Gingiva. Lilly & Bong.pptx
- 2. CONTENTS Introduction Definition Development of gingiva Macroscopic anatomy Microscopic anatomy Bloodsupply Lymphatic drainage Nerve supply Correlation of clinical and microscopic features Repair/healing of gingiva Age changes Gingival diseases Oral Mucusa- Alveolar Mucosa Clinical considerations Conclusion References
- 4. CARRANZA: Gingiva is the part of oral mucosa that covers the alveolar processes of jaws and surrounds the neck of teeth. LINDHE: Part of masticatory mucosa covering the alveolar processes of the cervical portions of teeth. GLOSSARY OF PERIODONTICS (AAP): The fibrous investing tissue, covered by keratinized epithelium, that immediately surrounds a tooth and is contiguous with its periodontal ligament and with the mucosal tissues of the mouth. DEFINITIONS
- 5. SCHROEDER: It is a combination of epithelium and connective tissue and it defined as that portion of oral mucous membrane, which in complete post eruptive dentition of a healthy young individual surrounds and is attached to the teeth and the alveolar processes. GRANT: Gingiva is the part of oral mucous membrane attached to the teeth and the alveolar processes. GENCO: Gingiva is that part of oral mucous membrane that covers the alveolar processes of the cervical portions of the teeth.
- 6. 6 DEVELOPMENT OF GINGIVA Listgarten,1972 & Mackenzie,1988
- 8. 8 MARGINAL GINGIVA INTERDENTAL GINGIVA ATTACHED GINGIVA MACROSCOPIC ANATOMY Schluger et al, 1990
- 9. 9 9 MARGINAL GINGIVA • Terminal edge surrounding the tooth in collar-like fashion. • 1mm wide. • Free gingival groove (30-40% cases). • Position: 1.5-2mm coronal to CEJ • Gingival zenith Smile designing
- 10. 10 10 • Gingival crevice – Orban & Mueller,1929 • Shallow crevice around the tooth • V- shaped • Significance: Imp. Diagnostic parameter Ideal conditions: 0/ close to 0mm Biologic depth: 1.8mm Probing depth: 2-3 mm
- 11. 11 • Occupies gingival embrasure • Formed by: Lateral borders & tip – marginal gingiva Central intervening portion – attached gingiva • Shape: Pyramidal - Anteriors Col – Posteriors • Diastema: gingiva is firmly bound over bone forming a smooth, rounded surface without interdental papilla. INTERDENTAL PAPILLA
- 12. ATTACHED GINGIVA • Firm, resilient and tightly bound to the underlying periosteum of alveolar bone by connective tissue fibers. • Coronally: marginal gingiva • Apically: palatally-palatal mucosa facially-alveolar mucosa • Mucogingival junction • Stippling • Significance • Width of attached gingiva
- 13. 13 Facial: • Widest in incisor region Maxilla: 3.5 – 4.5 mm Mandible: 3.3 – 3.9 mm • Most narrow adjacent to premolar Maxilla: 1.9 mm Mandible: 1.8 mm Lingual: • Wider in molar region • Narrow in incisor region Increases: by the age of 4yrs supraerupted teeth
- 14. 14 HALL WB, 1982: the width of attached gingiva is determined by subtracting the sulcus or pocket depth from total width of gingiva Total width of gingiva: from MGJ to crest of marginal gingiva ⦿ Methods to determine mucogingival junction: ⚫ 1. Visual method. ⚫ 2. Functional method. ⚫ 3. Visual methods after histochemistry staining.
- 15. How much zone of attached gingiva is necessary to maintain the health of Periodontium? • Lang & Loe,1972: suggested that 2 mm of keratinized gingiva (corresponding to 1 mm attached gingiva in this material) is adequate to maintain gingival health. • Bowers GM,1963: It is possible to maintain clinically healthy gingiva despite a very narrow zone of attachment (less than 1 mm.). • Mehta P et al,2010: width of attached gingiva is not significant to maintain periodontal health in the presence of adequate oral hygiene. • Wennstorm, 1987: the lack of minimum amount of attached Gingiva does not necessarily result in a soft tissue recession. Proper plaque control prevents soft tissue recession, even when it is out of adequate width.
