unmyelinated axons, or M3
receptors
at the sudomotor unit.11
Neurogenic bladder and sexual dysfunction
Normal bladder function includes a urine storage
phase and a micturition phase, which are controlled
at all levels of the neuraxis.12
Urine storage depends on
spinal reflexes mediated by the lumbosacral sympathetic
noradrenergic and sacral cholinergic motor neurons of
the Onuf nucleus. Normal micturition depends on a
Key points
■
■ Autonomic failure can occur in isolation, in association with peripheral
neuropathy, or as a manifestation of a neurodegenerative disorder
■
■ Disorders associated with autonomic failure can be classified according to
the type and severity of autonomic manifestations, associated neurological
symptoms, and temporal profile
■
■ Acute or subacute autonomic failure suggests an autoimmune autonomic
ganglionopathy, which may be paraneoplastic
■
■ In patients with parkinsonism and autonomic failure, early onset and
progression of orthostatic hypotension or urogenital dysfunction, urinary
incontinence, generalized anhidrosis, and/or laryngeal stridor are highly
suggestive of multiple system atrophy
■
■ Autonomic failure can occur with any type of diabetic or amyloid neuropathy
■
■ Important causes of painful neuropathy associated with autonomic failure
include Sjögren syndrome, HIV infections, Fabry disease, and sodium
channelopathies
supraspinal reflex coordinated by the pontine mictur
ition centre, which activates the sacral pre
gangli
onic
para
sympa
thetic output to the bladder detrusor while
simultaneously inhibiting the Onuf nucleus.13
Neurogenic bladder can manifest with detrusor over
activity or underactivity.14
Detrusor overactivity pro
duces urinary urgency with or without incontinence,
urinary frequency, and nocturia. Reduced detrusor
activity leads to incomplete bladder emptying, increased
post-void residual, low peak urinary flow rate and, even
tually, urinary retention and overflow incontinence.
Impaired micturition can result from lesions affecting
the bladder afferents, sacral parasympathetic neurons or
their axons, or cholinergic muscarinic neurotransmis
sion. Neurogenic bladder is commonly associated with
erectile and ejaculatory dysfunction in men and poor
vaginal lubrication in women. Erectile dysfunction
reflects impaired sacral parasympathetic output and
nitric oxide release in the erectile tissue.
Box 1 | Neurological causes of autonomic failure
A. Isolated autonomic failure
1. Acute or subacute
(a) Autoimmune autonomic ganglionopathy
(b) Paraneoplastic autonomic neuropathy
2. Progressive
(a) Pure autonomic failure
B. Progressive autonomic failure associated with
parkinsonism, ataxia or dementia
1. Multiple system atrophy
2. Lewy body disorders
(a) Parkinson disease
(b) Dementia with Lewy bodies
3. Others
(a) Familial leukoencephalopathies
(b) Prion disorders
C. Autonomic failure associated with peripheral
neuropathy
1. Chronic sensorimotor neuropathies
(a) Diabetes
(b) Amyloidosis
(c) Other metabolic disorders (vitamin B12
deficiency,
uraemia)
(d) Toxic neuropathies
2. Sensory ganglionopathies
(a) Sjögren syndrome
(b) Paraneoplastic
3. Distal painful neuropathies
(a) Diabetes
(b) Amyloidosis
(c) Idiopathic (sodium channelopathies)
(d) Infectious (HIV)
(e) Hereditary
(i) Hereditary sensory and autonomic neuropathy
(ii) Fabry disease
(iii) Sodium channelopathies
4. Acute or subacute motor polyradiculopathy or
neuropathy
(a) Guillain–Barré syndrome
(b) Porphyria
5. Acute autonomic and sensory neuropathy
6. Ross syndrome (segmental anhidrosis, Adie pupils
and areflexia).
REVIEWS
© 2014 Macmillan Publishers Limited. All rights reserved
- 3. NATURE REVIEWS | NEUROLOGY ADVANCE ONLINE PUBLICATION | 3
Gastrointestinal dysmotility
Control of gastrointestinal motility depends on intrin
sic reflexes mediated by the ENS, and their modulation
by vagal and paravertebral sympathetic inputs. Upper
gastro
intestinal motility is primarily controlled by the
vagal reflexes involving the nucleus of the solitary tract
and dorsal motor nucleus of the vagus in the medulla;15
peristalsis in the lower gastrointestinal tract depends
primarily on local ENS reflexes;16
and paravertebral
sympathetic reflexes inhibit gastrointestinal motility.
Symptoms of delayed oesophageal transit include
dysphagia and regurgitation. Delayed gastric emptying
produces early satiety, anorexia, nausea, bloating, belch
ing, postprandial vomiting, and pain. Lower gastro
intestinal dysmotility manifests with constipation and,
occasionally, diarrhoea.
Evaluation
Clinical
In addition to a careful history and general physical and
neurological examination, clinical evaluation of patients
with suspected autonomic failure includes assessment of
pupil size, symmetry and reactivity with both bright and
dim light; measurement of blood pressure and heart rate
after 2min in the supine position and at 1min and 2min
after standing; and examination of the skin to identify
areas of localized or generalized absence of or excessive
sweating, and changes in skin temperature or colour in
the hands and feet.
Laboratory tests
General laboratory tests that should be performed in
patients with autonomic failure include determination
of serum glucose (or in some cases haemoglobin A1c),
thyroid-stimulating hormone and vitamin B12
levels.
Serum and urine protein electrophoresis with immuno
fixation, including light-chain quantitation, are indi
cated to detect amyloid light-chain (AL) amyloidosis.17
SSA and SSB antibody testing for Sjögren syndrome may
be helpful in some cases. Determination of ganglionic
nicotinic acetylcholine receptor (gnAChR) antibodies,18
as well as paraneoplastic antibodies (particularly anti-
Hu, P/Q and N‑type voltage-gated calcium channel
and voltage-gated potassium complex anti
bodies), is
indicated in all patients with subacute onset of symp
toms.18,19
Determination of forearm venous catecho
lamines, including noradrenaline, dopamine and
adrenaline, in the supine position and after 5–10 min
of standing may be helpful in some cases; the results
require careful interpretation, however, as they can be
Parkinsonism, ataxia
Autonomic studies, neuroimaging (MRI),
polysomnogram, urodynamic studies,
neuropsychometrics
Autonomic studies, electromyography/nerve
conduction studies, FBG, SPEP
, UPEP
,
abdominal fat aspirate, ANCA, HIV,
α-galactosidase, punch skin biopsy
Associated
manifestations
Onset/
subtype
Main or
typical causes
Specific
evaluation*
Autonomic studies
Autoantibodies
(gnAChR,
paraneoplastic)
Sjögren
syndrome
Paraneoplastic
Diabetes
Amyloidosis
‘Pure’
autonomic
failure
Multiple
system
atrophy
Lewy body
disorders
■ PD
■ DLB
Autoimmune
autonomic
ganglionopathy
Paraneoplastic
autonomic
ganglionopathy
Vasculitis
HIV
Idiopathic
Fabry disease
Hereditary
Peripheral neuropathy
None (‘pure’ autonomic failure)
Chronic, progressive Subacute
sensory
Distal painful
Distal
sensorimotor
or any other
type
Acute or subacute
Autoantibodies
(SSA/SSB, paraneoplastic)
Salivary gland biopsy
Autonomic failure
Figure 1 | Evaluating the main causes of autonomic failure. All patients with autonomic failure should undergo
determination of serum glucose (or in some cases haemoglobin A1c), thyroid stimulating hormone and vitamin B12
levels.
Autonomic laboratory testing is helpful to detect and assess severity of autonomic failure. Patients with acute isolated
autonomic failure should also be tested for gnAChR and paraneoplastic antibodies, and SSA and SSB autoantibodies in
cases with prominent sensory symptoms. Patients with chronic progressive autonomic failure, including multiple system
atrophy, PD or DLB, should also undergo MRI (if possible), polysomnography, urodynamic studies and, in some cases,
neuropsychometric testing. Evaluation of patients with autonomic failure associated with peripheral neuropathy includes
electromyography and nerve conduction studies, SPEP and UPEP with immunofixation, abdominal fat aspirate
and/or sural nerve biopsy for detection of amyloidosis and, in some cases, determination of ANCA, HIV serology or
α‑galactosidase. Punch skin biopsy can also be helpful to detect small fibre neuropathy. *Include thermoregulatory sweat
test, sudomotor axon reflex tests, heart rate response to deep breathing and Valsalva manoeuvre, beat-to-beat blood
pressure profile during the Valsalva manoeuvre, and blood pressure and heart rate responses to head-up tilt.
Abbreviations: ANCA, antineutrophil cytoplasmic antibodies; DLB, dementia with Lewy bodies; FBG, fasting blood glucose;
gnAChR, ganglionic nicotinic acetylcholine receptor; PD, Parkinson disease; SPEP, serum protein electrophoresis; UPEP,
urine protein electrophoresis.
