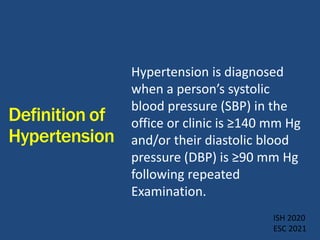
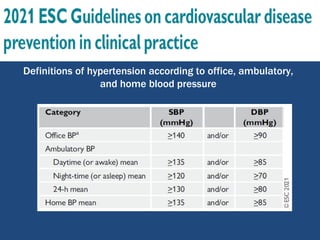
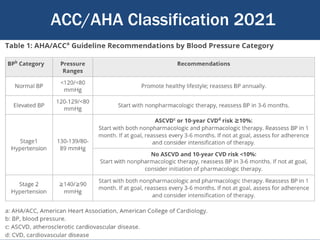
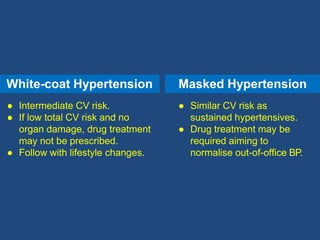
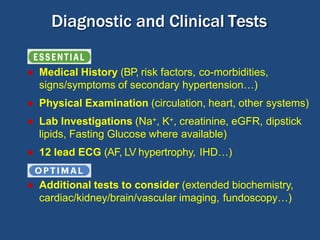
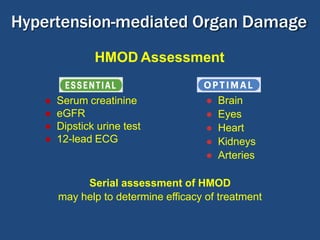
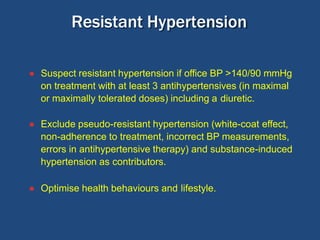
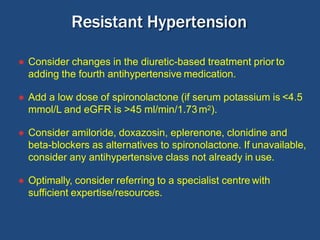
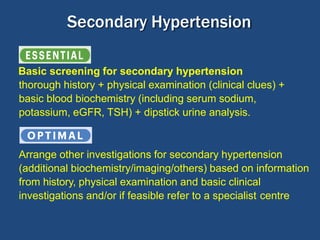
This document summarizes updates on hypertension from the 2020 guidelines of the International Society of Hypertension. It discusses the definition and classification of hypertension based on office blood pressure measurements. It also covers diagnostic tests, hypertension-mediated organ damage, treatment including lifestyle changes and drug treatment, resistant hypertension, secondary hypertension, and hypertensive emergencies. The guidelines provide guidance on screening, assessing, and managing these hypertension-related conditions and circumstances.