- 16. 16 MICROSCOPIC ANATOMY Histologically, gingiva is composed of : 1. Gingival epithelium 2. Epithelium-connective tissue interface 3. Connective tissue
- 17. GINGIVAL EPITHELIUM – GENERAL ASPECTS : • Continuous lining of stratified squamous epithelium. • Function: Physical barrier to Infection Participate actively in responding to infection in signaling further host reactions in integrating innate and acquired immune responses. To protect deep structures Allow a selective interchange with the oral environment.
- 18. • Layers of stratified squamous epithelium as seen by electron microscopy:
- 19. Stratum basale: • Cells: cylindric or cuboid. • Found immediately adjacent to the connective tissue separated by a basement membrane. • Germinative layer: having the ability to divide. • It takes approximately 1 month for a keratinocyte to reach the outer epithelial surface, where it is shed from the stratum corneum.
- 20. Stratum spinosum: • Prickle cell layer. • Large polyhedral cells with short cytoplasmic processes. • Keratinosomes or odland bodies: Modified lysosomes. stratum Present in the uppermost part of the spinosum. Contain a large amount of acid phosphatase.
- 21. Stratum granulosum: • Flattened cells, in a plane parallel to the gingival surface. • Keratohyaline granules : • Associated with keratin formation are 1 μm in diameter) round in shape and appear in the cytoplasm of the cell.
- 22. Stratum corneum: • Closely packed, flattened cells that have lost nuclei and most other organelles as they become keratinized. • The cells are densely packed with tonofilaments. • Clear, rounded bodies probably representing lipid droplets appear within the cytoplasm of the cell.
- 23. Proliferation through mitosis occurs in the basal layer , less frequently in the suprabasal layer and migration occurs. Differentiation includes keratinisation in which main morphologic changes seen are: to the production of • Progressive flattening of the cell. • Increased prevalence of tonofilaments. • Intercellular junctions coupled keratohyaline granules. • Disappearance of the nucleus
- 24. • Three types of surface keratinization can occur in the gingival epithelium: 1. Orthokeratinization 2. Parakeratinization 3. Nonkeratinization
- 25. • Complete keratinization superficial horny layer. • No nuclei in stratum corneal layer. • Well-defined stratum granulosum. • Few areas of outer gingival epithelium. ORTHOKERATINIZATION:
- 26. PARAKERATINIZATION: • Intermediate stage of keratinization. • Most prevalent surface area of the gingival epithelium. • Can progress to maturity or de- differentiate under different physiologic or pathologic conditions. • Stratum cornea retains PYKNOTIC NUCLEI. • Keratohyaline granules are dispersed rather than giving rise to a stratum granulosum.
- 27. NONKERATINIZATION: • Viable nuclei in superficial layer. • Has neither granulosum nor corneum strata. • Layers of nonkeratinized epithelium: 1. Stratum superficiale 2. Stratum intermedia 3. Stratum basale
- 28. ULTRASTRUCTURE OF EPITHELIUM: • Each epithelial type have characteristic pattern of cytokeratins. • Keratin proteins are composed of different polypeptide subunits characterized by their isoelectric points and molecular weights. • Basal cells begin synthesis of low mol. Wt. keratins. Ex.: K19 (40kD). • High mol. Wt. keratins are expressed when they reach superficial layers. Ex.: K1 (68kD).
- 29. • Other proteins synthesized during maturation proess: Keratolinin Involucrin Filaggrin • Corneocyte: Most differentiated epithelial cell Composed of bundles of keratin tonofilaments in amorphous matrix of filaggrin, surrounded by a resistant envelope made of keratolinin and involucrin. • These histochemical patterns change under normal or pathologic stimuli, thereby modifying the keratinization process.
- 30. EPITHELIAL CELL CONNECTIONS: • Together with intercellular protein-carbohydrate complexes, cohesion between cells is provided by numerous structures called “DESMOSOMES”. • DESMOSOMES: Located between the cytoplasmic processes of adjacent cells. Two hemidesmosomes facing each other. Large number of desmosomes gives a solid cohesion between cells.
