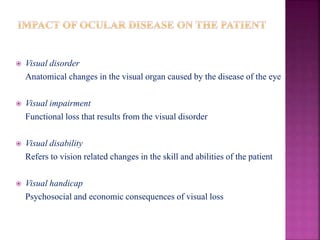
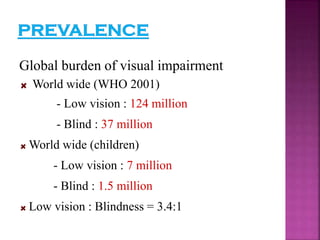
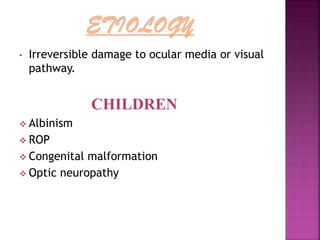
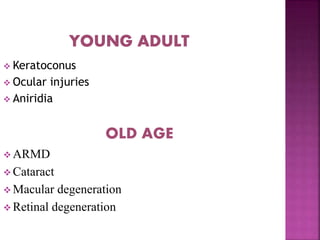
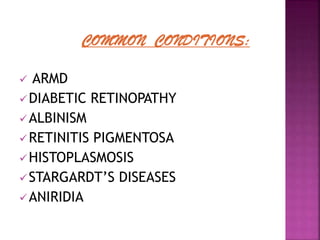
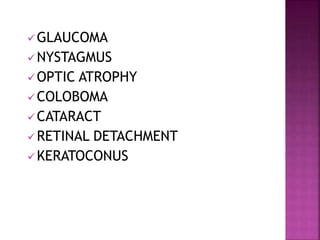
This document discusses low vision and provides definitions, classifications, common causes, and management strategies.
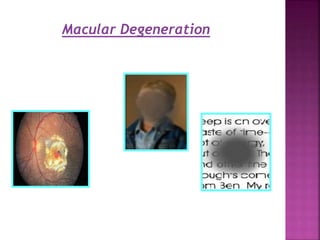
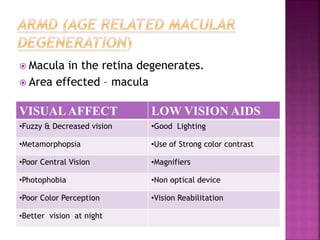
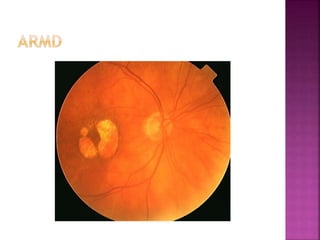
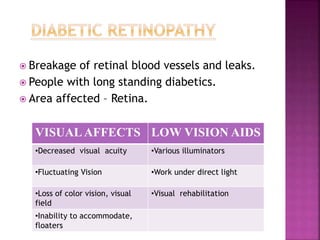
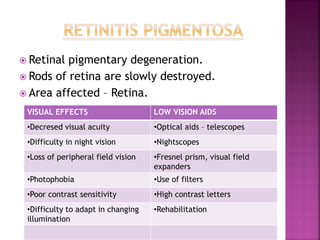
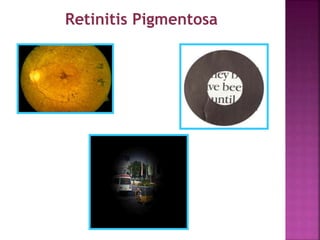
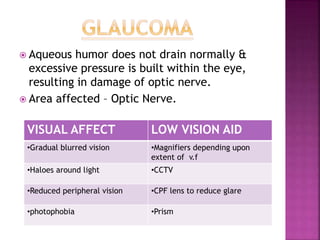
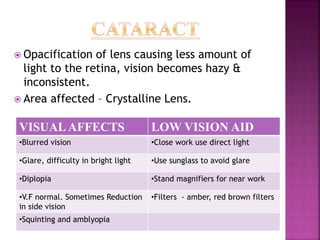
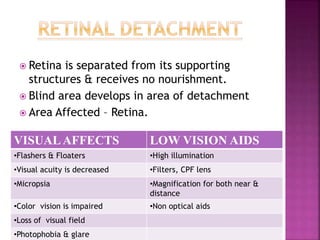
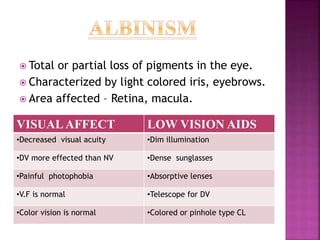
[1] Low vision is defined as visual impairment even after treatment that results in visual acuity worse than 6/18 but ability to use vision. It can be caused by conditions like macular degeneration, retinitis pigmentosa, cataract, and glaucoma.
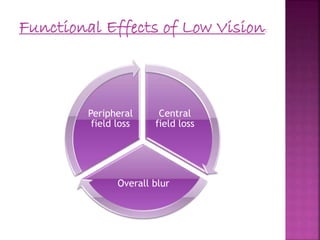
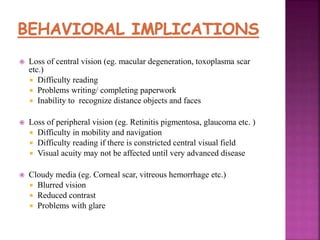
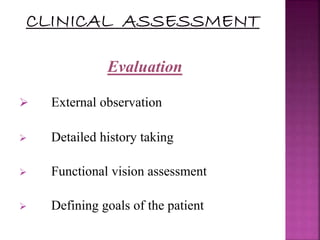
[2] Low vision affects people's ability to perform visual tasks and can cause blurry or decreased vision, loss of peripheral vision, and light sensitivity. Evaluation involves assessing vision and goals, while management includes low vision devices and counseling.
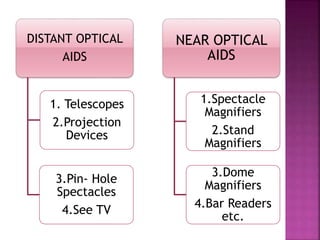
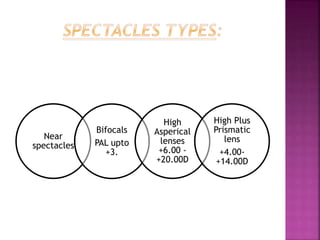
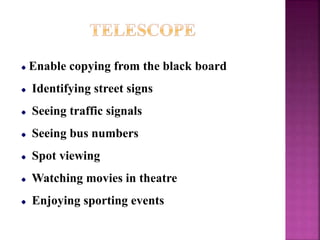
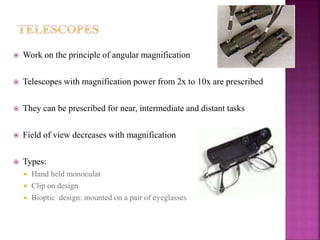
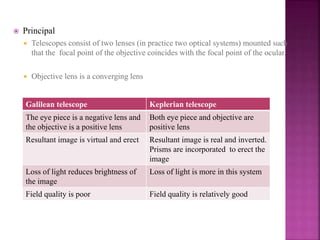
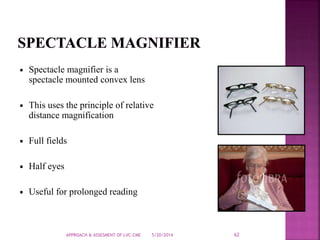
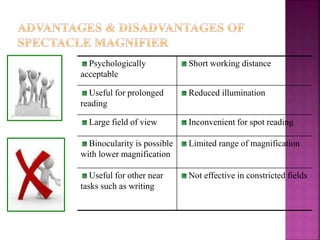
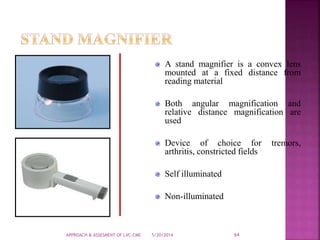
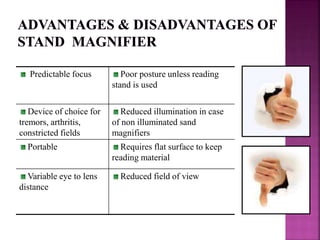
[3] Common low vision devices include telescopes, magnifiers, and electronic


