CVM_Lect-1-9.pptx
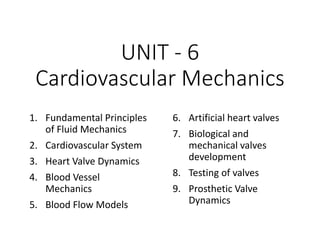
- 1. UNIT - 6 Cardiovascular Mechanics 1. Fundamental Principles of Fluid Mechanics 2. Cardiovascular System 3. Heart Valve Dynamics 4. Blood Vessel Mechanics 5. Blood Flow Models 6. Artificial heart valves 7. Biological and mechanical valves development 8. Testing of valves 9. Prosthetic Valve Dynamics
- 2. Fundamental Principles of Fluid Mechanics
- 3. Conservation Laws • Blood flow must obey the principles of conservation of mass, momentum, and energy. • Applied to any given region of space, the principle of conservation of mass means that whatever flows in must flow out. • If flow is confined to blood vessels, then we obtain a rule similar to Kirchhoff's law of electric circuits: • At any junction the summation of current flowing into a junction must be equal to the sum of the currents flowing out of that junction. • In a single tube of variable cross section, a steady flow implies that the average local speed of flow is inversely proportional to the local cross sectional area.
- 4. Conservation Laws • Conservation of momentum means that the momentum of matter cannot be changed without the action of force. • If there is force acting on a body, then according to the Newton's law of motion, the rate of change of momentum of the body is equal to the force.
- 5. Reynolds Transport Theorem • The Reynolds Transport Theorem is a generalisation of the principles of mass and momentum conservation. • A conserved quantity in the system is one whose rate of change we can quantify in terms of other physical effect.
- 6. Pressure gradient & divergence of shear stresses
- 7. Pressure gradient & divergence of shear stresses a) shows a small rectangular element of blood subjected to equal pressure on all sides. The element remains in equilibrium. b) Shows an element subjected to shear stresses that are equal on all sides. Because the shear stresses are equal in this case, the fluid element will be distorted by the shear stresses, but there will be no tendency to accelerate. c) shows a steady laminar flow of a fluid in a tube. The velocity distribution is indicated on the left. To the right, a series of fluid elements is shown. The shear stresses acting on these elements are indicated by arrows, with the magnitude proportional to the length.
- 8. Types of fluids • We categorise fluids according to the nature of the relationship between the stress tensor and the strain tensor: • Newtonian fluids obey a stress–strain relationship of the form σ = 2µε − ρI • Where, ρ is the pressure, ε is the strain tensor and µ is the viscosity (which is constant), • Inviscid fluids obey σ = − ρI • while other fluids have a more complicated relationship between the stress and strain tensors, which may depend on the history of the fluid motion, as well as the current state.
- 9. Newton's Law of Motion • Newton's law states that Mass x acceleration= force • Applied to a fluid, it takes the following form, which will be explained in detail below: Density x (transient acceleration + convective acceleration) = - pressure gradient + divergence of normal and shear stresses i.e. viscous stresses per unit volume Navier–Stokes equation
- 10. Flow of Fluid • Flow is defined by the field of velocity vectors of all particles in a domain. • It is said to be steady if the velocity field is independent of time. • It is unsteady if the velocity field varies with time.
- 11. Laminar & Turbulent Flow • It is turbulent if the velocity field is stochastic, that is, if the velocity components are random variables described by their statistical properties. • A turbulent flow contains small eddies within large eddies, and smaller eddies within small eddies, ad infinitum. • A laminar flow is one that is not turbulent.
- 12. Flow Profile
- 13. Laminar & Turbulent Flow Laminar Flow • A parabolic flow profile. • Low shear strain rate • Coefficients of friction or viscosity is low • Molecular motion between the sliding cylinders Turbulent Flow • A profile that is much blunter at the central portion of the tube and much sharper at the wall. • High shear strain rate • Coefficients of friction or viscosity is high • the molecular transport • the convection of the turbulent "eddies"
- 14. Laminar (Poiseuille) Flow • Assumptions of Poiseuille flow • Flow is axisymmetric • Flow is fully developed and the vessel is rigid with a uniform cross-section • Vessel is straight • Flow is steady • Artery is large enough that a Newtonian fluid model is appropriate
- 15. 1. Non-axisymmetric flow • To derive Poiseuille flow, we assumed the flow was axisymmetric. However, this need not be the case, as there are other solutions of the equations with broken symmetry. However, these are only observed for high Reynolds numbers, when the flow becomes turbulent. • Another reason for the flow to become non- axisymmetric is if the pipe is not perfectly circular.