- 31. A desmosome comprises the following structural components: 1. the outer leaflets (OL) of the cell membrane of two adjoining cells, 2. the thick inner leaflets (IL) of the cell membranes 3.the attachment plaques (AP), which represent granular and fibrillar material in the cytoplasm.
- 32. • TONOFILAMENTS: Cytoskeleton of keratin proteins which radiate in brush like fashion from the attachment plaques into cytoplasm of the cells. • TIGHT JUNCTIONS (ZONAE OCCLUDENS): Rarely observed forms of epithelial cell connections where the membranes of the adjoining cells are believed to be fused
- 33. ULTRASTRUCTURE OF EPITHELIAL CELL: • Cytoplasmic organelle concentration varies among different epithelial layers. • Mitochondria, endoplasmic reticulum, golgi complexes etc are more numerous in deeper strata and decrease towards the surface. • Cytokeratins increase in number from basale to corneal layers.
- 35. CELLS PRESENT IN GINGIVAL EPITHELIUM: KERATINOCYTES NONKERATINOCYTES/CLEAR CELLS: Langerhans cells Merkel cells Melanocytes Inflammatory cells
- 36. • 90% of the total gingival cell population. • Originate from ectodermal germ layer. • Cell organelles: nucleus, cytosol, ribosomes, Golgi apparatus etc • Melanosomes: Pigment bearing granules • Proliferation and differentiation of the keratinocytes helps in the barrier action of the epithelium. KERATINOCYTES
- 37. • Move from basal to superficial layers of the epithelium as the process of differentiation occurs, forming a keratin barrier. • The microfilaments present in the keratinocytes help in cell motility and maintenance of the polarity.
- 38. The various nonkeratinocytes are : • Langerhans cells, • Merkel cells, • Melanocytes, • Inflammatory cells NON-KERATINOCYTES/CLEAR CELLS:
- 39. • Dendritics cells - Modified monocytes belonging to RES. • Paul Langerhans used gold impregnation technique to visualize LCs. • Reside chiefly in suprabasal layers. • Act as antigen -presenting cells for lymphocytes. • Specific elongated g-specific granules called as Birbecks Granules. • Have marked adenosine triphosphatase activity. • Only epidermal cells which express receptors for C3 and Fc portion of IgG. • Can move in and out of the epithelium unlike melanocytes. • Found in oral ep. of normal gingiva. • Smaller amounts in sulcular ep. • Absent in healthy junctional ep. Langerhans cells:
- 40. Merkel Cells: • Located in deeper layers of epithelium. • Not dendritic cells • Possess keratin tonofilaments and desmosomes. • Harbor nerve endings. • Sensory in nature - respond to touch – Tactile Perceptors
- 41. Melanocytes: • Originate from neural crest cells. • Found in the stratum basale. • Identified in gingiva by Laidlaw and Cahn, 1932. • Have long dendritic processes, interspersed between the keratinocytes. • Lack tonofilaments and desmosomal connections. • Synthesize melanin, responsible for providing color to gingiva. • Melanin is synthesized in organelle called premelanosomes/melanosomes, which are transported along microtubules and actin filaments to the cell periphery. • Melanophores/Melanophages.
- 42. TYPES OF GINGIVAL EPITHELIUM Oral or outer epithelium Sulcular epithelium Junctional epithelium 2mm
- 43. ORAL OR OUTER EPITHELIUM • Covers the crest and outer surface of the marginal gingiva and the surface of the attached gingiva. • 0.2 to 0.3 mm in thickness. • Keratinized or parakeratinized, or it may present combinations of these conditions. • The oral epithelium is composed of four layers.
