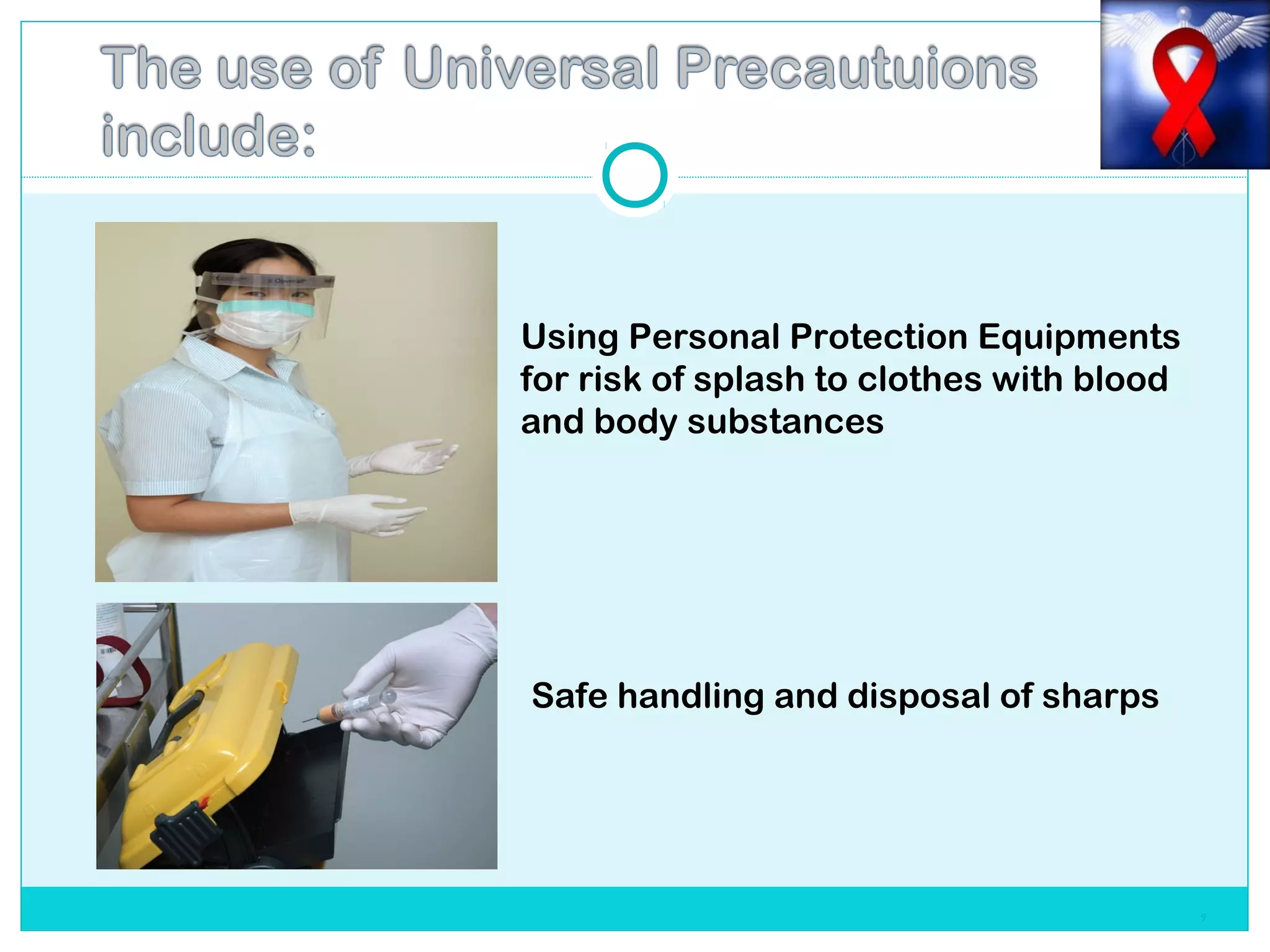
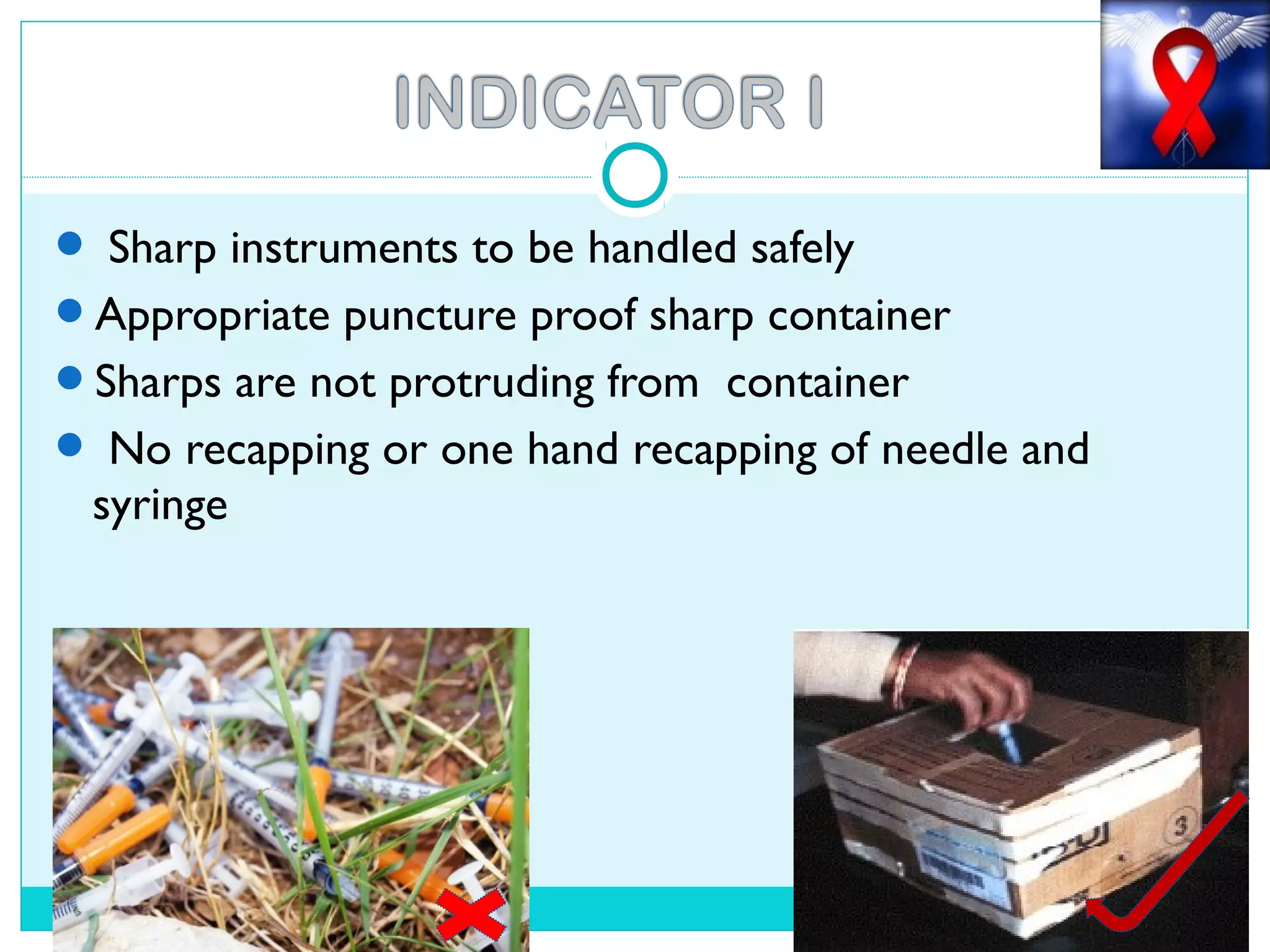
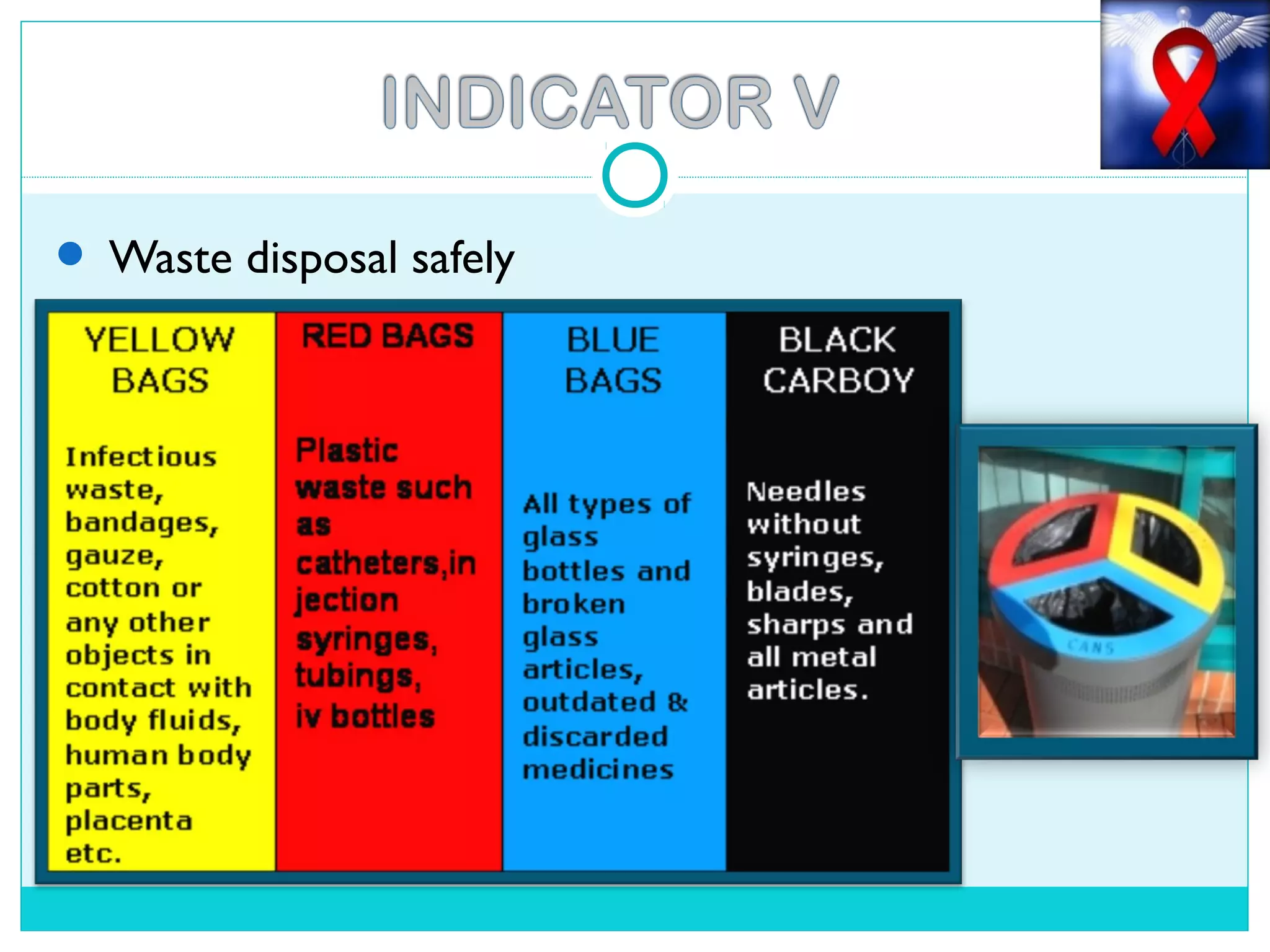