- 16. 1. Non-axisymmetric flow • Reynolds number: This is a dimensionless quantity used to describe a fluid flow. It is probably the most widely used dimensionless number in fluid mechanics. It is defined by • where • ρ is the fluid density, • U is a characteristic velocity scale, • L is a characteristic length scale, and • µ is the viscosity of the fluid. • The Reynolds number gives a qualitative description of the flow, and is an order-of-magnitude estimate. The precise value is usually not important. • For example, when describing the flow, the difference between a flow with Re = 60 and one with Re = 80 is often unimportant, but the difference between one with Re = 100 and Re = 1000 is important.
- 17. 2. Non-fully-developed flow • Arteries are usually long compared with their diameter and have a regular cross-section, so the assumption of fully developed flow is often reasonable. However: • The cross-section may not be constant along the pipe, for example due to: • Arterial taper, which tends to occur in most arteries. • Elasticity in the arterial walls cause the cross-sectional area to change in response to a change in pressure, resulting in non-uniformities in the cross-section along the pipe.
- 18. 2. Non-fully-developed flow • There may be entrance effects due to a change in the vessel, for example: • Flow in the ascending aorta is unlikely to be fully developed, since it is affected by the profile as it leaves the ventricle. • Flow in a daughter artery just after a bifurcation is affected by the splitting of the flow in the parent vessel. • Entrance effects persist for a distance proportional to a Re, where a is the radius of the artery and Re is the Reynolds number.
- 19. 3. Effect of arterial curvature on the flow • The derivation of Poiseuille flow assumes the artery is straight. • In reality, most arteries are curved, which has a significant effect on the flow structure. • It is still possible to gain some insight using analytical techniques in the case when the centreline of the artery (the locus of centres of cross-sections of the pipe) is circular.
- 20. 3. Effect of arterial curvature on the flow
- 21. 4. Effect of unsteadiness in the flow • Flow in the cardiovascular system is not steady, but is rather highly pulsatile. This is illustrated in the graph below, which shows pressure and flow in the aorta.
- 22. 4. Effect of unsteadiness in the flow • Slow oscillations of the pressure gradient • When the oscillations in the pressure gradient are sufficiently slow, there is enough time for Poiseuille flow to develop, meaning the profile at any fixed time looks like the Poiseuille flow solution with the same pressure gradient.
- 23. 5. Unsteady flow: High-frequency oscillations • In this case, we cannot neglect the time-derivative term in the Navier–Stokes equations. • We still assume: • Flow is axisymmetric • Flow is in the axial direction • Flow is fully developed (independent of z)
- 24. 5. Non-Newtonian flow • The blood is a Newtonian fluid. Newtonian fluids have a stress–strain relationship of the form σ = 2µε − ρI
- 25. 5. Non-Newtonian flow • Deformation of cells: As they flow along the arteries, the red blood cells deform significantly, meaning that a rigid-particle model to describe them is probably inaccurate. In order to pass through the narrow capillaries the cells adopt a completely different shape. • Particulate nature of cells: The cells have diameter of around 8 µm, and in small vessels this is a substantial proportion of the vessel diameter. In the capillaries it may be larger than the vessel diameter. With such relatively large particles in a small vessel, a continuum model may not be justified.
- 26. 5. Non-Newtonian flow • Observed shapes adopted by red cells when travelling through a glass capillary of diameter 7 µm. • The differences between the shapes of the three cells are thought to be due to the position of the cell within the capillary. • The pictures are reproduced well by a mathematical model: • To obtain a similar configuration to that in the top picture the cell is placed symmetrically. • To obtain the middle picture the cell is offset by 0.5 µm towards the top. • Finally to obtain the bottom picture the cell in the model is offfset by 1 µm.
- 27. Importance of Flow Analysis • Turbulence in blood flow is strongly implicated in atherogenesis. Atherosclerotic plaques are often found at sites of turbulence in the aorta. • Associated with the velocity fluctuations in a turbulent flow are pressure fluctuations. Pressure fluctuations can excite vibrations in the eardrum and cochlea, and can be heard if the frequencies are in the audible range. We can hear the howling of wind because wind is turbulent. We can hear jet noise if the jet flow is turbulent. • The Korotkoff sound at systole is the sound of the jet noise of rushing blood. A heart murmur is a turbulent noise. Flow separation at a site of stenosis in an artery often causes turbulence in the separated region, making it possible to detect a stenosis by listening to the noise (bruit) in the blood flow with a stethoscope.