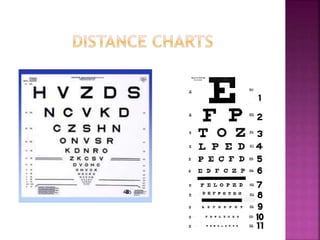
![Material required: Variable distance Log MAR
chart [ Bailey Lovie/ETDRS chart] for distance.
Continuous text or word reading chart for near
Setup: Normal room illumination
Start with better eye first
Allow change in head posture, eccentric viewing,
head movements etc.
Check monocular visual acuity followed by
binocular](https://image.slidesharecdn.com/lowvision-140520092803-phpapp02/85/Low-vision-35-320.jpg)

![Low vision device:
It is a device that enables the patient to
improve his/her residual visual performance & helps to
attain functional vision for the particular task of
concern.
Categories of LVD:
a] Optical
b] Non optical
c] Electronic
d] Assistive devices](https://image.slidesharecdn.com/lowvision-140520092803-phpapp02/85/Low-vision-46-320.jpg)



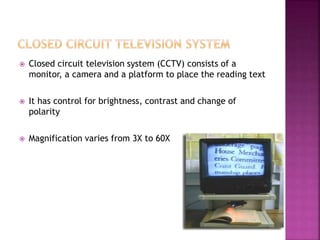

![Closed circuit television
[CCTV]
Monitor CCTV Portable CCTV Mouse model
CCTV](https://image.slidesharecdn.com/lowvision-140520092803-phpapp02/85/Low-vision-81-320.jpg)