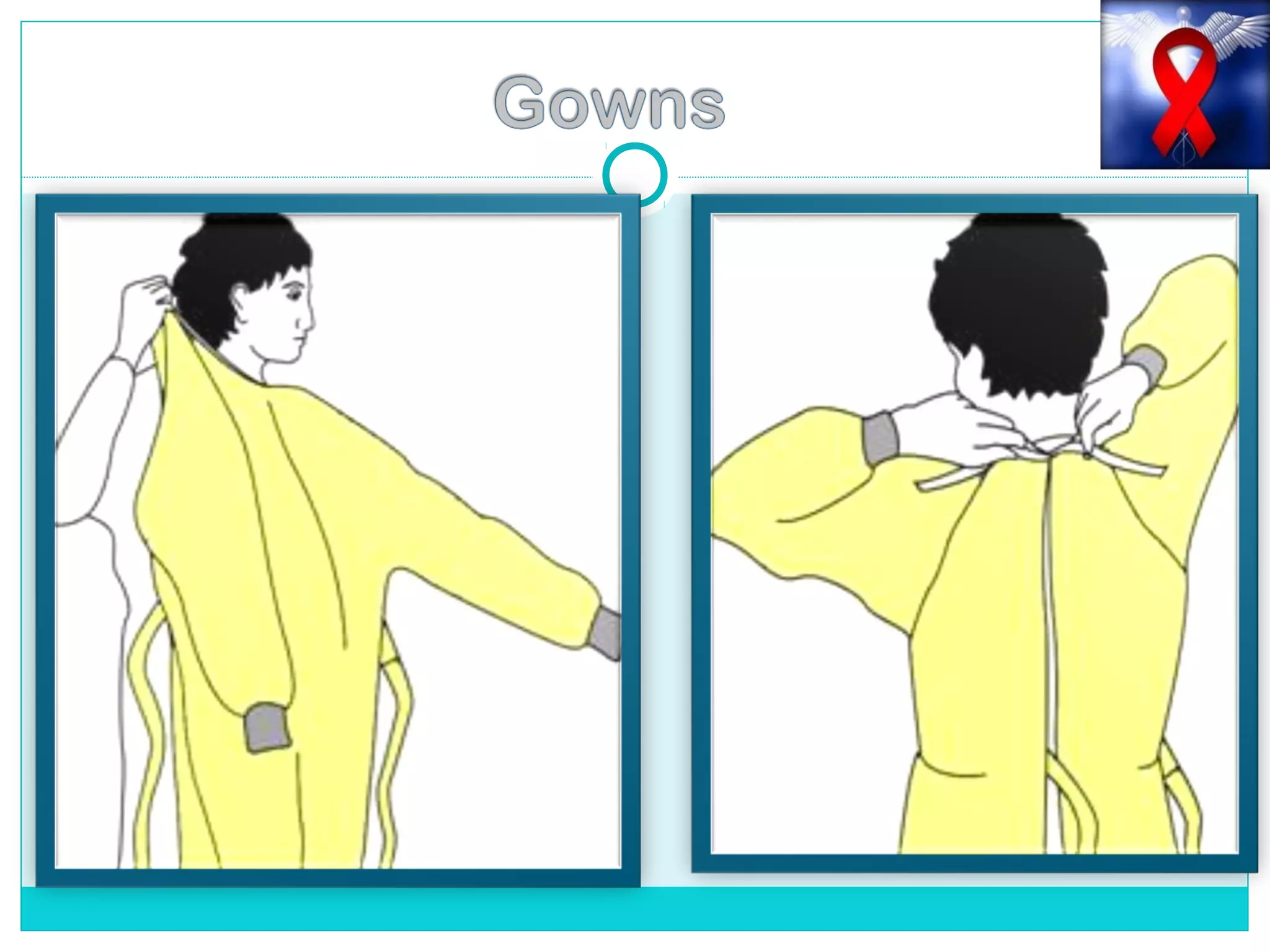
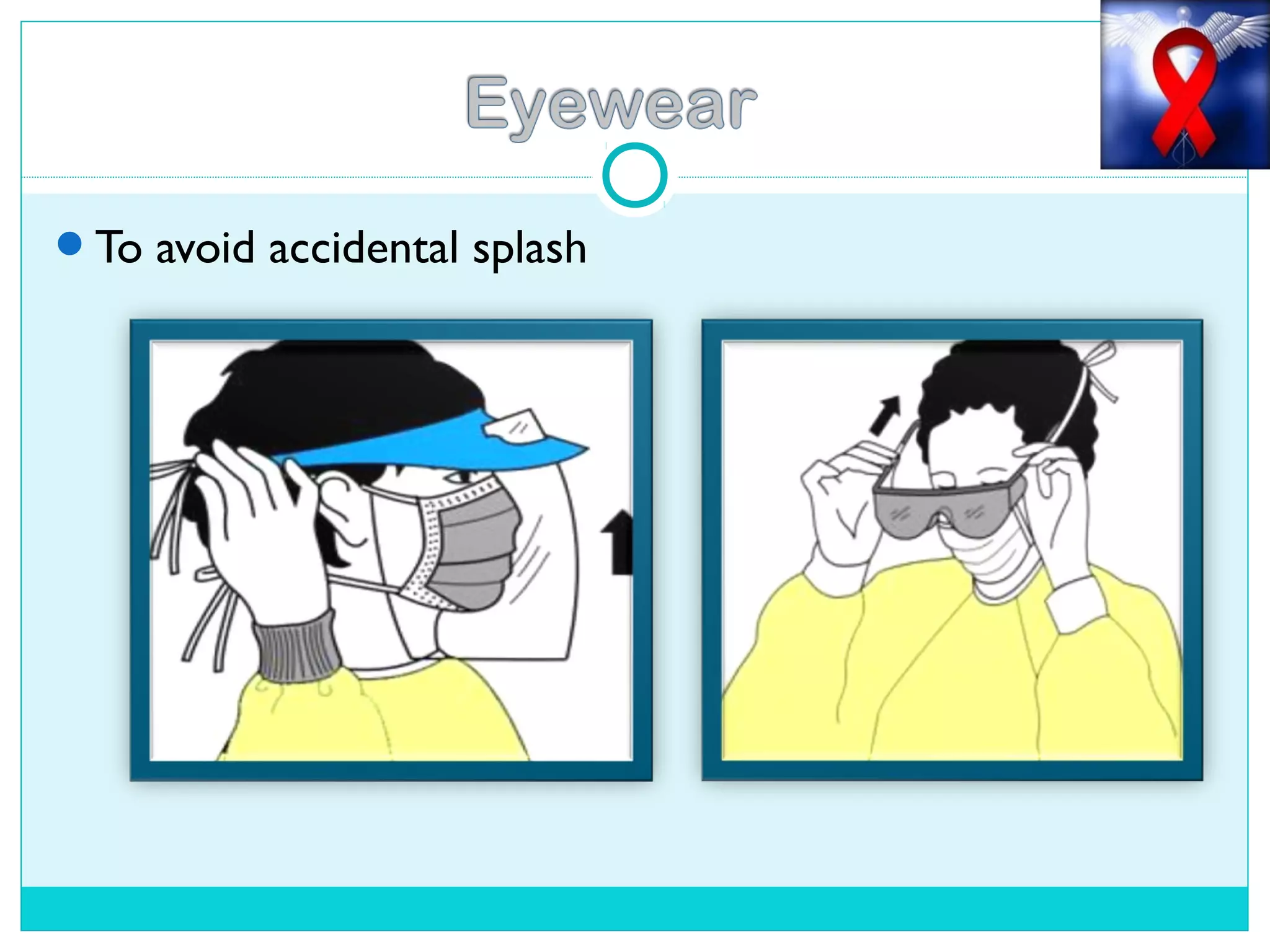
Universal precautions refer to practices that should be followed by all healthcare workers to prevent exposure to infectious diseases. They include hand washing, safe disposal of needles and other sharps, wearing protective equipment like gloves when handling bodily fluids, and cleaning and disinfecting equipment. Universal precautions are important because all patients should be treated as potentially infectious and they help minimize the risk of spreading diseases in healthcare settings.