- 28. Deceleration as a Generator of Pressure Gradient • If there is no turbulence and if the gravitational and frictional forces are small enough to be ignored, Density x acceleration = -pressure gradient
- 30. ANATOMY OF HEART
- 32. Pressure – Volume Loop A plot of the pressure and volume in a ventricle during a cardiac cycle
- 33. Heart Valves
- 35. Principle of Heart Valve Closure
- 36. Principle of Heart Valve Closure • The mitral valve is composed of two very flexible, thin membranes. These membranes are pushed open at a stage of diastole when the pressure in the left atrium exceeds that of the left ventricle. • Then a jet of blood rushes in from the left atrium into the left ventricle, impinges on the ventricular wall, and is broken up there. • Thus, the blood stream is decelerated in its path and a positive pressure gradient is created.
- 37. Principle of Heart Valve Closure • Toward the end of diastole, the pressure acting on the ventricular side of the mitral valve membranes becomes higher than that acting on the side of the membranes facing the left atrium. • The net force acts to close the valve. In a normal heart, closure occurs without any backward flow or regurgitation. • The papillary muscles play no role at all in opening and closing of the valve. They serve to generate systolic pressure in the isovolumetric condition by pulling on the membranes, and to prevent inversion of the valves into the atrium in systole.
- 38. THE AORTIC VALVE
- 39. THE AORTIC VALVE • composed of three leaflets • attach at their base in a semilunar manner to the aortic wall • not muscularized • moves passively according to changes in blood flow and pressure
- 40. THE AORTIC VALVE During diastole, left ventricular pressure is less than the pressure in the aorta, and the leaflets coapt at their tips to close the valve and prevent retrograde flow During systole, the pressure gradient drops to zero and the leaflets relax, allowing the valve to open
- 41. THE AORTIC VALVE • The leaflets must withstand substantial backpressure of 80 mmHg in normotensive individuals and more than 100 mmHg in hypertensive individuals, resulting in the leaflets stretching 10% in the circumferential direction and as much as 30% in the radial direction, with values of circumferential mechanical stress in the range of 300–600 kPa. • Movement of the blood into the aorta creates high oscillatory shear stress varying between –5 and 7 Pa on the ventricular side of the leaflet, while the aortic side experiences lower shear stress peaking at 2 Pa, with flows that are generally thought to be more disturbed and complex.
- 42. Aortic Valve Diseases • Aortic Stenosis • the narrowing of the AV opening during systole • producing an obstruction of the left ventricular outflow • caused by a congenital abnormality of the valve or by progressive calcification • elevated pressures in the left ventricle during systole • left ventricular wall thickens
- 43. Aortic Valve Diseases • Aortic Insufficiency (aortic regurgitation) • the valve does not close completely in diastole • Allowing blood to flow in the reverse direction (leak) • Causes might be, aortic dilatation, congenital abnormality of the valve, and calcification etc. • The blood reflux from the aorta into the left ventricle increases the ventricular workload through pressure and volume overloads • these overloads trigger a hypertrophic dilatation of the left ventricle
- 44. Aortic Valve Diseases • Aortic Valve Malformations • represent different cases of congenital malformations involving various numbers of cusps, from one to five • Some of these cusps can be fused with a raphe (the conjoined area between two underdeveloped cusps that turns into a malformed commissure) • complete or incomplete fusions of the cusps fusion of two anatomical cusps into a functional cusp with a raphe (in brown)
- 45. Aortic Valve Diseases • Aortic Valve Malformations
- 46. Three-dimensional illustration of a type 1 bicuspid aortic valve
- 47. Failure Mechanisms of the Aortic Valve with Aortic Insufficiency • Classifications of AI failure mechanisms have been proposed to provide cardiac surgeons with a better understanding of the diseased AV and help them guide the approach to be used for treatment. • Because stenotic valves cannot usually be surgically repaired (they need to be replaced instead), more efforts have been devoted to regurgitant AVs. Existing classifications are generally based on the distinction between two underlying causes for AI, issues with the aortic root, and issues with the cusps.
- 48. Failure Mechanisms of the Aortic Valve with Aortic Insufficiency
- 49. Mitral Valve • A medical view cross-section of the mitral valve is shown in figure.