REVIEWS
© 2014 Macmillan Publishers Limited. All rights reserved
- 4. 4 | ADVANCE ONLINE PUBLICATION www.nature.com/nrneurol
affected by concomitant use of drugs or impaired pre
synaptic noradrenaline reuptake.20
Low or undetectable
noradrenaline and adrenaline levels associated with
increased dopamine levels indicate a deficit of dopamine
β‑hydroxylase as the cause of orthostatic hypotension.21
Autonomic function tests
Autonomic laboratory evaluation is indicated to deter
mine the extent and severity of autonomic failure; to
detect autonomic failure in patients with parkinsonism
or ataxia; to assess small fibre function in patients with
peripheral neuropathy or ganglionopathy; to evalu
ate patients with symptoms of orthostatic intolerance;
and to obtain objective evidence of disease progression
or response to medications.22,23
The most commonly
used tests assess sudomotor, cardiovagal and adren
ergic vasomotor functions. Sudomotor function tests
include the thermoregulatory sweat test (TST), which
assesses the integrity of central and peripheral sudo
motor pathways,22
and sudomotor axon reflex tests such
as the quantitative sudomotor axon reflex test (QSART)23
and the quanti
tative direct and indirect test of sudo
motor function (QDIRT),24
which assess the peripheral
sympathetic cholinergic innervation of the sweat glands.
Tests that assess vagal control of the sinus node (cardio
vagal function) include the heart rate response to deep
breathing,25
and the heart rate response to the Valsalva
manoeuvre, or Valsalva ratio.26
Tests that indirectly assess
sympathetic vasomotor function include the beat-to-beat
blood pressure profile during the Valsalva manoeuvre27
and the blood pressure response to head-up tilt.28
The
physiological basis, methods, normal and abnormal
responses, and pitfalls of these and other autonomic
function tests have been the subject of several reviews.29–31
Other tests
Electromyography is indicated for patients with periph
eral neuropathy or ganglionopathy, and MRI may be
helpful in evaluation of central autonomic disorders.
Gastrointestinal motility and urodynamic studies might
be indicated in some cases. Polysomnography to detect
sleep-related respiratory dysfunction is indicated in all
patients with suspected MSA.
Tissue biopsy
Skin biopsy with assessment of intraepidermal nerve
fibre density (IENFD) can be useful in the evaluation
of SFN;32,33
immunocytochemical markers allow quanti
fication of the density of innervation of sweat gland34
and pilomotor35
nerves. Abdominal fat aspirate or sural
nerve biopsy are indicated to evaluate for amyloidosis.36,37
Immunostaining and laser microdissection, along with
mass spectrometry-based proteomic analysis of amyloid
deposition, allow identification of the specific subtype of
amyloid protein.38
Neurodegenerative synucleinopathies
Autonomic failure is an important manifestation of
neuro
degenerative disorders characterized by the pres
ence of intracellular inclusions containing α‑synuclein.
These conditions include MSA,1,39–41
and Lewy body
disorders such as PD, DLB or PAF.42,43
Multiple system atrophy
MSA was initially defined as a sporadic neurodegenera
tive disease characterized by any combination of auto
nomic failure, parkinsonism, cerebellar ataxia and/or
pyramidal signs.44
The prevalence of MSA has been esti
mated at 4–8 cases per 100,000 people, and its incidence
varies from 0.6 cases per 100,000 person-years in the
general population to 3 cases per 100,000 person-years
in people above 50 years of age.1,40
The neuropathological hallmark of MSA is the accumu
lation of α‑synuclein-immunoreactive glial cytoplasmic
inclusions in oligodendrocytes, and neuronal loss in the
striatum, substantia nigra pars compacta, pontine nuclei,
inferior olivary nuclei, cerebellum, and premotor auto
nomic nuclei.45
According to current criteria, probable
MSA is defined as a sporadic, progressive, adult-onset
(over 30 years of age) disease characterized by autonomic
failure, with urinary incontinence and erectile dysfunc
tion (in males) or orthostatic hypotension (blood pres
sure decrease ≥30mmHg systolic or ≥15mmHg diastolic
within 3min of standing), as well as parkinsonism poorly
responsive to levodopa (MSA‑P), or cerebellar syndrome
(MSA‑C).39
A large European study including 437 patients
with probable (72%) or possible (28%) MSA showed that
symptomatic autonomic failure was present in almost all
cases; the most frequent manifestations were urinary dys
function (83%) and orthostatic hypotension (75%).41
In a
study on 29 autopsy-confirmed cases, a pattern consist
ing of severe and progressive adrenergic and sudomotor
failure was highly predictive of MSA.46
Although MSA is still generally regarded as a sporadic
disease, several studies have identified familial cases.1
A recent study identified mutations of the coenzyme Q2
(COQ2) gene in Japanese families with MSA, and COQ2
variants were also associated with an increased risk of
sporadic MSA.47
Median survival from symptom onset in MSA is
8–10 years, but the spectrum ranges from 4–15 years.
Natural history studies indicate that presence of the
parkinsonian variant, early onset of autonomic failure,
incomplete bladder emptying, and shorter duration
of symptoms at baseline are all factors that predict
shorter survival.48–50
In MSA, orthostatic hypotension occurs at earlier
stages and is more severe than in PD.51
Orthostatic
hypotension in MSA reflects involvement of pre
gangli
onic sympathetic neurons52
and sympathoexcitatory
neurons of the rostral ventrolateral medulla.53
Urogenital
manifestations may herald the onset of MSA.51
Bladder
dysfunction in MSA is characterized by urinary urgency,
followed by incontinence and incomplete bladder empty
ing. These manifestations result from a combination of
detrusor hyperreflexia and urethral sphincter weakness
followed by detrusor contraction failure,54
and they
reflect involvement of the pontine micturition centre,55
sacral preganglionic neurons56
and Onuf nucleus.57
Erectile dysfunction is almost always present in male
REVIEWS
© 2014 Macmillan Publishers Limited. All rights reserved
- 5. NATURE REVIEWS | NEUROLOGY ADVANCE ONLINE PUBLICATION | 5
patients with MSA.58
Upper gastrointestinal symptoms,
constipation and faecal incontinence occur frequently;
anal sphincter electromyography shows large motor
unit potentials indicating denervation due to loss of
Onuf nucleus motor neurons.59
Anhidrosis occurs in the
majority of patients with MSA, and the percentage of
the body affected by anhidrosis may help to differentiate
MSA from PD.60,61
An important manifestation of disrupted brainstem
homeostatic mechanisms in MSA is sleep-related dis
ordered breathing, including sleep apnoea and laryn
geal stridor, which occur in up to 70% of patients with
MSA.62–64
Whereas the development of central hypo
ventilation and laryngeal stridor is closely related to the
severity of autonomic failure, respiratory manifestations
can occur early in the course of MSA.65
Laryngeal dys
tonia with inspiratory adduction of the vocal cords might
underlie laryngeal stridor in at least some individuals with
MSA.66
Impaired automatic ventilation reflects involve
ment of the brainstem respiratory network, including
the pre-Bötzinger complex67
and the medullary raphe,68
which may predispose patients to sudden death.69
Lewy body disorders
Accumulation of Lewy neurites and Lewy bodies in
the ENS, autonomic ganglia, peripheral autonomic
nerve terminals, and intermediolateral cell column
can be detected at autopsy of cases of incidental Lewy
body disease (ILBD), PAF, early-stage PD, and DLB.70–73
α‑Synuclein inclusions can be also detected in cutaneous
nerves of patients with PAF74
or PD.75
These findings
indicate that Lewy body disorders constitute a contin
uum of progressive involvement of areas of the periph
eral autonomic nervous system, and subsequently the
CNS, by α‑synuclein neuropathology, which may range
clinically from asymptomatic cases (ILBD) to pure auto
nomic failure (PAF), and might eventually manifest with
parkinsonism (PD), dementia (DLB) or both.
Pure autonomic failure
PAF was first described by Bradbury and Eggleston in
1925, and was initially termed idiopathic orthostatic
hypotension. PAF is a rare, sporadic, adult-onset dis
order characterized by symptomatic orthostatic hypo
tension and variable gastrointestinal, bladder and sexual
dysfunction, in the absence of somatic motor deficits.
Onset is typically between 50 and 70 years of age.42
The symptoms of PAF are insidious in onset, and are
less progressive and disabling than those in other neuro
degenerative autonomic disorders. Some patients may
have bladder symptoms, erectile or ejaculatory dysfunc
tion, or impaired sweating, before developing ortho
static hypotension. Constipation is common, but other
symptoms of gastrointestinal dysmotility are rare.76
The
diagnosis of PAF is always tentative; after a few years,
many patients with presumed PAF may develop cerebel
lar, extrapyramidal or cognitive deficits indicating MSA,
PD or DLB. Thus, the diagnosis of PAF requires at least a
5 year history of isolated autonomic dysfunction without
other neurological manifestations. PAF is a clinical
syndrome reflecting involvement of the autonomic gan
glion cells and their postganglionic axons. This disorder
can have a variety of different pathobiological substrates.
