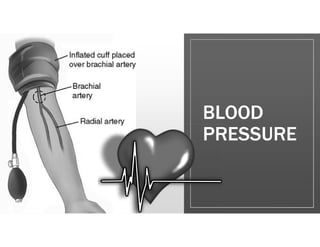
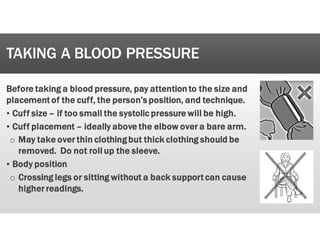
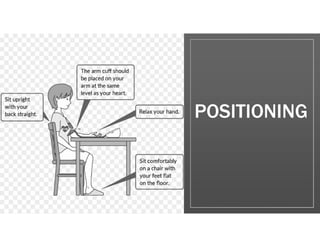
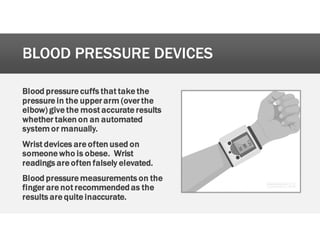
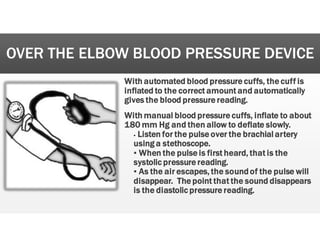
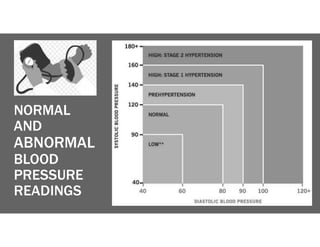
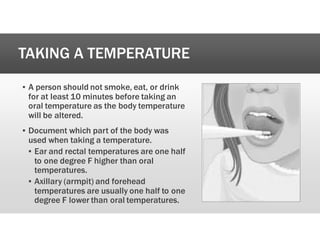
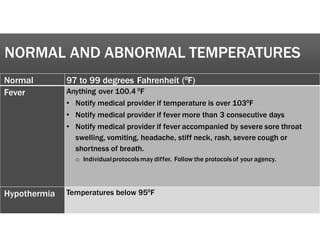
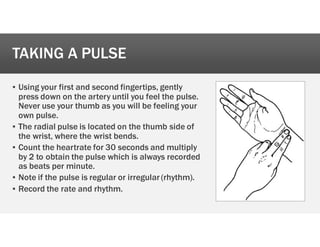
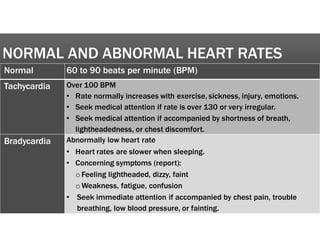
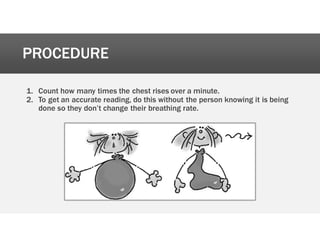
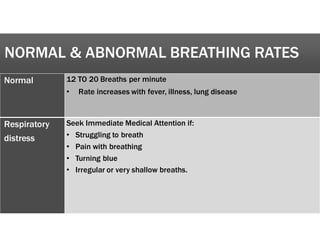
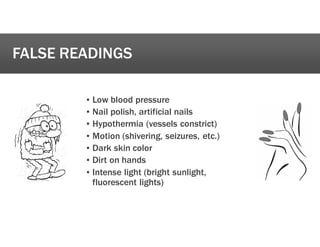
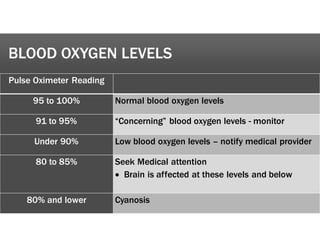
The document outlines the procedures and protocols for assessing vital signs, including blood pressure, temperature, heart rate, respiration rate, and oxygen saturation. It details the methods for accurately measuring these vital signs, the normal and abnormal ranges, and when to notify medical providers. Each client should have specific written protocols regarding these assessments to ensure proper care.