- 50. Mitral Valve • The mitral valve are composed of four primary elements. These elements include the valve annulus, the valve leaflets, the papillary muscles, and the chordae tendineae. • The bases of the leaflets form the annulus, which is an elliptical ring of dense collagenous tissue surrounded by muscle. The circumference of the mitral annulus is 8 to 12 cm during ventricular diastole when blood is flowing through the mitral valve from the left atrium to the left ventricle. • During ventricular systole the mitral valve closes and the circumference of the mitral annulus is smaller.
- 51. A superior view of a mitral valve
- 52. Mitral Valve • The mitral valve is a bicuspid valve and has an aortic (or anterior) leaflet and a mural (or posterior) leaflet. • Because of the oblique position of the valve, strictly speaking neither leaflet is anterior or posterior. The aortic leaflet occupies about a third of the annular circumference and the mural leaflet is long and narrow and lines the remainder of the circumference. • When the valve is closed the view of the valve from the atrium resembles a smile. Each end of the closure line is referred to as a commissure.
- 53. Mitral Valve • Each leaflet is composed of collagen reinforced endothelium. Striated muscle, nerves fiber, and blood vessels are also present in the mitral valve. Muscle fibers are usually present on the aortic leaflet but rarely on the mural leaflet. • The aortic (anterior) leaflet is slightly larger than the mural (posterior) leaflet. The combined surface of both leaflets is approximately twice the area of the mitral orifice, allowing for a large area of coaptation permitting effective valve sealing.
- 54. Mitral Valve • The chordae tendineae for both leaflets attach to the papillary muscle. Chordae tendineae consist of an inner core of collagen surrounded by loosely meshed elastin and collagen fibers with an outer layer of endothelial cells. • There is an average of about 12 primary chordae tendineae attached to each papillary muscle. The anterolateral and the posteromedial papillary muscle attach to the ventricular wall and tether the mitral valve into place. • The chordae tendineae prevent the mitral valve from inverting through the annular ring and into the atrium. That is, in normal physiologic situations they prevent mitral valve prolapse. Improper tethering results in prolapse and mitral regurgitation.
- 55. Mitral Valve • Stresses in mitral valve leaflets of up to 0.22 MPa have been estimated when the left ventricular pressure reaches up to 150 mmHg during ventricular systole. • Mitral velocity flow curves show a peak in the curve during early filling. This is known as an E wave. Peak velocities are typically 50 to 80 cm/s at the mitral annulus. A second velocity peak occurs during the atrial systole and is known as an A wave.
- 56. Mitral Valve • In healthy individuals, velocities in the A wave are lower than the velocities during the E wave. • Diastolic filling of the ventricle shows a peak inflow during diastolic filling followed by a second peak during atrial systole.
- 57. Mitral Valve Failure • Chordae tendineae rupture and papillary muscle paralysis can be consequences of a heart attack. • This can lead to bulging of the valve, excessive backward leakage into the atria (regurgitation), and even valve prolapse. • Valve prolapse is the condition under which the valve inverts backward into the atrium. Because of these valve problems, the ventricle does not fill efficiently. • Significant further damage, and even death, can occur within the first 24 h after a heart attack because of this problem.
- 59. Anatomy of the Arterial bed Mean Radius of Various Arteries
- 60. Arterial Radius related to Age The radius and wall thickness of human arteries for young ( Y) and old (0) persons
- 61. Modulus of Elasticity related to Age (a) Thoracia aorta (b) Iliac artery Incremental modulus of elasticity of arteries of normal young and old persons at a pressure of 100 mm Hg
- 62. Vascular Branching Mother Branch Daughter Branch
- 63. Pulsatile Blood Flow • In pulsatile blood flow the transient inertial force term may become important when compared with the viscous force term. • To make an estimate, let U = a characteristic velocity, ω = a characteristic frequency, and L = a characteristic length. • This is a dimensionless number. If it is large, the transient inertial force dominates. If it is small, the viscous force dominates.
- 64. Pulsatile Blood Flow • The dimensionless number ωL2/ν is a frequency parameter, and is called the Stokes' number because its significance was pointed out by George Stokes in 1840. It is better known by its square root, • which is called Womersley number in honor of J. R. Womersley, who made extensive calculations on pulsatile blood flow in 1950s. If L is taken to be the radius of the blood vessel, then Womersley's number is often written as α:
- 65. Pulsatile Blood Flow • The ratio of the radius of the tube to the wall layer thickness (δ) is • if α is large , the effect of the viscosity of the fluid does not propagate very far from the wall and pulsatile flow will be relatively blunt, in contrast to the parabolic profile of the Poiseuillean flow, which is determined by the balance of viscous and pressure forces.