- 44. • K1, K2, K10-12 cytokeratins present are immunohistochemically expressed with high intensity in orthokeratinized areas and with less intensity in parakeratinized areas. • K6 and K16 , characteristic of highly proliferative epithelia. • K5 and K14, stratification-specific cytokeratins , also are present
- 45. SULCULAR EPITHELIUM • Lines the gingival sulcus. • Thin, nonkeratinized stratified squamous epithelium • No rete pegs. • Extends from the coronal limit of the junctional epithelium to the crest of the gingival margin. • Hydropic degeneration of cells. • Contains K4 and K13, K19. • Don’t have merkel cells.
- 46. Sulcular epithelium has the potential to keratinize: • If it is reflected and exposed to the oral cavity. • If the bacterial flora of the sulcus is totally eliminated. Outer epithelium loses its keratinization: • When it is placed in contact with the tooth. These findings suggest that the local irritation of the sulcus prevents sulcular keratinization. Sulcular epithelium is extremely important because it act as a semi permeable membrane through which injurious bacterial products pass into gingival fluid. Less permeable than JE.
- 47. JUNCTIONAL EPITHELIUM • Collarlike band of stratified squamous non-keratinizing epithelium. • 3 to 4 layers thick in early life, but the number increases with age to 10 or even 20 layers. • Tapers from end to apical the its coronal located junction at in healthy termination, cementoenamel tissue. • Length: 0.25 to 1.35 mm.
- 48. • These cells can be grouped in two strata: The Basal layer: that face s the connective tissue (External Basal Lamina) • the suprabasal layer: that extends to the tooth surface- DAT Cells (Internal basal lamina) • 3 zones of junctional epithelium: 1. Apical – germination 2. Middle – adhesion 3. Coronal- permeable.
- 49. THE DENTOGINGIVAL UNIT: • The attachment of the junctional epithelium to the tooth is reinforced by the gingival fibers, which brace the marginal gingiva against the tooth surface. • For this reason, the junctional epithelium and the gingival fibers are considered together as a functional unit.
- 50. Hypothesis given to explain mode of attachment of epithelium to tooth surface: 1. Gottlieb: gingiva is organically united to surface of enamel. He termed it as epithelial attachment. (drawback- did not explain how exactly it attaches.) 2. Waerhaug : in 1952 presented a concept of epithelial cuff, he concluded that gingival tissues are closely adapted but not organically united. 3. Stern: in 1962 showed the attachment to tooth is through hemidesmosomes, supported by schroeder and listgarten.
- 51. Unique structural and functional features of JE that contribute to preventing pathogenic bacterial flora from colonizing the subgingival tooth surface: First, Firmly attached to the tooth surface forming an epithelial barrier against plaque bacteria. Second, Allows access of gingival fluid, inflammatory cells, and components of the immunologic host defense to the gingival margin. Third, Exhibits rapid turnover contributing to the host–parasite equilibrium and the rapid repair of damaged tissue. Have an endocytic capacity equal to that of macrophages and neutrophils and that this activity may be protective in nature.
- 52. Development/Origin of Junctional Epithelium REE surrounds the crown of tooth from the moment enamel is properly mineralized till the tooth erupts . Migratingepithelium produces an epithelial mass between oral epithelium and REE so thattooth can erupt without bleeding. When tooth has penetrated in oral cavity large portions immediately apical to incisal area of enamel are covered by junctional epithelium containing few layers of cell. Duringlater phases of tooth eruption all cells of REE is replaced by JE.
- 53. JE Functions: • Provides attachment to the tooth. • Forms an epithelial barrier against the plaque bacteria. • Rapid cell division and funneling of cells towards the sulcus: Hinder bacterial colonization and Repair of damaged tissue occurs rapidly. • Allow GCF: From connective tissue into crevice – Gingival fluid exudates, PMNs,etc. From crevice to connective tissue – Foreign material such as carbon particles, • Produces active antimicrobial substances like defensins, lysosomal enzymes, calprotectin and cathelicidin. • Epithelial cells activated by microbial substances secrete chemokines, e.g. IL-1, IL-6, IL- 8 and TNF that attract and activate professional defense cells such as lymphocytes and PMNs.