Patients with PAF have been shown to have accumula
tion of α‑synuclein-containing Lewy bodies and neurites
in sympathetic ganglia peripheral tissues, including skin
sympathetic nerves.74,75
However, some cases of PAF are
associated with low-titre gnAChR antibodies, suggesting
that this condition can reflect a chronic form of AAG in
some instances.77
Parkinson disease
Autonomic dysfunction—particularly gastrointestinal
dysmotility—is a prominent nonmotor manifestation
of PD.43
Gastrointestinal dysmotility in PD can affect
any level of the gastrointestinal tract.78
Gastrointestinal
symptoms can occur at an early stage of the disease;79
for
example, constipation may precede the development of
motor symptoms by several years.80,81
Excessive drooling
in PD must reflect oropharyngeal dysphagia, as salivary
secretion is reduced even at an early stage of disease;82,83
this finding is consistent with the presence of α‑synuclein
pathology in the salivary gland.84
Oesophageal dysmotility
and delayed gastric emptying are frequent manifestations
in PD,85,86
and are likely to reflect early involvement of
the dorsal motor nucleus of the vagus.70
The prevalence
of constipation ranges from 20–89%,79
and is primarily
attributable to slow colonic transit, reflecting the early
involvement of the ENS.87
However, defecatory dysfunc
tion due to paradoxical contraction of the
puborectalis
muscle is also an important contributory factor.85,88
Orthostatic hypotension is estimated to occur in
16–58% of patients with PD.89
In general, orthostatic
hypotension in PD is asymptomatic and tends to occur
at later stages of disease than in MSA, but in a subgroup
of patients it may be early and prominent, manifesting
even before the initiation of dopaminergic therapy.89
Urinary symptoms occur in 38–71% of patients with
PD.77,90,91
The most prominent symptom is nocturia, fol
lowed by urgency and frequency, and the most common
urodynamic finding is detrusor overactivity.92
Nocturia is
the only urinary symptom that improves after deep brain
stimulation of the subthalamic nucleus.
Differential diagnosis
The differential diagnosis between MSA‑P and PD with
autonomic failure can be difficult. A prospective study
showed that autonomic indices, particularly the percent
age of the body affected by anhidrosis, were significantly
and persistently more abnormal in MSA than in PD with
autonomic failure.61
Urodynamic findings such as large
post-micturitional residual volume (100ml), detrusor
external sphincter dyssynergia, and open bladder neck
at the start of filling are highly suggestive of MSA.54
Anal sphincter denervation due to loss of Onuf nucleus
motor neurons may help to distinguish MSA from PD
within the first few years of onset of motor symptoms,
but this finding is not specific for MSA, and can occur
in progressive supranuclear palsy or in PD patients with
chronic constipation.93
REVIEWS
© 2014 Macmillan Publishers Limited. All rights reserved
- 6. 6 | ADVANCE ONLINE PUBLICATION www.nature.com/nrneurol
Structural brain imaging, including diffusion-
weighted and diffusion tensor MRI, and functional
imaging, including PET and single-photon emis
sion CT (SPECT), might aid the differential diagnosis
between MSA and PD.1
The presence of atrophy in the
putamen, middle cerebellar peduncle and pons on MRI
serve as supporting features for the diagnosis of pos
sible MSA.39
Signal changes on T2-weighted images,
including the slit-like void signal (hypointensity of
the posterior putamen surrounded by hyperintense
lateral putaminal rim) and the hot cross bun sign (due
to myelin loss in the basis pontis) are more charac
teristic of MSA but are not specific for this condition.
Diffusion-weighted imaging shows elevated apparent
diffusion coefficient in the putamen, pons and middle
cerebellar peduncle in MSA.94
In MSA‑P, but not in PD,
brain perfusion SPECT shows striatal hypoperfusion,95
and 18
F-fluorodeoxyglucose PET shows striatal hypo
metabolism.96
By contrast, dopamine transporter SPECT
using 123
I-FP-CIT demonstrates reduced striatal binding
in both disorders.97
Myocardial scintigraphy using 123
I-metaiodobenzyl
guanidine (MIBG)98
or 6‑18
F-fluorodopamine PET99
assesses postganglionic sympathetic innervation of the
heart; these modalities are potential tools to differenti
ate between MSA and Lewy body disorders. However,
although initial studies suggested that loss of cardiac
sympathetic innervation in PD or PAF could help in
distinguishing Lewy body disorders from MSA,99,100
decreased cardiac MIBG uptake has also been found in
up to 30% of patients with MSA,101
possibly reflecting
coexistent Lewy body pathology.
Dementia with Lewy bodies
Severe autonomic dysfunction, as well as repeated falls
and syncope, are features supporting the diagnosis of
DLB.102
Orthostatic hypotension, urinary frequency
and urge incontinence can be disabling symptoms in
DLB,103,104
and symptomatic orthostatic hypotension
may occur in 30–50% of cases. On the basis of auto
nomic laboratory evaluation, the severity of autonomic
failure in DLB is intermediate between that seen in MSA
and PD.105
Other neurodegenerative disorders
Other central neurodegenerative disorders can manifest
with autonomic failure that reflects peripheral autonomic
involvement. These conditions, which may clinically
mimic MSA or Lewy body disorders, include fragile X
tremor–ataxia syndrome, in which bladder symptoms
might be prominent;106
adult-onset autosomal dominant
leukodystrophy, which is associated with pure sympa
thetic failure;107
and a novel prion disorder character
ized by diarrhoea and length-dependent, predominantly
sensory and autonomic axonal neuropathy, followed by
cognitive decline.108
Autoimmune autonomic disorders
Autoimmune autonomic disorders are characterized
by acute or subacute onset of generalized or restricted
autonomic failure, including gastrointestinal enteropathy.
Early recognition of these disorders is important because
they are disabling and might be the initial manifestation
of an underlying neoplasm. In addition, patients with
autoimmune autonomic disorders may show substantial
improvement with
immunomodulatory therapy.4,109
Autoimmune autonomic ganglionopathy
AAG (formerly known as acute pandysautonomia or
idiopathic subacute autonomic neuropathy18,110
) is
characterized by severe autonomic failure that develops
over the course of days or weeks in a previously healthy
person. The onset of symptoms may follow a viral infec
tion, minor surgical procedure, or vaccination. The
most common manifestation is generalized sympathetic,
parasympathetic and ENS failure, but the spectrum is
broad; symptoms might be confined to pure choliner
gic neuropathy manifested by sicca syndrome, isolated
adrenergic neuropathy, or isolated gastrointestinal dys
motility. Patients may recover spontaneously, but only
one-third experience substantial functional improvement
without treatment.
Approximately 50% of cases of subacute AAG are
associ
ated with gnAChR antibodies18
that block trans
mission at the autonomic ganglia. Antibody titres
correlate with the severity of autonomic failure.19,111
gnAChR antibodies can also be associated with chronic
or restricted forms of autonomic dysfunction,77
and with
neurological or paraneoplastic disorders unrelated to
the autonomic nervous system.19
In one series, 30% of
gnAChR-seropositive patients had other paraneoplastic
antibodies in the setting of occult cancer, most com
monly adenocarcinoma.19
In some cases, AAG coexists
with other autoimmune disorders, such as myasthenia
gravis, in patients with occult cancer.112,113
Several observational studies report that patients
with gnAChR-seropositive AAG benefit from intra
venous immunoglobulin, plasma exchange, prednisone,
mycophenolate, azathioprine and rituximab, either
individually or in combination.19,114–116
A substantial
percentage of patients with AAG are seronegative for
gnAChR and other autoantibodies;117
some of these
patients may also show symptomatic improvement with
immunomodulatory therapy.116
Paraneoplastic autonomic neuropathy
A type of subacute autonomic neuropathy that is clinically
indistinguishable from idiopathic AAG might occur as
a manifestation of an occult neoplasm, most commonly
small-cell lung carcinoma associated with anti-Hu
antibodies or, less frequently, thymoma or other neo
plasms.118,119
Like AAG, paraneoplastic autonomic neuro
pathy may manifest with generalized autonomic failure,
or with isolated enteric ganglionopathy leading to the
intestinal pseudo-obstruction syndrome.120,121
Acute autonomic and sensory neuropathy
Acute autonomic and sensory neuropathy is a rare dis
order that differs from AAG in that profound autonomic
failure is associated with various degrees of sensory
REVIEWS
© 2014 Macmillan Publishers Limited. All rights reserved
- 7. NATURE REVIEWS | NEUROLOGY ADVANCE ONLINE PUBLICATION | 7
impairment, including loss of pain and temperature
sensation, followed by sensory ataxia due to impair
ment of proprioception.109,122,123
The mean age of onset
is in the late second decade, but can vary from child
hood to the elderly. A triggering event, such as respira
tory or gastrointestinal tract infections, is reported in
two-thirds of patients. Gastrointestinal dysmotility is
the most prominent autonomic symptom; the sensory
loss affects the proximal regions of the limbs, face, scalp
and trunk, and tends to be asymmetrical and segmen
tal. Pain in the involved region is a common and serious
symptom. Other features of this disorder are reduction of
sensory nerve action potentials and increased T2 signal
in the posterior columns of the cervical spinal cord.123
Autopsy studies have shown severe neuronal cell loss in
the thoracic sympathetic and dorsal root ganglia, and
in Auerbach’s plexus.123
Sjögren syndrome
Primary Sjögren syndrome manifests with a wide variety
of peripheral neuropathies or ganglionopathies.124
Dorsal
root ganglionopathy may manifest with neuropathic pain
or ataxic neuropathy; autonomic neuropathy might be
prominent in some cases, but is the least frequent form
of neuropathy overall.124
Autoantibodies against muscarinic M3
receptors have
been identified in a subset of patients with Sjögren syn
drome.125
These antibodies are particularly prevalent in
juvenile cases126
and have cholinergic blocking actions
in vitro.127
Some patients with Sjögren syndrome and
chronic progressive autonomic failure have gnAChR
antibodies, which may predict a positive response to
immunomodulatory therapy.128
Peripheral neuropathies
Peripheral neuropathies associated with autonomic
failure present with various phenotypes, including typical
distal symmetric sensorimotor neuropathy; dorsal root
ganglionopathy manifesting with neuropathic pain or
sensory ataxia; demyelinating, predominantly motor
polyradiculopathy; or distal painful neuropathy. The
spectrum of severity of autonomic failure is highly vari
able in these disorders, ranging from being a major cause
of disability, as can occur in neuropathies associated
with diabetes or amyloidosis, to restricted distal vaso
motor and sudomotor impairment in the lower limbs,
as observed in painful SFN.
