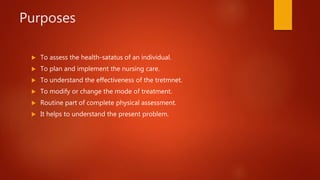
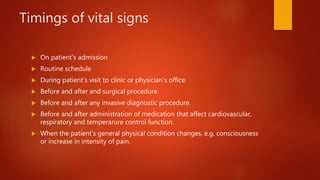
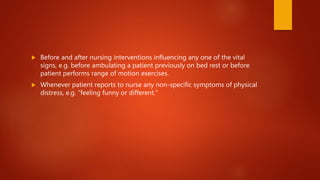
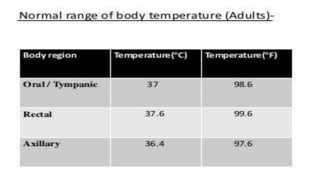
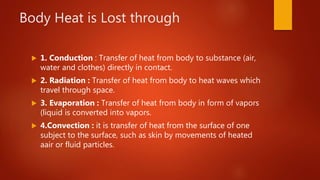
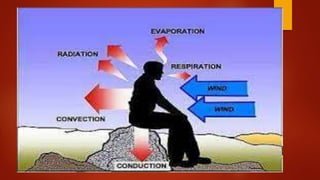
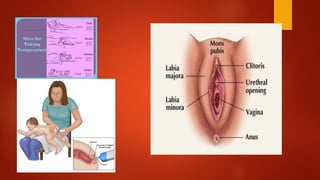
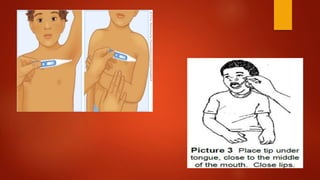
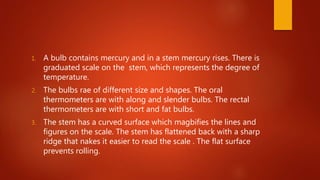
The document discusses vital signs and taking body temperature measurements. It defines vital signs as body temperature, pulse, respiration, and blood pressure, which reflect the body's vital functions. Taking accurate vital sign measurements is important for assessing a patient's health status, planning care, understanding treatment effectiveness, and modifying treatment as needed. The document provides details on different methods and sites for measuring body temperature, factors that influence temperature regulation, and guidelines for properly taking and documenting temperature readings.