- 55. • Represented as either as transudate or an exudate. • Diagnostic or prognostic biomarker of the biologic state of the periodontium in health and disease. • GCF flow increases during inflammation and resembles that of inflammatory exudates. • Gingival fluid diffuses through the basement membranes. GINGIVAL CREVICULAR FLUID
- 56. • Functions: Cleanse material from the sulcus. Contain plasma proteins that may improve adhesion of epithelium to the tooth Possess antimicrobial properties Expert antibody activity to defend the gingiva. GINGIVAL CREVICULAR FLUID
- 57. Epithelium—Connective Tissue Interface • Ultrastructurally the interface is composed of 4 elements: • Basal cell plasma membrane. • Lamina lucida: 25 to 45 nm wide. • Lamina densa: 40 to 60 nm thickness. • Reticular layer. • From the lamina densa so called anchoring fibrils project in a fan- shaped fashion into the connective tissue.
- 58. Various junctional complexes present in gingiva are: • Tight junctions/Zonae occludens • Adhesive junctions: Cell to cell – Zonula adherens – Desmosomes: 30 nm. Cell to matrix – Focal adhesions – Hemidesmosomes • Gap junctions: Intercellular pipes/channels bridge both adjacent membranes and intercellular space. Intercellular space in gap junction is approx. 3 nm. Major pathway for direct intercellular communication.
- 60. CONNECTIVE TISSUE • The predominant tissue component of gingiva – Lamina Propria. • Components: Collagen fibers (60%) Fibroblasts (5%) Vessels, Nerves & Matrix (35%) • Layers of connective tissue: 1. Papillary Layer 2. Reticular Layer
- 61. GROUND SUBSTANCE: • Fills space between fibers and cells • Amorphous • High water content • Composed of: Proteoglycans: Hyaluronic acid Chondroitin sulphate Glycoproteins: (PAS positive) Fibronectin Laminin
- 62. CELLS: The different types of cell present in the connective tissue are: Fibroblasts Mast cells Fixed Macrophages & Histiocytes Inflammatory cells (Plasma cells, Lymphocytes, Neutrophils) Adipose cells Eosinophils
- 63. Fibroblasts: • Preponderant cellular element in the gingival connective tissue. • Mesenchymal origin. • Play a major role in the development, maintenance, and repair of gingival connective tissue. Synthesize: Collagen, elastic fibers, glycoproteins and glycosaminoglycan • Regulate collagen degradation through phagocytosis and the secretion of collagenases. • Fibroblast heterogeneity is now a well-established feature of fibroblasts in the periodontium which is necessary for the normal functioning of tissues in health, disease, and repair
- 64. GINGIVAL FIBERS: The connective tissue fibers are produced by the fibroblasts and can be divided into: • Collagen fibers • Reticulin fibers • Oxytalan fibers • Elastic fibers..
- 65. Collagen type I: forms the bulk of the lamina propria provides the tensile strength to the gingival tissue. Type IV collagen: branches between the collagen type I bundles continuous with fibers of the basement membrane and the blood vessel walls. Densely packed collagen bundles that are anchored into the acellular extrinsic fiber cementum just below the terminal point of the junctional epithelium form the connective tissue attachment. The stability of this attachment is a key factor in the limitation of the migration of junctional epithelium.
- 66. Reticulin fibres: •Have argyrophilic property and are numerous in tissue adjacent to basement membrane. • Found in large number in loose CT surrounding blood vessel • Hence found in endothelial-CT and epithelium-CT interface. Elastic fibres: • Only present in association with blood vessels. •Gingiva seen coronal to mucogingival junction has no elastic fibres except in assocation with blood vessels. • Alveolar mucosa may have many elastic fibres. Oxytalan fibres. • Initially described by Fullmer. • Modified type of elastic fibres. • Scarce in gingiva but more in PDL. • Have thin fibrils with 150 A0 dia.
