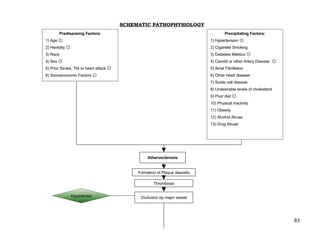
Schematic Pathophysiology Cva
- 1. SCHEMATIC PATHOPHYSIOLOGY Predisposing Factors: Precipitating Factors: 1) Age ۞ 1) Hypertension ۞ 2) Heredity ۞ 2) Cigarette Smoking 3) Race 3) Diabetes Meliitus ۞ 4) Sex ۞ 4) Carotid or other Artery Disease ۞ 5) Prior Stroke, TIA or heart attack ۞ 5) Atrial Fibrillation 6) Socioeconomic Factors ۞ 6) Other heart disease 7) Sickle cell disease 8) Undesirable levels of cholesterol 9) Poor diet ۞ 10) Physical inactivity 11) Obesity 12) Alcohol Abuse 13) Drug Abuse Atherosclerosis Formation of Plaque deposits Thrombosis Hypertensio Occlusion by major vessel 83
- 2. If managed: If not managed Actual: Possible: Dx: Dx: PET scan, MRI, Lysed or moved thrombus Cranial CT scan (6/16/08) cerebral angiography, from the vessel Capsuloganglionic bleed lumbar puncture, EEG/ Lacunar infarct, ECG, skull x-ray, Bilateral Internal Carotid carotid ultrasonography Ateriosclerosis Vascular wall becomes Doppler (6/16/08) TX: aspirin within 24 weakened and fragile Mean flow velocities and hrs, thrombolytics within pulsatility index of both 3 hours, carotid anterior and posterior stenting, hypothermia, circulation within normal Leaking of blood from the anticoagulants, surgical limits fragile vessel wall decompression (hemicraniectomy), EEG/ECG, skull x-ray, carotid endartectomy carotid ultrasonography Guarded Prognosis Cerebral Hemorrhage Sx:, headache, unconsciousness, If managed: If not managed nausea/vomiting, Dx: CT scan, MRI, cerebral angiography, visual disturbances arteriography, lumbar puncture, skull x-ray Tx: chronic hypertensives, surgical decompression, evacuation and aspiration, administration of fresh frozen plasma with Mass of blood forms and fibrinogen or cryoprecipitate grows Decreased Hematoma evacuation ICP 84 Formation of cavity surrounded by dense gliosis
- 3. > 60 ml < 30 ml 30-60 ml hemorrhage hemorrhage hemorrhage Intermediate Poor prognosis Good prognosis prognosis Vasospasm of tissue and arteries Blood seeps into the Formation of small ventricles and large clots CEREBRAL HYPOPERFUSION Sx: dizziness, Obstruction of CSF confusion, passageway headache Impaired distribution of oxygen and glucose Accumulation of CSF in the ventricles Tissue hypoxia and cellular starvation Ventricles dilate behind Lodges unto the point of obstruction Cerebral Ischemia other cerebral arteries Increased ICP Initiation of ischemic cascade If not managed If managed: Ventriculostomy, VP shunt, ICP Anaerobic metabolism by Monitoring mitochondria Alternative route Unrelieved Production of oxygen free for return of CSF obstruction radicals and other reactive in the circulation Generates large amounts of Failure production of oxygen species lactic acid adenosine triphosphatase Compression of Guarded brain tissues will Failure of energy dependent Metabolic Acidosis Prognosis not occur process 85 (ion pumping)
- 4. Release of excitatory Damage to the blood vessel neurotransmitter glutamate endothelium Influx of calcium Failure of Activates enzymes that mitochondria digest cell proteins, lipids and nuclear material Further energy depletion Transient Ischemic Attack If not managed If managed: -t-PA (urokinase, streptokinase) Brain sustains an irreversible -calcium channel cerebral damage blockers Release of metalloprotrease (zinc and calcium-dependent enzymes) Guarded Prognosis Break down of collagen, hyaluronic acid and other elements of connective tissue Structural integrity loss of brain tissue and blood vessels Breakdown of the protective Blood Brain Barrier 86
- 5. Cerebral edema Vascular Congestion Compression of tissue Increased intracranial pressure Impaired perfusion and function Middle Anterior cerebral Posterior CerebraI Internal Carotid Vertebrobasilar Anteroinferior Posteroinferior Cerebral Artery artery Artery Artery System Cerebellar cerebellar Lateral Frontal Lobe Occipital lobe; Branches into Cerebellum and Cerebellum Cerebellum hemisphere, anterior and ophthalmic, PCA, brain stem frontal, parietal medial portion of anterior choroidal, and temporal temporal lobe ACA, MCA lobes, basal ganglia 87
- 6. Sx: Sx: Sx: Sx: Sx: Sx: Sx: Ipsilateral contralateral Contralateral Contralateral Mild Ataxia, Alternating ataxia, facial hemiparesis hemiparesis or hemiparesis, contralateral paralysis of the motor paralysis, with facial hemiplegia, foot and leg hemiparesis, larynx and soft weaknesses, ipsilateral loss asymmetry, unilateral deficits greater intention palate, ataxic gait, of sensation in contralateral neglect, altered than the arm, tremor, diffuse ipsilateral loss dysmetria, face, sensation sensory consciousness foot drop, gait sensory loss, of sensation in contralateral changes on alterations, , homonymous disturbances, pupillary face, hemisensory trunk and homonymous hemianopsia, contralateral dysfunction, contralateral on impairments, limbs, hemianopsia, inability to turn hemisensory loss of body, double vision, nystagmus, ipsilateral eyes toward alterations, conjugate nystagmus, homonymous Horner’s periods of affected side, deviation of gaze, dysarthria, hemianopsia, syndrome, blindness, vision changes, eyes toward nystagmus, Horner’s nystagmus, tinnitus, aphasia if dyslexia, affected side, loss of depth syndrome, conjugate hearing loss dominant dysgraphia, expressive perception, hiccups and gaze, paralysis, hemisphere is aphasia, aphasia, cortical coughing, dysarthria, involved, Mild agnosia, confusion, blindness, vertigo, nausea memory loss, Horner’s memory deficits, amnesia, flat homonymous and vomiting disorientation, syndrome, vomiting affect, apathy, hemianopsia, drop attacks, carotid bruits shortened perseveration, tinnitus, attention span, dyslexia, hearing loss, loss of mental memory vertigo, acuity, apraxia, deficits, visual dysphagia, incontinence hallucinations coma 88
- 7. If not managed: If managed: Palliative care- Frequent vital sign and neurovital signs, intubation, mechanical Continued insufficiency of blood ventilation, vasodilators, osmotic diuretics, flow ventriculostomy, ICP monitoring Further compression of tissues Poor cerebral perfusion Coma Poor improvement Cerebral Death Poor Prognosis Loss of neural feedback mechanisms Cessation of physiologic functions 89
- 8. Pulmonary Other systems GUT Cardiovascular GIT System System Relaxation of Sx: restlessness, intestines and Loss of cardiac Relaxation of abnormal sphincters thermoregulation, muscle function venous valves mental confusion, increased secretions, decreased urinary output. Sx: Sx: bradycardi hypotension Loss of bowel Failure of accessory Loss of lung control Decreased muscles for breathing movement Neurogenic bladder Loss of sphincter cardiac output control Sx: apnea Cardiopulmonary arrest Systemic Failure 90 DEATH