Diabetic autonomic neuropathy
Diabetic neuropathies are heterogeneous: they include
typical diabetic sensorimotor polyneuropathy, painful
diabetic neuropathy, and diabetic autonomic neuro
pathy.129
Estimates of the prevalence of diabetic auto
nomic neuropathy vary depending of the source of
information (community, clinic or tertiary referral centre)
and the type of tests performed to assess autonomic func
tion.129
Using strict criteria based on autonomic testing
abnormalities, the prevalence in one study was 16.8% for
patients with type 1 and 34.3% for patients with type 2
diabetes mellitus.130
Diabetic autonomic neuropathy can affect cardio
vascular, gastrointestinal, urogenital and sudomotor
functions to various degrees. In most of the typical cases,
a combination of cardiovascular tests and sudomotor
tests allows its detection in otherwise asympto
matic
patients. An impaired heart rate response to deep
breathing
—an indicator of cardiovagal failure—has the
greatest specificity (~80%).131,132
Characteristic mani
festations of diabetic cardiovascular autonomic neuro
pathy include resting tachycardia, exercise intolerance,
orthostatic hypotension, intraoperative cardiovascular
instability, and silent myocardial infarction–silent ischae
mia syndrome. Cardiovascular autonomic neuropathy
has been associated with increased morbidity and mor
tality,133
so screening for this condition should be per
formed at the time of diagnosis of type 2 diabetes and
5 years after the diagnosis of type 1 diabetes, particularly
in high-risk patients.129
Upper gastrointestinal dysmotility, which is present
in 40–50% of longstanding cases of diabetes, may
affect postprandial blood glucose levels and glycaemic
control. Constipation is the most frequent gastrointesti
nal symptom in diabetes, and was reported by 60% of
patients in one study.134
Profuse, watery and predomi
nantly nocturnal diarrhoea135
and faecal incontinence136
may be disabling in some patients. Bladder symptoms
occur in up to 50% of patients; 43–87% of type 1 and 25%
of type 2 diabetic patients have abnormal urodynamic
findings.137,138
Erectile dysfunction has a reported preva
lence of 35–90% in patients with diabetes.139,140
Length-
dependent loss of thermoregulatory sweating is common,
and is occasionally associated with compensatory hyper
hidrosis.22
Gustatory sweating can result from aberrant
innervation of sweat glands by parasympathetic fibres.141
Some patients with diabetes develop an acute painful
neuropathy associated with autonomic failure within a
short time of commencing tight glucose control.142
The
symptoms may be associated with abnormal autonomic
test results and reduced IENFD on punch skin biopsy,
and can all improve over time.142
Amyloid neuropathy
Amyloidoses manifesting with autonomic neuro
pathy include the AL type (which may be associated
with myeloma or macroglobulinaemia), and familial
amyloid polyneuropathy (FAP), which is most com
monly linked to mutations in the transthyretin (TTR)
gene. The types of amyloid neuropathy associated with
autonomic failure are highly heterogeneous.143,144
In a
retrospective study on 65 cases of AL amyloidosis or
FAP, generalized autonomic failure was associated with
painful (62%) or nonpainful (17%) sensorimotor poly
neuropathy or distal SFN (5%); autonomic failure also
occurred without neuropathy (11%), but polyneuro
pathy without generalized autonomic failure was infre
quent (6%).143
In AL amyloidosis, peripheral neuropathy
may be the presenting feature or an incidental finding
of the disease, and can occur in up to 20% of cases.145
The median survival of patients with AL amyloidosis
who have peripheral neuropathy has improved with the
REVIEWS
© 2014 Macmillan Publishers Limited. All rights reserved
- 8. 8 | ADVANCE ONLINE PUBLICATION www.nature.com/nrneurol
Table 1 | General management of autonomic failure
Symptom Approach Comments
Orthostatic
hypotension
Patient education: recognize atypical symptoms of
orthostatic hypotension; get up slowly from bed; urinate
in the sitting position; avoid hot, humid environments;
exercise regularly; avoid straining; keep a blood
pressure diary; discontinue aggravating drugs
The most important aspect of management
Sleep with the head elevated 4in (reverse
Trendelenburg position)
Avoids supine hypertension and nocturnal polyuria
Postural countermanouevres (for example, leg crossing,
squatting)
Increases orthostatic tolerance
Support garments (waist-high support stockings,
abdominal binder)
Reduces venous pooling
Volume expansion (daily intake of 8–10g sodium,
fluid intake of at least 2.0–2.5l)
Initial step before pharmacological management
Rapid ingestion of 500ml tap water Rapidly increases blood pressure independently
of volume expansion
Dietary changes; avoid alcohol; eat small, frequent
meals (carbohydrate is best ingested with the last
meal of the day)
Prevents splanchnic vasodilation
Florinef (0.1–0.4mg daily) Adverse effects include supine hypertension, ankle
oedema, hypokalaemia, hypomagnesaemia, headache,
and reduced effects of warfarin
Midodrine (10–40mg daily) Adverse effects include scalp tingling or itching,
goose bumps, supine hypertension, and urinary urgency
or retention
Pyridostigmine (60–240mg daily) Adverse effects include nausea, abdominal cramps,
diarrhoea, increased salivation, urinary urgency and
bradycardia
Droxidopa (100–600mg TID) Main potential adverse effect is supine hypertension
Erythropoietin (25–75U/kg SQ) Iron supplementation is usually required; supine
hypertension may occur
Desmopressin nasal spray (5–40μg) Risk of water intoxication and hyponatraemia
Octreotide (25–200μg SQ) Adverse effects include nausea and abdominal cramps,
hypertension, risk of gallstones and postprandial
hyperglycaemia
Neurogenic
bladder
Anticholinergics (for example, oxybutynin, tolterodine);
clean intermittent self-catheterization
Adverse effects include constipation, dry mouth, risk
of glaucoma, and worsening of cognitive function
Drooling Anticholinergics; botulinum toxin Anticholinergics may worsen confusion; botulinum toxin
may worsen dysphagia
Gastroparesis Metoclopramide (5–20mg QID); domperidone
(10–30mg QID); erythromycin (50–250mg QID);
pyridostigmine (30–60mg TID); bethanechol (25mg
QID); nutritional support (low-fat, low-fibre oral
supplementation; infusion of formula via a jejunal
feeding tube)
Gastroparesis may impair absorption of levodopa;
metoclopramide is contraindicated in parkinsonian
disorders; domperidone may cause QT prolongation,
and is not available in the USA
Constipation Fibre supplementation (15g per day); bulk agents
(for example, psyllium [1tsp up to three times daily],
methylcellulose); osmotic laxatives (for example, milk
of magnesia [two tablets up to four times daily],
polyethylene glycol [17g in 25ml once or twice daily],
lactulose [15–30ml TID]); docusate (stool softener,
100mg BID); lubiprostone (24μg BID); pyridostigmine
(up to 180–540mg); bisacodyl (10mg up to three times
a week); antibiotics to prevent bacterial overgrowth;
surgery for intractable colonic inertia
Donepezil and other cholinesterase inhibitors may
cause diarrhoea
Erectile
dysfunction
Oral phosphodiesterase type 5 inhibitors (for example,
sildenafil 25–100mg)
Adverse effects include headache, flushing, nasal
congestion, blue vision, and non-arteritic ischaemic
optic neuropathy; these drugs may worsen orthostatic
hypotension
Intracavernous drugs (for example, alprostadil,
papaverine)
Adverse effects include penile pain, oedema and
haematoma, palpable nodules or plaques, and priapism
Abbreviations: BID, twice a day; QID, four times a day; SQ, subcutaneous; TID, three times a day.