- 67. Gingival Fibers: • The connective tissue of the marginal gingiva is densely collagenous, and it contains a prominent system of collagen fiber bundles called the gingival fibers. • These fibers consist of type I collagen. • Functions: To brace the marginal gingiva firmly against the tooth To provide the rigidity necessary to withstand the forces of mastication without being deflected away from the tooth surface To unite the free marginal gingiva with the cementum of the root and the adjacent attached gingiva
- 68. The gingival fibers are arranged in three groups: 1. Gingivodental 2. Circular 3. Transseptal According Page et.al: Semicircular fibers: Transgingival fibers Lindhe: Dentoperiosteal fibers
- 69. • Originates from cementum and spreads laterally into lamina propria Dentogingival • Orginates from periosteum and spreads into lamina propria Alveologingival • Originates from cementum near CEJ into periosteum of alveolar crest Dentoperiosteal • Originates from within the free marginal and attached gingiva coronal to alveolar crest and encircles each tooth Circular • Originates from interproximal cementum coronal to crest and courses mesially and distally in the interdental area into cementum of adjacent teeth Transseptal
- 70. •Originates from the periosteum of the lateral aspect of alveolar process and spreads into attached gingiva. Periosteogingival •Originates from within interdental gingiva and follows on orofacial course Interpapillary •Originates within the attached gingiva interwing along dental arch between and around teeth Transgingival •Originates from cementum on distal surface of tooth spreading buccally and lingually around adjacent tooth and inserting on mesial cementum of next tooth Intercircular •Originates from attached gingiva immediately subjacent to basement membrane and courses mesiodistally Intergingival •Originates from cementum of the mesial surface of tooth and courses distally and inserts on the cementum of distal surface of same tooth Semicircular
- 71. 71 A. Dentogingival plexus B. Subepithelial plexus BLOOD SUPPLY
- 73. NERVE SUPPLY Sublingual nerve Superior labialbranches from infraorbital nerve Sphenopalatine nerve Meissner type tactile corpuscles Krause –type end bulbs Encapsulated spindles
- 74. CORRELATION OF CLINICAL AND MICROSCOPIC FEATURES
- 75. • Generally coral pink. • Color is a result of: Vascular supply Thickness Degree of keratinisation of epithelium, Presence of pigment containing cells. • Color to be correlated with cutaneous pigmentation Color:
- 76. Physiologic Pigmentation(melanin) • Melanin (non hemoglobin derived brown pigment) • Prominent in blacks, diminished in albinos • Distribution of Oral Pigmentations in blacks: Gingiva -60% Hard Palate -61% Mucous membrane -22% Tongue -15% • As a diffuse , deep purplish discoloration or as irregularly shaped brown and light brown patches and may appear as early as 3 hours after birth.
- 77. Synthesis of Melanin pigmentation • Tyrosine is hydroxylated into DOPA in presence of Tyrosinase enzyme. • DOPA (Dihydroxy Phenylalanine) is converted into Melanin • Melanin is phagocytosed to become Melanophages or Melanophores.
- 78. • Sum total of the bulk of cellular and intercellular elements and their vascular supply. • Alteration in size is a common feature of gingival disease Size
- 79. Contour • Marginal gingiva envelops the teeth in collarlike fashion and follows a scalloped outline on the facial and lingual surfaces. • straight line - along teeth with relatively flat surfaces. • accentuated - pronounced mesiodistal convexity (e.g., maxillary canines) or teeth in labial version • horizontal and thickened - in lingual version.
- 80. The shape of the interdental gingiva is governed by the contour of the proximal tooth surfaces and the location and shape of the gingival embrasures. Anterior region of the dentition, the interdental papilla is pyramidal in form. the papilla is more flattened in a buccolingual direction in the molar region. Shape.
- 81. • Shape depends on: Presence/absence of contact Distance btw contact point and osseous crest Course of CEJ Width of the approximate tooth surfaces Presence/absence of recession.
- 82. Consistency • Firm and resilient • Collagenous nature of the lamina propria and its contiguity with the mucoperiosteum determine the firmness of the attached gingiva. • The gingival fibers contribute to the firmness of the gingival margin. • If the gingiva is suppressed, the proteoglycans become deformed and recoil when the pressure is eliminated. • Thus, the macromolecules are important for the resilience of the gingiva.