- 66. Womersley's number The theoretical velocity profiles computed for a straight circular cylindrical tube in which a sinusoidally oscillating pressure gradient acts. As (α increases from 3.34 to 6.67, the profiles are seen to become flatter and flatter in the central portion of the tube.
- 67. Pressure and Blood velocity patterns
- 68. Transient motion velocity changing with time • a recording of blood velocity of a single patient
- 69. Transient motion velocity changing with time • an ensemble average of many experiments
- 70. Transient motion velocity changing with time • a sample of turbulence velocity of a single patient
- 71. Transient motion velocity changing with time • the root-mean-square of the turbulence velocity, or the so-called turbulence intensity
- 73. Blood Flow Model • Since the pioneering work of Otto Frank in 1899, there have been many types of mathematical models of blood flow. • The aim of these models is a better understanding of the biofluid mechanics in cardiovascular systems. • Raines et al. in 1972 observed that patients with severe vascular disease have pressure waveforms that are markedly different from those in healthy persons. • By developing a model that would predict which changes in parameters affect those pressure waveforms in what way, the scientists might provide a means for diagnosing vascular disease before it becomes severe.
- 74. Electrical Analog Model of Flow in a Tube • The electrical schematic of a circuit representing a length of artery, terminating in a capillary bed. • The values for resistance, capacitance, and inductance for each resistor, capacitor, and inductor, respectively, are calculated from the blood vessel properties on a per unit length basis.
- 75. • For this type of discretized model, the resistance in each discrete resistor can be written as • The inductance in the vessel for each discrete inductor element becomes • The capacitance of the vessel is the compliance of the vessel, or dA/dP, and depends on the pressure at the point where the capacitor is located. Electrical Analog Model of Flow in a Tube
- 76. Modelling of Flow through the Mitral Valve • Assessment of ventricular function and quantification of valve stenosis and mitral regurgitation are important in clinical practice as well as in physiological research. • Noninvasive assessment of diastolic function that does not require the use of intracardiac pressure has been an important goal, and in recent years, Doppler electrocardiography has become the “diagnostic modality of choice” to assess diastolic function. • The goal of the research that created this model was development and validation of a mathematical model of flow through the mitral valve during early diastolic ventricular filling.
- 77. Modelling of Flow through the Mitral Valve • The model of early ventricular filling, or the E-wave portion of a single heartbeat, begins at the time when pressures are equal in the atrium and the ventricle, i.e., it begins from the instant of mitral valve opening. • The model then describes flow and pressures during ventricular filling up to the point of atrial systole.
- 78. Modelling of Flow through the Mitral Valve • A schematic of the atrium and ventricle with the mitral valve in-between. Afluid cylinder of length L is shown.
- 79. Modelling of Flow through the Mitral Valve • Rv, Rc, M, Ca, Cv are described in greater detail in the text following. • The first differential equation describing flow rate through the mitral valve is shown below.
- 80. Modelling of Flow through the Mitral Valve • The second differential equation is written as follows: • where Ca represents atrial compliance in m5/N (m3/N/m2). The pressure inside the atrium is related to its volume through atrial compliance. Ca = d(volume)/dt. • The volume is also related to flow rate. In one sense, the flow intro the atrium determines its final volume and therefore the final atrial pressure.
- 81. Modelling of Flow through the Mitral Valve • Similarly, the third equation describing the system is the equation for change in ventricular pressure with time. The ventricular pressure is similarly related to the ventricular volume and the ventricular compliance, Cv. The change in pressure of the ventricle is also related to “active relaxation.” • In all three equations, q represent flow rate in m3/s, dq/dt represents the time rate of change of flow rate in m3/s2, Pa represents left atrial pressure in N/m2, Pv represents left ventricular pressure in N/m2, and M represents the inertance term, which is analogous to inductance in the electrical circuit and has the units of kg/m4.
- 83. TYPES OF PROSTHETIC VALVES
- 84. CAGED BALL VALVE • Early mechanical prosthetic heart valves were ball valves. In 1952, Dr. Charles Hufnagel implanted the first ball and cage valve into a patient with aortic valve insufficiency. • Although the design of mechanical prosthetic valves has progressed significantly over the past 50 years, ball and cage valves are still the valve of choice by some surgeons.