REVIEWS
© 2014 Macmillan Publishers Limited. All rights reserved
- 9. NATURE REVIEWS | NEUROLOGY ADVANCE ONLINE PUBLICATION | 9
combination of melphalan, prednisone and autologous
stem cell transplantation.146
The clinical and pathological features of FAP have
been reviewed in detail elsewhere.147,148
Over 100 muta
tions in the TTR gene have been identified, the most
common (~50% of cases of FAP worldwide) of which
causes a Val30Met substitution. Different TTR variants
contribute to variable age at diagnosis, degree of cardiac
involvement, and survival.149
The first-line specific treat
ment of choice for Val30Met TTR-FAP is liver transplan
tation.150
In addition, tafamidis, a stabilizer of tetrameric
transthyretin, has shown short-term effectiveness in
slowing the progression of peripheral neuropathy at very
early stages of Val30Met TTR-FAP.151
Painful small fibre neuropathies
Selective involvement of postganglionic as well as noci
cep
tive fibres in painful SFN typically manifests with
distal anhidrosis (or sometimes hyperhidrosis) and
vasomotor dysfunction (generally erythema, but some
times vasoconstriction and coldness) in the lower limbs.
In some cases, SFN can result in more-generalized
autonomic failure that may be symptomatic or detect
able with autonomic testing. Important examples of
painful SFN are those associated with HIV infections152
and Fabry disease,153
in addition to the types related to
dia
betes and amyloidosis, as highlighted above. Distal
sympathetic sudomotor and vasomotor failure in con
junction with neuropathic pain also occur in sodium
channelopathies associated with gain-of-function
SCNA9 mutations, both in familial syndromes154
and in
a substantial proportion of idiopathic SFN cases.155
The
SCNA9 gene encodes the Nav
1.7 voltage-gated sodium
channel, which is expressed in nociceptive dorsal root
ganglion and sympathetic neurons. These gain-of-
function mutations cause increased excitability of the
nociceptor and hypoexcitability of sympathetic ganglion
neurons,156,157
which might explain the coexistence of
neuropathic pain and postganglionic sympathetic failure.
Management issues
A detailed discussion of the management of autonomic
failure is beyond the scope of this Review, but the general
approach is summarized in this section and in Table 1.
The principles of management include discontinua
tion of potentially causative drugs; immunomodula
tory therapy for autoimmune disorders; management
of diabetes, amyloidosis or other potentially treatable
cause of autonomic neuropathy; patient education; non-
pharmacological approaches; and pathophysiologically
based drug therapy. Patient education is a fundamen
tal aspect of management. For example, patients with
orthostatic hypotension should be instructed to recog
nize atypical symptoms and avoid precipitating factors.
Appropriate fluid and sodium intake, dietary adjust
ments and regular exercise are beneficial in most cases
of autonomic failure.
Conclusions
The wide spectrum of clinical manifestations and dis
orders associated with autonomic failure requires a
systematic clinical and laboratory approach to establish
the diagnosis, particularly in cases where autonomic
failure is disabling or life-threatening. A careful history
and examination is the mainstay of diagnosis, and lab
oratory and other ancillary tests must be prioritized to
search for potentially treatable causes. Patient education,
avoidance of precipitating factors, non-pharmacological
approaches, and pathophysiologically based drug therapy
form the basis of current treatment of these disorders.
Further elucidation of the pathobiological mechanisms
that lead to immune, metabolic or degenerative damage
or dysfunction of central and peripheral autonomic
neurons will provide more-specific therapeutic targets.
Review criteria
A PubMed search from 1st
January 1975 to 15th
December
2013 was performed using the following terms (individually
and in various combinations): “autonomic failure”,
“autonomic neuropathy”, “orthostatic hypotension”,
“multiple system atrophy”, “Parkinson disease”, “Lewy
body disease”, “dementia with Lewy bodies”, “autoimmune
autonomic ganglionopathy”, “paraneoplastic”, “diabetic
neuropathy”, “amyloid neuropathy”, “Sjögren syndrome”,
“leukoencephalopathy”, “fragile X” and “prion”. The
search was limited to full articles published in English.
Other articles were identified from bibliographies of the
retrieved articles.
1. Stefanova, N., Bucke, P
., Duerr, S.
Wenning, G. K. Multiple system atrophy: an
update. Lancet Neurol. 8, 1172–1178 (2009).
2. Cersosimo, M. G. Benarroch, E. E. Autonomic
involvement in Parkinson’s disease: pathology,
pathophysiology, clinical features and possible
peripheral biomarkers. J. Neurol. Sci. 313,
57–63 (2012).
3. Vernino, S. Autoimmune and paraneoplastic
channelopathies. Neurotherapeutics 4, 305–314
(2007).
4. Muppidi, S. Vernino, S. Autoimmune
autonomic failure. Handb. Clin. Neurol. 117,
321–327 (2013).
5. Freeman, R. Autonomic peripheral neuropathy.
Lancet 365, 1259–1270 (2005).
6. Freeman, R. et al. Consensus statement on the
definition of orthostatic hypotension, neurally
mediated syncope and the postural tachycardia
syndrome. Auton. Neurosci. 161, 46–48 (2011).
7. Mathias, C. J. et al. Differential blood pressure
and hormonal effects after glucose and xylose
ingestion in chronic autonomic failure. Clin. Sci.
(Lond.) 77, 85–92 (1989).
8. Mathias, C. J., Mallipeddi, R. Bleasdale-
Barr, K. Symptoms associated with orthostatic
hypotension in pure autonomic failure and
multiple system atrophy. J. Neurol. 246,
893–898 (1999).
9. Freeman, R. Clinical practice. Neurogenic
orthostatic hypotension. N. Engl. J. Med. 358,
615–624 (2008).
10. Benarroch, E. E. The arterial baroreflex:
functional organization and involvement in
neurologic disease. Neurology 71, 1733–1738
(2008).
11. Cheshire, W. P. Freeman, R. Disorders
of sweating. Semin. Neurol. 23, 399–406
(2003).
12. Fowler, C. J., Griffiths, D. de Groat, W. C. The
neural control of micturition. Nat. Rev. Neurosci.
9, 453–466 (2008).
13. Holstege, G. Micturition and the soul. J. Comp.
Neurol. 493, 15–20 (2005).
14. Panicker, J. N. Fowler, C. J. The bare
essentials: uro-neurology. Pract. Neurol. 10,
178–185 (2010).
15. Travagli, R. A., Hermann, G. E., Browning, K. N.
Rogers, R. C. Brainstem circuits regulating
gastric function. Annu. Rev. Physiol. 68, 279–305
(2006).
16. Furness, J. B. The enteric nervous system and
neurogastroenterology. Nat. Rev. Gastroenterol.
Hepatol. 9, 286–294 (2012).
REVIEWS
© 2014 Macmillan Publishers Limited. All rights reserved
- 10. 10 | ADVANCE ONLINE PUBLICATION www.nature.com/nrneurol
17. Kyle, R. A. Bayrd, E. D. Amyloidosis: review of
236 cases. Medicine (Baltimore) 54, 271–299
(1975).
18. Vernino, S. et al. Autoantibodies to ganglionic
acetylcholine receptors in autoimmune
autonomic neuropathies. N. Engl. J. Med. 343,
847–855 (2000).
19. McKeon, A., Lennon, V. A., Lachance, D. H.,
Fealey, R. D. Pittock, S. J. Ganglionic
acetylcholine receptor autoantibody: oncological,
neurological, and serological accompaniments.
Arch. Neurol. 66, 735–741 (2009).
20. Goldstein, D. S. Catecholamines 101. Clin.
Auton. Res. 20, 331–352 (2010).
21. Robertson, D. et al. Isolated failure of autonomic
noradrenergic neurotransmission. Evidence for
impaired β‑hydroxylation of dopamine. N. Engl.
J. Med. 314, 1494–1497 (1986).
22. Fealey, R. D., Low, P
. A. Thomas, J. E.
Thermoregulatory sweating abnormalities in
diabetes mellitus. Mayo Clin. Proc. 64, 617–628
(1989).
23. Low, P
. A. Autonomic nervous system function.
J. Clin. Neurophysiol. 10, 14–27 (1993).
24. Gibbons, C. H., Illigens, B. M., Centi, J.
Freeman, R. QDIRT: quantitative direct and
indirect test of sudomotor function. Neurology
70, 2299–2304 (2008).
25. Bennett, T. et al. Assessment of vagal control of
the heart in diabetes. Measures of R–R interval
variation under different conditions. Br. Heart J.
39, 25–28 (1977).
26. Booth, R. W. Ryan, J. M. The clinical use of the
Valsalva maneuver. Heart Bull. 10, 111–113
(1961).