- 83. • Orange peel – stippled, • Stippling is best viewed by drying Gingiva. • Attached Gingiva is stippled, marginal gingival is not. • Central portion of interdental papilla is usually stippled, but marginal borders are smooth. • Less prominent on lingual surfaces and may be absent in some. Surface Texture
- 84. • Stippling –produced by alternate round protuberance and depressions in the gingival surface. • Low magnification ; a stippled surface, • Higher magnification; cell micropits • A form of adaptive specialization or reinforcement for function –feature of healthy gingiva
- 85. • Reduction of stippling – common sign of Gingival disease. • Stippling returns when gingiva is restored to health. • Keratinisation – protective adaptation , increased by tooth brushing. • In 40% of adults Gingiva show stippling. • Generalized absence of stippling is seen in: Infancy Diseased conditions like gingival enlargements, mucocutaneous lesions affecting gingiva, inflammation etc.,
- 86. Position • The level at which the gingival margin is attached to the tooth. • Continuous eruption, even after meeting their functional antagonists occurs through out life Active Eruption :Movement of teeth in the direction of occlusal plane Passive Eruption: exposure of the tooth by apical migration of Gingiva • Gottlieb : active and passive eruption go hand in hand. • Active eruption is coordinated with attrition, to compensate for tooth substance worn away. • Attrition reduces the clinical crown and prevents it from becoming disproportionately long in relation to the clinical root, thus avoiding excessive leverage on periodontal tissue. • Rate of active eruption is in pace with tooth wear in order to preserve vertical dimension.
- 88. • Exposure of the tooth via the apical migration of the gingiva is called gingival recession or atrophy. • According to the concept of continuous eruption, the gingival sulcus may be located on the crown, the cementoenamel junction, or the root, depending on the age of the patient and the stage of eruption. • Therefore, some root exposure with age would be considered normal and referred to as physiologic recession. • Again, this concept is not accepted at present. • Excessive exposure is termed pathologic recession
- 89. REPAIR/HEALING OF GINGIVA • Turnover rate is 10-12 days. • It is one of the best healing tissues in the body with little or no scarring. • However the reparative capacity is lesser than that of periodontal ligament and epithelial tissue.
- 90. AGE CHANGES Stippling usually disappears with age. Width of the attached gingiva increases with age. a. Gingival epithelium: • Thinning and decreased keratinization • Rete pegs flatten • Migration of junctional epithelium apically. • Reduced oxygen consumption. b. Gingival connective tissue: • Increased rate of conversion of soluble to insoluble collagen • Increased mechanical strength of collagen • Increased denaturing temperature of collagen • Decreased rate of synthesis of collagen • Greater collagen content.
- 91. GINGIVAL DISEASES Gingivitis associated with dental plaque only Gingival diseases modified by systemic factors Gingival diseases modified by medications Gingival diseases modified by malnutrition DENTAL-PLAQUE– INDUCED GINGIVAL DISEASES
- 92. Gingival diseases of specific bacterial origin Gingival diseases of viral origin Gingival diseases of fungal origin Gingival lesions of genetic origin Gingival manifestations of systemic conditions Traumatic lesions Foreign-body reactions Not otherwise specified NONPLAQUE INDUCED GINGIVAL DISEASES
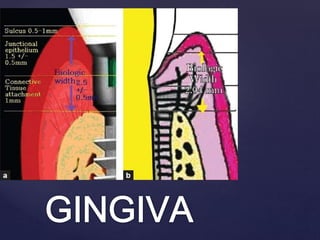
- 93. CLINICAL CONSIDERATIONS • The biological width is defined as the dimension of the soft tissue, which is attached to the portion of the tooth coronal to the crest of the alveolar bone. • Gargiulo et al.,: • Established that there is a definite proportional relationship between the alveolar crest, the connective tissue attachment, the epithelial attachment, and the sulcus depth. BIOLOGICAL WIDTH
- 94. • They reported the following mean dimensions: A sulcus depth of 0.69 mm, (a) an epithelial attachment of 0.97 mm,(b) connective tissue attachment of 1.07 mm.(c) The biologic width is commonly stated to be 2.04 mm,(b+c) which represents the sum of the epithelial and connective tissue measurements.
