Eric Benjamin submitted his final project on malaria in Nigeria to Walden University. The 3 sentence summary is:
The project focused on malaria in Nigeria, where it is a major public health problem, with an estimated 100 million cases and 300,000 deaths per year. Malaria disproportionately affects children under 5 and the poor, and factors like poverty, lack of education, and cultural beliefs contribute to the high burden. Nigeria has implemented strategies like insecticide-treated bed nets and indoor residual spraying, as well as policies to improve prevention, treatment, and the public health system's response to malaria.

![2
Final Project Component1: Introduction
Malaria is a life-threatening blood disease that is characterized by intermittent and remittent fever and
anemia, jaundice, splenomegaly and hypoglycemia in severe cases.Malaria is caused by a protozoan
parasite that invades human red blood cells, and can be transmitted from one person to another by
mosquitoes. Among the four kinds of malaria parasites (p. ovale, p. vivax, p. malariae and p. falciparum)
that infect humans, Plasmodium falciparum most often result in severe infection that may lead to death if
not promptly treated (Markle, Fisher & Smego, 2014).
There are certain factors that must be present for the parasite to complete its life cycle depending on the
species of mosquito involved. For instance, the tropical climate in the sub-Saharan Africa regions
particularly Nigeria is highly favorable to the Anopheles species. The human host and breeding sites
(stagnant waters and tropical forests) are also common factors that have warranted malaria to be endemic
in Africa (Markle, et al. 2014). As a result, the focus of this project would be Nigeria because malaria is
the major public health problem coupled with the weak public health system (The Presidential Malaria
Initiative [PMI], 2014).
In the global context, the estimated number of malaria cases in Nigeria is 100 million with about 300,000
deaths per year. Thus making Nigeria the most populous nation with about 2.6% estimated annual growth
rate in a total population of approximately 172 million in Africa. The mortality rate resulting from malaria
is very high compared to that of HIV/AIDS (215,000). Also, about 65% of Nigerians live in poverty,
hence making it difficult to combat malaria efficiently. The burden of malaria placed Nigeria as the 17th
PMI country in 2010, and $43.6 and $43.2 million were received in 2011 and 2012 respectively as an aid
to combat the disease (PMI,2014). Because malaria is preventable and treatable, the burden can be
eliminated.](https://image.slidesharecdn.com/236ed2a4-78d3-484b-848b-b41ec657f255-161015182747/85/WK11ProjBenjaminE-2-320.jpg)
![3
Health Indicators
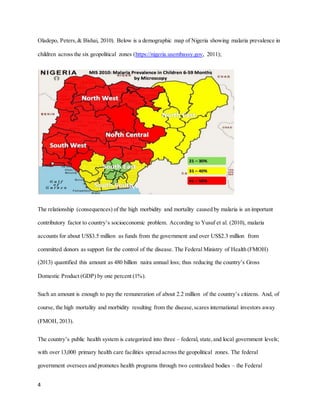
Nigeria is divided into 36 states and a centralized capital city – Abuja. The states are further grouped into
six geopolitical zones – North Central, North East, North West,South-South, and South West. There are
774 constitutionally recognized local government areas that are unevenly distributed across the states
(Federal Ministry of Health [FMOH], 2013).
Nigeria is considered one of the most populous countries in Africa with over 160 million people. The
morbidity rate resulting from malaria infection is approximately 90 percent of the total population, and
mortality rate of 207,000 each year. Due to this high figure, Nigeria is ranked as the country with the
highest burden of malaria in the sub-Saharan Africa (Noland, Graves, Sallau, Eigege, Emukah,
Patterson…& Richards,2014). The country’s geographic setting and climate is suitable for the breeding
of the Anopheles mosquito; thus making it a malaria-endemic region. However,the distribution of the
health indicators mentioned above varies considerably according to the six geopolitical zones. For
instance, in a cross-sectional study between two northern states – Sokoto and Bauchi; it was found that
malaria infection among children below the age five were high relatively high (Millar, McCutcheon,
Coakley, Brieger, Ibrahim, Mohammed, ….& Sambisa, 2014).
In another cross-sectionalstudy, high morbidity and mortality due to malaria was observed among
children at the same age level – below five (Odu, Mitchell, Isa, Ugot, Yusuf, Cockroft,…. & Anderson,
2015). The observed differences in the disease distribution among the children below age five were
related to socioeconomic status. For instance, the examined northern states experienced a shortage of
essential malaria supplies and limited access to the health facility (Millar, et al. 2014). But in the South
East– Cross River, mothers were less likely to seek treatment for affected children even when health
facilities were available (Odu et al. (2015). Also, in a study based on multilevel analysis, the prevalence
of malaria was found to be higher in the rural environment than in the urban setting (Yusuf, Adeoye,](https://image.slidesharecdn.com/236ed2a4-78d3-484b-848b-b41ec657f255-161015182747/85/WK11ProjBenjaminE-3-320.jpg)
![5
Ministry of Health (FMOH) and the National Primary Health Care Development Agency. Unfortunately,
the health facilities are not evenly distributed among the 36 states owing to weak economy and
corruption. The existing health facilities lack proper coordination and skilled manpower (The Presidential
Malaria Initiative [PMI], 2014).
The inefficiency of the health system has also contributed to the incidence of malaria in the country. For
example, the lack of health facilities in a majority of the rural areas can lead to self-medication with
unhygienic locally made herbs; and even death from acute infection. Shortage of well-trained health
professionals and ill-equipped primary health care centers can result in inadequate diagnosis and
treatment. Poor logistic and inadequate coordination between the primary care facilities and the FMOH
leads in inequitable distribution of malaria supplies. As a consequence the intervention measures become
ineffective; including the MDG6 goal – combating HIV/AIDS,malaria and other diseases (PMI,2014).
The reasons for the setback mentioned above in combating the disease is poor economy exacerbated by –
large population, drug resistance,and insecurity as well as civil unrest (PMI, 2014).
Health Determinants
Among African nations, Nigeria is faced with the highest malaria burden (51 million cases and a
mortality of 207,000) every year. Also, of the 160 million populations, about 97% are prone to
Plasmodium infection. In spite of intervention strategies adopted to curb the menace,malaria has
remained critical to public health (Noland, Graves, Sallau, Eigege, Emukah, Patterson & Richards, 2014).
The burden of malaria can be attributed to severalcauses such as – socio-cultural, economic and
environmental factors. Non-compliance with the use of mosquito treated nets is an example of a socio-
cultural factor. Eteng, Mitchell, Garba, Ana, Liman, Cockroft, & Anderson (2014), found in their research
that the fear of adverse effect and discomfort associated with the use of treated net; as well as poorly
ventilated apartments were some given reasons by participants for not using the treated bed net.](https://image.slidesharecdn.com/236ed2a4-78d3-484b-848b-b41ec657f255-161015182747/85/WK11ProjBenjaminE-5-320.jpg)