27. Sandroni, P
., Benarroch, E. E. Low, P
. A.
Pharmacological dissection of components of
the Valsalva maneuver in adrenergic failure.
J. Appl. Physiol. 71, 1563–1567 (1991).
28. Cooke, J. et al. Sitting and standing blood
pressure measurements are not accurate for the
diagnosis of orthostatic hypotension. QJM 102,
335–339 (2009).
29. Low, P
. A. Testing the autonomic nervous
system. Semin. Neurol. 23, 407–421 (2003).
30. Freeman, R. Assessment of cardiovascular
autonomic function. Clin. Neurophysiol. 117,
716–730 (2006).
31. Hilz, M. J. Dutsch, M. Quantitative studies of
autonomic function. Muscle Nerve 33, 6–20
(2006).
32. Lauria, G. et al. European Federation of
Neurological Societies/Peripheral Nerve Society
Guideline on the use of skin biopsy in the
diagnosis of small fiber neuropathy. Report of a
joint task force of the European Federation of
Neurological Societies and the Peripheral Nerve
Society. Eur. J. Neurol. 17, 903–912, e44–e49
(2010).
33. Donadio, V. et al. Peripheral autonomic
neuropathy: diagnostic contribution of skin
biopsy. J. Neuropathol. Exp. Neurol. 71,
1000–1008 (2012).
34. Gibbons, C. H., Illigens, B. M., Wang, N.
Freeman, R. Quantification of sweat gland
innervation: a clinical-pathologic correlation.
Neurology 72, 1479–1486 (2009).
35. Nolano, M. et al. Quantification of pilomotor
nerves: a new tool to evaluate autonomic
involvement in diabetes. Neurology 75,
1089–1097 (2010).
36. Libbey, C. A., Skinner, M. Cohen, A. S. Use of
abdominal fat tissue aspirate in the diagnosis
of systemic amyloidosis. Arch. Intern. Med. 143,
1549–1552 (1983).
37. Kyle, R. A. Greipp, P
. R. Amyloidosis (AL).
Clinical and laboratory features in 229 cases.
Mayo Clin. Proc. 58, 665–683 (1983).
38. Klein, C. J. et al. Mass spectrometric-based
proteomic analysis of amyloid neuropathy type in
nerve tissue. Arch. Neurol. 68, 195–199 (2011).
39. Gilman, S. et al. Second consensus statement
on the diagnosis of multiple system atrophy.
Neurology 71, 670–676 (2008).
40. Wenning, G. K., Ben Shlomo, Y., Magalhaes, M.,
Daniel, S. E. Quinn, N. P
. Clinical features and
natural history of multiple system atrophy. An
analysis of 100 cases. Brain 117, 835–845
(1994).
41. Kollensperger, M. et al. Presentation, diagnosis,
and management of multiple system atrophy in
Europe: final analysis of the European multiple
system atrophy registry. Mov. Disord. 25,
2604–2612 (2010).
42. Kaufmann, H. Biaggioni, I. Autonomic failure in
neurodegenerative disorders. Semin. Neurol. 23,
351–363 (2003).
43. Chaudhuri, K. R. Schapira, A. H. Non-motor
symptoms of Parkinson’s disease: dopaminergic
pathophysiology and treatment. Lancet Neurol.
8, 464–474 (2009).
44. Graham, J. G. Oppenheimer, D. R. Orthostatic
hypotension and nicotine sensitivity in a case of
multiple system atrophy. J. Neurol. Neurosurg.
Psychiatry 32, 28–34 (1969).
45. Papp, M. I., Kahn, J. E. Lantos, P
. L. Glial
cytoplasmic inclusions in the CNS of patients
with multiple system atrophy (striatonigral
degeneration, olivopontocerebellar atrophy
and Shy–Drager syndrome). J. Neurol. Sci. 94,
79–100 (1989).
46. Iodice, V. et al. Autopsy confirmed multiple
system atrophy cases: Mayo experience and
role of autonomic function tests. J. Neurol.
Neurosurg. Psychiatry 83, 453–459 (2012).
47. Multiple-System Atrophy Research Collaboration.
Mutations in COQ2 in familial and sporadic
multiple-system atrophy. N. Engl. J. Med. 369,
233–244 (2013).
48. Tada, M. et al. Early development of autonomic
dysfunction may predict poor prognosis in
patients with multiple system atrophy. Arch.
Neurol. 64, 256–260 (2007).
49. O’Sullivan, S. S. et al. Clinical outcomes of
progressive supranuclear palsy and multiple
system atrophy. Brain 131, 1362–1372 (2008).
50. Wenning, G. K. et al. The natural history of
multiple system atrophy: a prospective European
cohort study. Lancet Neurol. 12, 264–274 (2013).
51. Wenning, G. K. et al. Time course of symptomatic
orthostatic hypotension and urinary incontinence
in patients with postmortem confirmed
parkinsonian syndromes: a clinicopathological
study. J. Neurol. Neurosurg. Psychiatry 67,
620–623 (1999).
52. Oppenheimer, D. R. Lateral horn cells in
progressive autonomic failure. J. Neurol. Sci. 46,
393–404 (1980).
53. Benarroch, E. E., Smithson, I. L., Low, P
. A.
Parisi, J. E. Depletion of catecholaminergic
neurons of the rostral ventrolateral medulla in
multiple systems atrophy with autonomic failure.
Ann. Neurol. 43, 156–163 (1998).
54. Winge, K. Fowler, C. J. Bladder dysfunction in
Parkinsonism: mechanisms, prevalence,
symptoms, and management. Mov. Disord. 21,
737–745 (2006).
55. Benarroch, E. E. Schmeichel, A. M. Depletion
of corticotrophin-releasing factor neurons in the
pontine micturition area in multiple system
atrophy. Ann. Neurol. 50, 640–645 (2001).
56. Kennedy, P
. G. Duchen, L. W. A quantitative
study of intermediolateral column cells in motor
neuron disease and the Shy–Drager syndrome.
J. Neurol. Neurosurg. Psychiatry 48, 1103–1106
(1985).
57. Chalmers, D. Swash, M. Selective
vulnerability of urinary Onuf motoneurons in
Shy–Drager syndrome. J. Neurol. 234, 259–260
(1987).
58. Kirchhof, K., Apostolidis, A. N., Mathias, C. J.
Fowler, C. J. Erectile and urinary dysfunction may
be the presenting features in patients with
multiple system atrophy: a retrospective study.
Int. J. Impot. Res. 15, 293–298 (2003).
59. Sakakibara, R. et al. Colonic transit time,
sphincter EMG, and rectoanal videomanometry
in multiple system atrophy. Mov. Disord. 19,
924–929 (2004).
60. Sandroni, P
., Ahlskog, J. E., Fealey, R. D.
Low, P
. A. Autonomic involvement in
extrapyramidal and cerebellar disorders.
Clin. Auton. Res. 1, 147–155 (1991).
61. Lipp, A. et al. Prospective differentiation of
multiple system atrophy from Parkinson disease,
with and without autonomic failure. Arch. Neurol.
66, 742–750 (2009).
62. Iranzo, A. Sleep and breathing in multiple system
atrophy. Curr.Treat. Options Neurol. 9, 347–353
(2007).
63. Ghorayeb, I., Bioulac, B. Tison, F. Sleep
disorders in multiple system atrophy. J. Neural
Transm. 112, 1669–1675 (2005).
64. Silber, M. H. Levine, S. Stridor and death
in multiple system atrophy. Mov. Disord. 15,
699–704 (2000).
65. Glass, G. A., Josephs, K. A. Ahlskog, J. E.
Respiratory insufficiency as the primary
presenting symptom of multiple-system atrophy.
Arch. Neurol. 63, 978–981 (2006).
66. Vetrugno, R. et al. Sleep-related stridor due to
dystonic vocal cord motion and neurogenic
tachypnea/tachycardia in multiple system
atrophy. Mov. Disord. 22, 673–678 (2007).
67. Schwarzacher, S. W., Rub, U. Deller, T.
Neuroanatomical characteristics of the human
pre-Bötzinger complex and its involvement in
neurodegenerative brainstem diseases. Brain
134, 24–35 (2011).
68. Benarroch, E. E., Schmeichel, A. M., Low, P
. A.
Parisi, J. E. Depletion of putative chemosensitive
respiratory neurons in the ventral medullary
surface in multiple system atrophy. Brain 130,
469–475 (2007).
69. Tada, M. et al. Depletion of medullary
serotonergic neurons in patients with multiple
system atrophy who succumbed to sudden
death. Brain 132, 1810–1819 (2009).
70. Braak, H. et al. Stanley Fahn Lecture 2005:
the staging procedure for the inclusion body
pathology associated with sporadic Parkinson’s
disease reconsidered. Mov. Disord. 21,
2042–2051 (2006).
71. Dickson, D. W. et al. Evidence that incidental
Lewy body disease is pre-symptomatic
Parkinson’s disease. Acta Neuropathol. 115,
437–444 (2008).