- 95. Biologic Width Evaluation: 1. Clinical (discomfort when the restoration margin levels are being assessed with a periodontal probe) 2. Radiographs (for interproximjal violation but mesiofacial and distofacial line angle not seen properly) 3. Bone sounding (probing under anesthesia) If this distance is less than 2 mm or more at one or more locations, a diagnosis of biologic width violation can be confirmed Biologic width violation: • Unpredictable bone loss • Gingival recession • Persistence of ginigivitis
- 96. GINGIVAL BIOTYPE • Gingival biotype is described as the thickness of the gingiva in the faciopalatal/ faciolingual dimension. • Seibert and Lindhe categorized the gingiva into: 1. thick-flat: A gingival thickness of ≥ 2 mm 2. thin scalloped: a gingival thickness of <1.5 mm • Significant impact on the outcome of the restorative, regenerative and implant therapy. • Direct co-relation exists with the susceptibility of gingival recession followed by any surgical procedure.
- 97. Thick blunted: Resists recession reacts to surgical & restorative insults with pocket formation Thin scalloped: Attached soft tissue is minimal Bony dehiscence & fenestration defects Reacts to surgical or restorative interventions with ST recession, apical migration of attachment & loss of underlying alveolar volume .
- 98. Three primary types of oral mucosa: 1. lining mucosa 2. masticatory mucosa 3. specialized mucosa. Of the types of lining mucosa, there are three kinds: alveolar mucosa, labial mucosa, and buccal mucosa. Oral Mucosa Source: www.icoi.org glossary
- 99. Alveolar mucosa is the soft, thin mucous membrane that sits above the marginal gingiva and the attached gingiva, and continues across the floor of the mouth, cheeks, and lips. It is bright red in color due to being rich with blood vessels, and is shiny and smooth in appearance. it is made up of nonkeratinized stratified squamous epithelium, making it delicate and sometimes difficult to work with. In oral implantology, it’s crucial to keep the alveolar mucosa intact, particularly when implants are done in the front of the mouth. Disruption of the alveolar mucosa can impact the aesthetic results of the procedure, leading to implant failure. The buccal flap should be made carefully so as to keep the alveolar mucosa intact.
- 100. 99 • Clinical Periodontology By Carranza, 12th Edition • Clinical Periodontology And Implant Dentistry By Jan Lindhe, 4th Edition. • Biology Of Periodontal Connective Tissue-bartold And Sampath Narayana • Oral Histology, Development, Structure And Function – A.R. Tencate, 5th Edition • PERIODONTICS REVISITED Shalu Bathla, 1st Edition REFERENCES
- 101. • Gingival tissues play a key role in the protection of tooth structures and supporting periodontal tissues against trauma and/or infection • Making the gingival health, a very essential component for the success of all periodontal treatment procedures. • Therefore, Gingiva, a small tissue is a big issue for the fraternity of periodontics. CONCLUSION
- 102. • Babita Pawar, Pratishtha Mishra, Parmeet Banga, and P. P. Marawar. Gingival zenith and its role in redefining esthetics: A clinical study. J Indian Soc Periodontol. 2011 Apr-Jun; 15(2): 135–138. • Niklaus P. Lang, and Harald Löe. The Relationship Between the Width of Keratinized Gingiva and Gingival Health. J Periodontol. 1972 Oct;43(10):623-7. • Gerald M. Bowers. A Study of the Width of Attached Gingiva. Journal of Periodontology,May 1963, Vol. 34, No. 3, Pages 201-209 • Wennström JL. Lack of association between width of attached gingiva and development of soft tissue recession. A 5-year longitudinal study. J Clin Periodontol. 1987 Mar;14(3):181-4
- 103. • Mehta P, Lim LP. The width of the attached gingiva--much ado about nothing? J Dent. 2010 Jul;38(7):517-25. • Molecular and Cell Biology of the Gingiva, Periodontology 2000; Vol 24; 2000; 28-55.