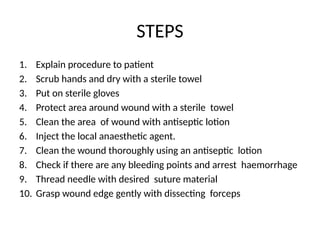
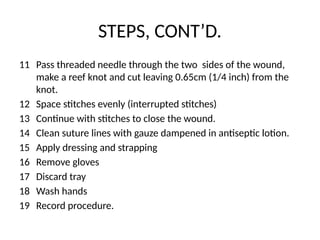
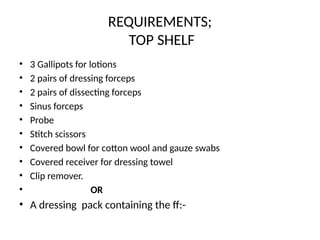
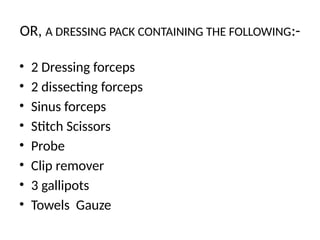
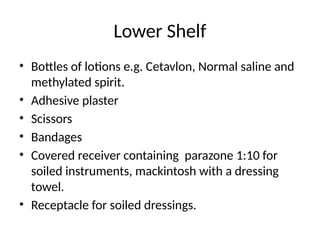
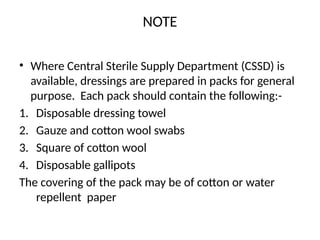
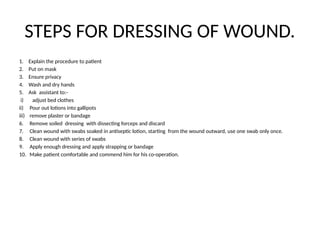
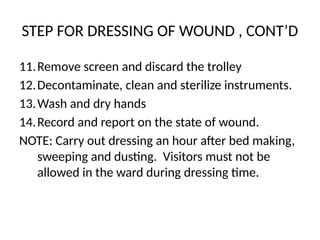
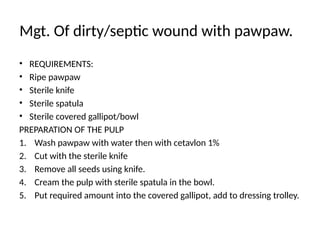
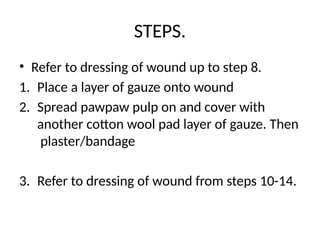
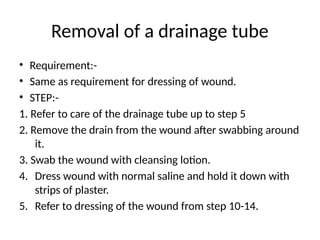
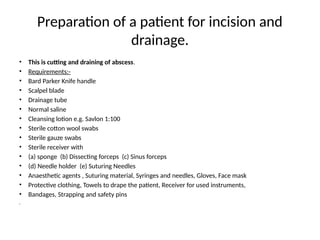
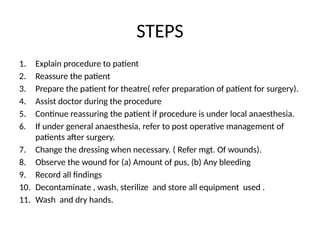
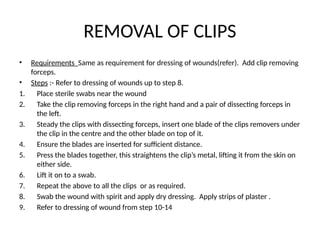
The document outlines the procedures for suturing minor wounds and dressing them, detailing the necessary materials, preparation steps, and techniques for effective wound management. Additionally, it includes information on the management of dirty or septic wounds using natural substances like pawpaw and honey, as well as the importance of surgical drains and their care. The document emphasizes cleanliness and proper techniques to ensure effective healing and minimize infection risks.