72. Jellinger, K. A. A critical reappraisal of current
staging of Lewy-related pathology in human
brain. Acta Neuropathol. 116, 1–16 (2008).
73. Beach, T. G. et al. Multi-organ distribution of
phosphorylated alpha-synuclein histopathology
in subjects with Lewy body disorders. Acta
Neuropathol. 119, 689–702 (2010).
74. Shishido, T. et al. α‑Synuclein accumulation in
skin nerve fibers revealed by skin biopsy in pure
autonomic failure. Neurology 74, 608–610
(2010).
75. Wang, N., Gibbons, C. H., Lafo, J. Freeman, R.
α‑Synuclein in cutaneous autonomic nerves.
Neurology 81, 1604–1610 (2013).
76. Polinsky, R. J. Clinical autonomic
neuropharmacology. Neurol. Clin. 8, 77–92
(1990).
REVIEWS
© 2014 Macmillan Publishers Limited. All rights reserved
- 11. NATURE REVIEWS | NEUROLOGY ADVANCE ONLINE PUBLICATION | 11
77. Klein, C. M. et al. The spectrum of autoimmune
autonomic neuropathies. Ann. Neurol. 53,
752–758 (2003).
78. Pfeiffer, R. F. Gastrointestinal dysfunction in
Parkinson’s disease. Parkinsonism Relat. Disord.
17, 10–15 (2011).
79. Siddiqui, M. F., Rast, S., Lynn, M. J., Auchus, A. P
.
Pfeiffer, R. F. Autonomic dysfunction in
Parkinson’s disease: a comprehensive symptom
survey. Parkinsonism Relat. Disord. 8, 277–284
(2002).
80. Abbott, R. D. et al. Frequency of bowel
movements and the future risk of Parkinson’s
disease. Neurology 57, 456–462 (2001).
81. Savica, R. et al. Medical records documentation
of constipation preceding Parkinson disease:
a case–control study. Neurology 73, 1752–1758
(2009).
82. Proulx, M., de Courval, F. P
., Wiseman, M. A.
Panisset, M. Salivary production in Parkinson’s
disease. Mov. Disord. 20, 204–207 (2005).
83. Cersosimo, M. G. et al. Hyposialorrhea as an
early manifestation of Parkinson disease.
Auton. Neurosci. 150, 150–151 (2009).
84. Del Tredici, K., Hawkes, C. H., Ghebremedhin, E.
Braak, H. Lewy pathology in the submandibular
gland of individuals with incidental Lewy body
disease and sporadic Parkinson’s disease.
Acta Neuropathol. 119, 703–713 (2010).
85. Edwards, L. L., Quigley, E. M., Harned, R. K.,
Hofman, R. Pfeiffer, R. F. Characterization
of swallowing and defecation in Parkinson’s
disease. Am. J. Gastroenterol. 89, 15–25
(1994).
86. Castell, J. A. et al. Manometric abnormalities
of the oesophagus in patients with Parkinson’s
disease. Neurogastroenterol. Motil. 13, 361–364
(2001).
87. Wakabayashi, K., Takahashi, H., Takeda, S.,
Ohama, E. Ikuta, F. Parkinson’s disease:
the presence of Lewy bodies in Auerbach’s
and Meissner’s plexuses. Acta Neuropathol. 76,
217–221 (1988).
88. Sakakibara, R., Uchiyama, T., Yamanishi, T.,
Shirai, K. Hattori, T. Bladder and bowel
dysfunction in Parkinson’s disease. J. Neural
Transm. 115, 443–460 (2008).
89. Sharabi, Y. Goldstein, D. S. Mechanisms
of orthostatic hypotension and supine
hypertension in Parkinson disease. J. Neurol.
Sci. 310, 123–128 (2011).
90. Winge, K., Skau, A. M., Stimpel, H.,
Nielsen, K. K. Werdelin, L. Prevalence of
bladder dysfunction in Parkinsons disease.
Neurourol. Urodyn. 25, 116–122 (2006).
91. Blackett, H., Walker, R. Wood, B. Urinary
dysfunction in Parkinson’s disease: a review.
Parkinsonism Relat. Disord. 15, 81–87 (2009).
92. Winge, K. Nielsen, K. K. Bladder dysfunction
in advanced Parkinson’s disease. Neurourol.
Urodyn. 31, 1279–1283 (2012).
93. Sakakibara, R., Uchiyama, T., Yamanishi, T.
Kishi, M. Sphincter EMG as a diagnostic tool in
autonomic disorders. Clin.Auton. Res. 19, 20–31
(2009).
94. Seppi, K. et al. Progression of putaminal
degeneration in multiple system atrophy: a serial
diffusion MR study. Neuroimage 31, 240–245
(2006).
95. Feigin, A. et al. Tc‑99m ethylene cysteinate
dimer SPECT in the differential diagnosis of
parkinsonism. Mov. Disord. 17, 1265–1270
(2002).
96. Kwon, K. Y., Choi, C. G., Kim, J. S., Lee, M. C.
Chung, S. J. Comparison of brain MRI and
18
F-FDG PET in the differential diagnosis of
multiple system atrophy from Parkinson’s
disease. Mov. Disord. 22, 2352–2358 (2007).
97. Varrone, A., Marek, K. L., Jennings, D.,
Innis, R. B. Seibyl, J. P
. [123
I]β-CIT SPECT
imaging demonstrates reduced density of
striatal dopamine transporters in Parkinson’s
disease and multiple system atrophy. Mov.
Disord. 16, 1023–1032 (2001).
98. King, A. E., Mintz, J. Royall, D. R. Meta-analysis
of 123
I-MIBG cardiac scintigraphy for the
diagnosis of Lewy body-related disorders.
Mov. Disord. 26, 1218–1224 (2011).
99. Goldstein, D. S., Holmes, C., Cannon, R. O. 3rd
,
Eisenhofer, G. Kopin, I. J. Sympathetic
cardioneuropathy in dysautonomias. N. Engl.
J. Med. 336, 696–702 (1997).
100. Treglia, G. et al. Diagnostic performance
of iodine‑123‑metaiodobenzylguanidine
scintigraphy in differential diagnosis between
Parkinson’s disease and multiple-system atrophy:
a systematic review and a meta-analysis. Clin.
Neurol. Neurosurg. 113, 823–829 (2011).
101.Nagayama, H. et al. Abnormal cardiac
[123
I]‑meta‑iodobenzylguanidine uptake in
multiple system atrophy. Mov. Disord. 25,
1744–1747 (2010).
102.McKeith, I. G. Consensus guidelines for the
clinical and pathologic diagnosis of dementia
with Lewy bodies (DLB): report of the
Consortium on DLB International Workshop.
J. Alzheimers. Dis. 9, 417–423 (2006).
103.Stubendorff, K., Aarsland, D., Minthon, L.
Londos, E. The impact of autonomic dysfunction
on survival in patients with dementia with Lewy
bodies and Parkinson’s disease with dementia.
PLoS ONE 7, e45451 (2012).
104.Kanazawa, M. et al. An autopsy case of
dementia with Lewy bodies showing autonomic
failure and dementia as the initial symptoms.
Mov. Disord. 22, 1212–1213 (2007).
105.Thaisetthawatkul, P
. et al. Autonomic dysfunction
in dementia with Lewy bodies. Neurology 62,
1804–1809 (2004).
106.Leehey, M. A. Fragile X‑associated tremor/ataxia
syndrome: clinical phenotype, diagnosis, and
treatment. J. Investig. Med. 57, 830–836 (2009).
107.Guaraldi, P
. et al. Isolated noradrenergic failure in
adult-onset autosomal dominant leukodystrophy.
Auton. Neurosci. 159, 123–126 (2011).
108.Mead, S. et al. A novel prion disease associated
with diarrhea and autonomic neuropathy. N. Engl.
J. Med. 369, 1904–1914 (2013).
109.Koike, H., Watanabe, H. Sobue, G. The
spectrum of immune-mediated autonomic
neuropathies: insights from the
clinicopathological features. J. Neurol.
Neurosurg. Psychiatry 84, 98–106 (2013).
110.Suarez, G. A., Fealey, R. D., Camilleri, M.
Low, P
. A. Idiopathic autonomic neuropathy:
clinical, neurophysiologic, and follow-up studies
on 27 patients. Neurology 44, 1675–1682
(1994).
111.Gibbons, C. H. Freeman, R. Antibody titers
predict clinical features of autoimmune
autonomic ganglionopathy. Auton. Neurosci. 146,
8–12 (2009).
112.Vernino, S., Cheshire, W. P
. Lennon, V. A.
Myasthenia gravis with autoimmune autonomic
neuropathy. Auton. Neurosci. 88, 187–192
(2001).
113.Peltier, A. C. et al. Coexistent autoimmune
autonomic ganglionopathy and myasthenia
gravis associated with non‑small‑cell lung
cancer. Muscle Nerve 41, 416–419 (2010).
114.Gibbons, C. H., Vernino, S. A. Freeman, R.
Combined immunomodulatory therapy in
autoimmune autonomic ganglionopathy.