- 85. CAGED BALL VALVE • The first artificial heart valve was the caged- ball, which utilizes a metal cage to house a silicone elastomer ball. • When blood pressure in the chamber of the heart exceeds that of the pressure on the outside of the chamber the ball is pushed against the cage and allows blood to flow. • At the completion of the heart's contraction, the pressure inside the chamber drops and is lower than beyond the valve, so the ball moves back against the base of the valve forming a seal.
- 86. CAGED BALL VALVE
- 87. CAGED BALL VALVE • Advantages • Oldest prosthetic valve. • Durabilty upto 40 yr • Disadvantages • High profile • Hemolysis • High thrombogenecity • Poor hemodynamics in small sizes • Unique features • Occluder travels completely out of the orifice, reduces thrombus & pannus growing from the sewing ring. • Continuously changing points of contact of the ball reduces the wear & tear in any one area • Thrombogenic risk 4-6% per year.
- 88. TILTING DISC VALVE • Björk-Shiley designed the first tilting disk, or single leaflet, valve around 1969. Those valves used a tilting disk occluder that was held in place by a retaining strut. • However, the development of the bileaflet valve by St. Jude in 1978, has led to the predominance of this type of bileaflet valve in the mechanical valve market.
- 89. TILTING DISC VALVE • Tilting disk valves have a single circular occluder controlled by a metal strut. • They are made of a metal ring covered by an PTFE- coated high translucency (ePTFE) fabric, into which the suture threads are stitched in order to hold the valve in place. • The metal ring holds, by means of two metal supports, a disc which opens and closes as the heart pumps blood through the valve. • The disc is usually made of an extremely hard carbon material (pyrolytic carbon), in order to allow the valve to function for years without wearing out.
- 91. TILTING DISC VALVE • Advantages • Low profile • Good hemodynamics even in small sizes • Excellent durability • Permit central laminar flow. • Disadvantages • Anticoagulation mandatory • Higher risk of thrombosis than cage ball • Sudden catastrophic valve thrombosis.
- 92. BILEAFLET VALVES • They have two semicircular leaflets retained within the ring by hinges. The potential for impeded leaflet movement due to interference with cardiac structures is slim, as the open leaflets are positioned in the middle of the blood stream and enclosed within the ring in the closed position. • Bileaflet valves are the most protected as the leaflets hardly protrude from the valve ring, even during maximum opening.
- 93. BILEAFLET VALVES
- 94. BILEAFLET VALVES • Advantages:- • Low bulk - flat profile. • Less thrombogenicy. • Central laminar flow. • Two semicircular discs that pivot between open and closed positions. • No need for supporting struts. • Good hemodynamics even in small sizes. • 2 lateral, 1 central minor orifice , no chance of sudden catastro thrombosis. • Disadvantages:- • Anticoagulation mandatory risk of thrombosis.
- 95. TISSUE (BIOLOGICAL) HEART VALVES • Tissue valves (also called biologic or bioprosthetic valves) are made of human or animal tissue. Some valves may have some artificial parts to help give the valve support and to aid placement. • Once the tissue is removed from the animal, it is chemically treated to preserve the tissue and prevent immulogic reactions once it is placed in a patient. • There are three types of tissue valves: • pig tissue (porcine), • cow tissue (bovine), and • human (allografts or homografts).
- 96. Porcine Stented valves • The porcine stented valve was the first generation of porcine tissue valves. They have been available for more than 30 years. • The valves are made from natural porcine aortic valves, but may be used for aortic or mitral valve replacement. They are trimmed and then fixed in buffered glutaraldehyde at high pressure.
- 97. Porcine stentless valve • The porcine stentless valve is used for aortic valve replacement. The valve is made from a natural porcine aortic valve and is fixed in buffered glutaraldehyde solution at a low pressure. • No stents or synthetic sewing rings are used. Therefore, these valves are very similar to the homograft valve. • These valves are technically more difficult to implant but are useful in patients with small hypertrophied hearts.
- 98. Pericardial valves The Carpentier-Edwards PERIMOUNT Pericardial Bioprosthesis • Pericardial valves include the Perimount series valves (Edwards LifeSciences). Ionescu-Shiley pericardial valves have been discontinued. • More recently, stentless porcine valves have been used. • They offer improved hemodynamics with a decreased transvalvular pressure gradient when compared with older stented models.
