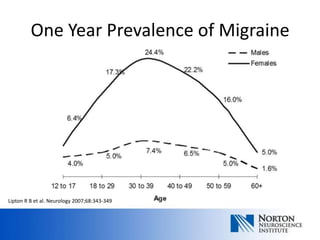
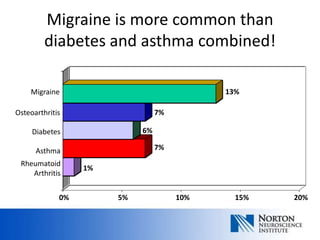
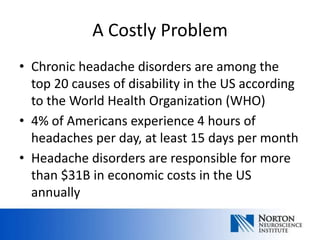
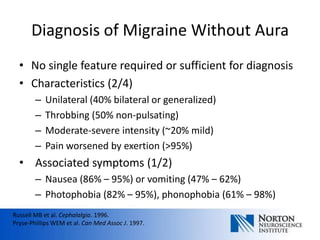
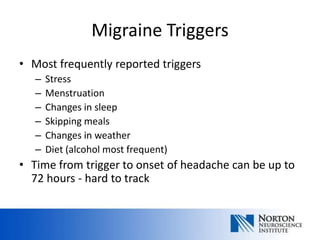
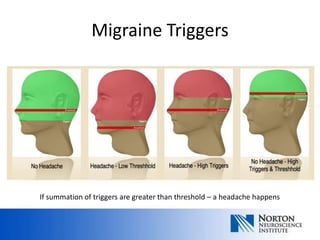
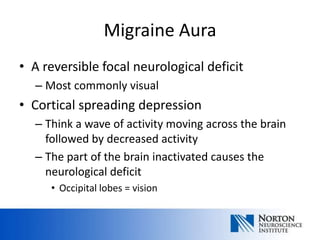
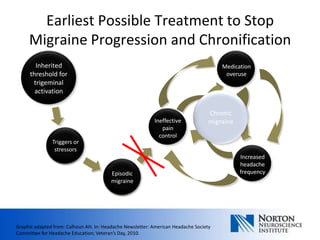
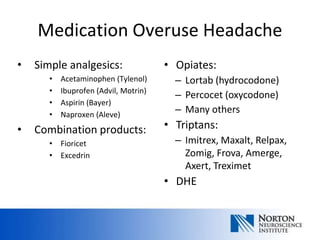
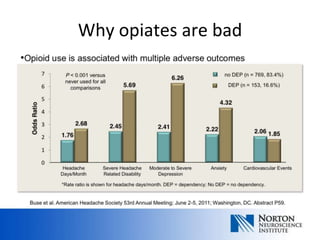
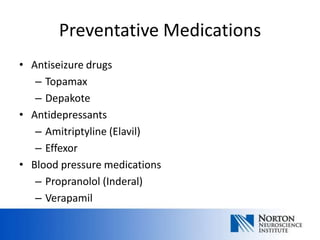
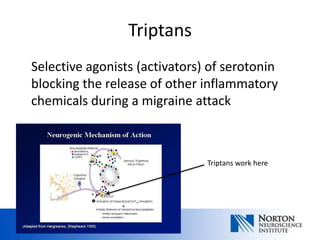
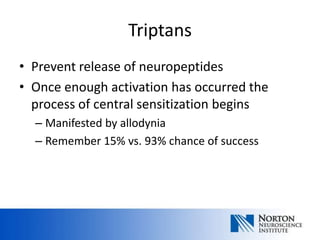
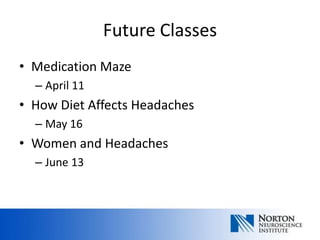
Headache School provides education to help patients better manage migraine. Migraine is a very common neurological disorder that affects over 30 million Americans. Formal educational programs have been shown to produce better outcomes for patients with headache. The classes cover topics like different medication options, how diet can impact headaches, and headaches in women. Understanding the science behind migraine can help patients identify triggers to prevent attacks and choose effective treatment options.