Arch. Neurol. 65, 213–217 (2008).
115.Imrich, R., Vernino, S., Eldadah, B. A., Holmes, C.
Goldstein, D. S. Autoimmune autonomic
ganglionopathy: treatment by plasma exchanges
and rituximab. Clin.Auton. Res. 19, 259–262
(2009).
116.Iodice, V. et al. Efficacy of immunotherapy
in seropositive and seronegative putative
autoimmune autonomic ganglionopathy.
Neurology 72, 2002–2008 (2009).
117.Sandroni, P
. et al. Idiopathic autonomic
neuropathy: comparison of cases seropositive
and seronegative for ganglionic acetylcholine
receptor antibody. Arch. Neurol. 61, 44–48
(2004).
118.Lucchinetti, C. F., Kimmel, D. W. Lennon, V. A.
Paraneoplastic and oncologic profiles of patients
seropositive for type 1 antineuronal nuclear
autoantibodies. Neurology 50, 652–657 (1998).
119.Winkler, A. S., Dean, A., Hu, M., Gregson, N.
Chaudhuri, K. R. Phenotypic and neuropathologic
heterogeneity of anti-Hu antibody-related
paraneoplastic syndrome presenting with
progressive dysautonomia: report of two cases.
Clin.Auton. Res. 11, 115–118 (2001).
120.Chinn, J. S. Schuffler, M. D. Paraneoplastic
visceral neuropathy as a cause of severe
gastrointestinal motor dysfunction.
Gastroenterology 95, 1279–1286 (1988).
121.De Giorgio, R. et al. Inflammatory neuropathies
of the enteric nervous system. Gastroenterology
126, 1872–1883 (2004).
122.Colan, R. V., Snead, O. C. 3rd
, Oh, S. J.
Kashlan, M. B. Acute autonomic and sensory
neuropathy. Ann. Neurol. 8, 441–444 (1980).
123.Koike, H. et al. Clinicopathological features of
acute autonomic and sensory neuropathy. Brain
133, 2881–2896 (2010).
124.Pavlakis, P
. P
. et al. Peripheral neuropathies in
Sjögren syndrome: a new reappraisal. J. Neurol.
Neurosurg. Psychiatry 82, 798–802 (2011).
125.Dawson, L., Tobin, A., Smith, P
. Gordon, T.
Antimuscarinic antibodies in Sjögren’s
syndrome: where are we, and where are we
going? Arthritis Rheum. 52, 2984–2995 (2005).
126.Nakamura, Y. et al. High prevalence of
autoantibodies to muscarinic‑3 acetylcholine
receptor in patients with juvenile-onset Sjögren
syndrome. Ann. Rheum. Dis. 67, 136–137
(2008).
127.Park, K., Park, S. Jackson, M. W. The inhibitory
effects of antimuscarinic autoantibodies in the
sera of primary Sjogren syndrome patients on
the gastrointestinal motility. Mol. Immunol. 56,
583–587 (2013).
128.Kondo, T. et al. Autoimmune autonomic
ganglionopathy with Sjögren’s syndrome:
significance of ganglionic acetylcholine receptor
antibody and therapeutic approach. Auton.
Neurosci. 146, 33–35 (2009).
129.Tesfaye, S. et al. Diabetic neuropathies: update
on definitions, diagnostic criteria, estimation of
severity, and treatments. Diabetes Care 33,
2285–2293 (2010).
130.Ziegler, D., Gries, F. A., Spuler, M. Lessmann, F.
The epidemiology of diabetic neuropathy.
Diabetic Cardiovascular Autonomic Neuropathy
Multicenter Study Group. J. Diabetes
Complications 6, 49–57 (1992).
131.Low, P
. A. et al. Autonomic symptoms and
diabetic neuropathy: a population-based study.
Diabetes Care 27, 2942–2947 (2004).
132.England, J. D. et al. Practice Parameter:
evaluation of distal symmetric polyneuropathy:
role of autonomic testing, nerve biopsy, and skin
biopsy (an evidence-based review). Report of the
American Academy of Neurology, American
Association of Neuromuscular and
Electrodiagnostic Medicine, and American
Academy of Physical Medicine and Rehabilitation.
Neurology 72, 177–184 (2009).
REVIEWS
© 2014 Macmillan Publishers Limited. All rights reserved
- 12. 12 | ADVANCE ONLINE PUBLICATION www.nature.com/nrneurol
133.Vinik, A. I. Ziegler, D. Diabetic cardiovascular
autonomic neuropathy. Circulation 115,
387–397 (2007).
134.Maleki, D. et al. Gastrointestinal tract symptoms
among persons with diabetes mellitus in the
community. Arch. Intern. Med. 160, 2808–2816
(2000).
135.Lysy, J., Israeli, E. Goldin, E. The prevalence
of chronic diarrhea among diabetic patients.
Am. J. Gastroenterol. 94, 2165–2170 (1999).
136.Schiller, L. R. et al. Pathogenesis of fecal
incontinence in diabetes mellitus: evidence
for internal‑anal‑sphincter dysfunction. N. Engl.
J. Med. 307, 1666–1671 (1982).
137.Bradley, W. E. Diagnosis of urinary bladder
dysfunction in diabetes mellitus. Ann. Intern.
Med. 92, 323–326 (1980).
138.Kaplan, S. A., Te, A. E. Blaivas, J. G.
Urodynamic findings in patients with diabetic
cystopathy. J. Urol. 153, 342–344 (1995).
139.Bacon, C. G. et al. Association of type and
duration of diabetes with erectile dysfunction
in a large cohort of men. Diabetes Care 25,
1458–1463 (2002).
140.Malavige, L. S. Levy, J. C. Erectile dysfunction
in diabetes mellitus. J. Sex. Med. 6, 1232–1247
(2009).
141. Watkins, P
. J. Facial sweating after food: a new
sign of diabetic autonomic neuropathy. Br. Med. J.
1, 583–587 (1973).
142.Gibbons, C. H. Freeman, R. Treatment-
induced diabetic neuropathy: a reversible
painful autonomic neuropathy. Ann. Neurol. 67,
534–541 (2010).
143.Wang, A. K., Fealey, R. D., Gehrking, T. L.
Low, P
. A. Patterns of neuropathy and autonomic
failure in patients with amyloidosis. Mayo Clin.
Proc. 83, 1226–1230 (2008).
144.Cappellari, M. et al. Variable presentations of
TTR-related familial amyloid polyneuropathy in
seventeen patients. J. Peripher. Nerv. Syst. 16,
119–129 (2011).
145.Rajkumar, S. V., Gertz, M. A. Kyle, R. A.
Prognosis of patients with primary systemic
amyloidosis who present with dominant
neuropathy. Am. J. Med. 104, 232–237 (1998).
146.Gertz, M. A. et al. Stem cell transplantation
for the management of primary systemic
amyloidosis. Am. J. Med. 113, 549–555
(2002).
147.Planté-Bordeneuve, V. Said, G. Familial amyloid
polyneuropathy. Lancet Neurol. 10, 1086–1097
(2011).
148.Said, G. Planté-Bordeneuve, V. TTR-familial
amyloid polyneuropathy—neurological aspects.
Amyloid 19 (Suppl. 1), 25–27 (2012).
149.Arruda-Olson, A. M. et al. Genotype,
echocardiography, and survival in familial
transthyretin amyloidosis. Amyloid 20, 263–268
(2013).
150.Yamashita, T. et al. Long-term survival after liver
transplantation in patients with familial amyloid
polyneuropathy. Neurology 78, 637–643 (2012).
151.Coelho, T. et al. Tafamidis for transthyretin
familial amyloid polyneuropathy: a randomized,
controlled trial. Neurology 79, 785–792 (2012).
152.Robinson-Papp, J., Sharma, S., Simpson, D. M.
Morgello, S. Autonomic dysfunction is
common in HIV and associated with distal
symmetric polyneuropathy. J. Neurovirol. 19,
172–180 (2013).
153.Dutsch, M. et al. Small fiber dysfunction
predominates in Fabry neuropathy. J. Clin.
Neurophysiol. 19, 575–586 (2002).
154.Dib-Hajj, S. D., Cummins, T. R., Black, J. A.
Waxman, S. G. From genes to pain: Nav
1.7 and
human pain disorders. Trends Neurosci. 30,
555–563 (2007).
155.Faber, C. G. et al. Gain of function Nav
1.7
mutations in idiopathic small fiber neuropathy.
Ann. Neurol. 71, 26–39 (2012).
156.Rush, A. M. et al. A single sodium channel
mutation produces hyper- or hypoexcitability in
different types of neurons. Proc. Natl Acad. Sci.
USA 103, 8245–8250 (2006).
157.Han, C. et al. Functional profiles of SCN9A
variants in dorsal root ganglion neurons and
superior cervical ganglion neurons correlate with
autonomic symptoms in small fibre neuropathy.
Brain 135, 2613–2628 (2012).
REVIEWS
© 2014 Macmillan Publishers Limited. All rights reserved