- 99. Other types of biological valves • Xenografts are tissue valves (eg, bioprostheses, heterografts); most are from pigs (porcine), but valves from cows (bovine) may also be used. Their viability is 7 to 10 years. • They do not generate thrombi, thereby eliminating the need for long-term anticoagulation.
- 100. Other types of biological valves • Homografts, or allografts (ie, human valves), are obtained from cadaver tissue donations. • The aortic valve and a portion of the aorta or the pulmonic valve and a portion of the pulmonary artery are harvested and stored cryogenically. • Homografts are not always available and are very expensive.
- 101. Other types of biological valves • Autografts (ie, autologous valves) are obtained by excising the patient’s own pulmonic valve and a portion of the pulmonary artery for use as the aortic valve. • Anticoagulation is unnecessary because the valve is the patient’s own tissue and is not thrombogenic. • The autograft is an alternative for children (it may grow as the child grows), women of childbearing age, young adults, patients with a history of peptic ulcer disease, and those who cannot tolerate anticoagulation.
- 102. Testing of Valves
- 103. Radiologic Identification • Starr-Edwards caged ball valve : • Radiopaque base ring • Radiopaque cage • Three struts for the aortic valve; 4 struts for the mitral or tricuspid valve
- 104. Cinefluoroscopy • Structural integrity • Motion of the disc or poppet • Excessive tilt ("rocking") of the base ring - partial dehiscence of the valve • Aortic valve prosthesis Fluoroscopy of a normally functioning CarboMedics bileaflet prosthesis in mitral position A=opening angle B=closing angle
- 105. MRI • Not useful in assessing prosthetic-valve structure • Used only when prosthetic-valve regurgitation or para valvular leakage is suspected but not adequately visualized by echocardiography
- 106. Cardiac Catheterization • Measure the transvalvular pressure gradient, from which the EOA can be calculated • Can visualize and quantify valvular or paravalvular regurgitation
- 107. Echocardiography of Stentless Aortic Homografts • Doppler flow characteristics similar to native valve. • Only 2-D evidence: Increased Echo intensity, and Thickness of aortic annulus.
- 109. Valve dysfunction
- 110. Patient-prosthesis mismatch • When the effective prosthetic valve area, after insertion into the patient less than that of a normal valve (Rahimtoola in 1978) • Effective Orifice Area (EOA) indexed to Body Surface Area (BSA) is less than 0.85 cm2/m2 • EOA (echo) differs from geometric orifice area (measured directly) • EOA for each prostheses type & size obtained in literature from pts normally functioning prostheses • Average if > 1 value • mild (0.9 - 1 cm² /m² • moderate (0.6 - 0.9 cm2/m² • severe (iEOA < 0.6cm²/m² (Rahimtoola)
- 111. Three-step algorithm • Step 1: Calculation of the patient BSA. • Step 2: Reference to the specific table for identification of the adequate valvular EOA according to the patient BSA. • Step 3: Selection of the most appropriate type and size of valve prosthesis according to the target iEOA
- 112. Valve thrombosis
- 113. Valve thrombosis • Incidence of 0.1 to 5.7 % per patient/year <0.2% per year for mechanical valves <0.1% bioprosthetic valves • small thrombus, at the hinge portion of a bileaflet valve → obstruct the mechanism • tilting disk -- a much larger thrombus to prevent function • Ball and cage valves – less susceptible → occluder has no contact at all with the valve housing for a portion of every cycle • Clinical • Non obstructive- incidental/embolic phenomenon • Partial obstruction- dyspnea,systemic embolism , fever • Severe obstruction- overt heart failure
- 114. Fibrinolytic therapy • Rt sided thrombosis 80-100% success rate • Surgery for fibrinolysis failure/symptoms > 3 wk • Surgery – Lt sided thrombosis, large clot burden
- 115. Embolization • Cerebral embolization → CT normal/infarct → warf & heparin – 72 hrs APTT lower therapeutic level → till the desired INR • Anticoagulantion delayed for at least 7 to 14 days - ICH, extensive cerebral infarction → OAC
- 116. Paravalvular Regurgitation • Mild or moderate paravalvular leakage – asymptomatic, may have only a mild haemolytic anemia. • can be observed carefully with serial echo • Severe paravalvular leakage - usually have symptoms of heart failure or severe anemia. • should be treated with surgical repair or replacement of the valve
- 117. THANK YOU